There are currently four stages of this disease:

- Osteoarthritis of the big toe
- Joint-sparing surgery for minor trauma
- Causes and mechanism of hallux valgus formation
- Diagnosis of hallux valgus
- Treatment tactics for a stiff big toe
- Clinical observations
- Rehabilitation after surgery
- Cost of Hallux Rigidus treatment
- What is hallux valgus grade 1
- Treatment of hallux valgus grade 1
- ,Hello!' – Network of the Clinic for Spinal and Joint Health
- symptoms
- The 'Halo! – Network of spine and joint clinics
- Bursitis of the metatarsal
- Inflammation of the metatarsophalangeal joint of the big toe
- Bursitis of the heel
- Causes of the disease:
- The treatment:
Osteoarthritis of the big toe
Osteoarthritis of the big toe joint or hallux rigidus is defined by doctors as degeneration and destruction of the big toe joint. Hallux rigidus develops as a result of a long-term, progressive deforming joint disease of the big toe joint.
The disease is manifested by severe stiffness, deformation of the big toe and pain when walking.
The triggering factor for the development of osteoarthritis can be trauma to the joint, constant stress on the joint or a systemic disease. Sometimes the cause of osteoarthritis cannot be determined.
Hallux rigidus is characterized by restricted movement of the first toe as a result of arthritic changes. Normal dorsiflexion of the thumb is about 50-60 degrees, while hallux rigidus reduces the range of motion to 5-15 degrees. These movements are associated with significant pain. Hallux rigidus leads to complete immobilization of the thumb.
Hallux rigidus is the second most common disease of the big toe. First and foremost is the valgus deformity of the thumb, the hallux valgus. Statistically, one in forty-five people over the age of fifty suffers from hallux rigidus. Both feet are often affected at the same time, especially in rheumatoid arthritis and gout.
Researchers have identified several causes for the development of hallux rigidus. The most common is inflammation and detachment of the articular cartilage in the big toe following trauma or in association with a rheumatic disease. Hallux rigidus can occur as a complication after surgery to correct a thumb misalignment (hallux valgus).
The metatarsophalangeal joint consists of the first metatarsal bone and the main phalanx of the thumb.

Like any other joint in the body, it is covered with articular cartilage.
The articular cartilage covers the ends of the bones and is very smooth, shiny, and whitish in color.
Joint-sparing surgery for minor trauma
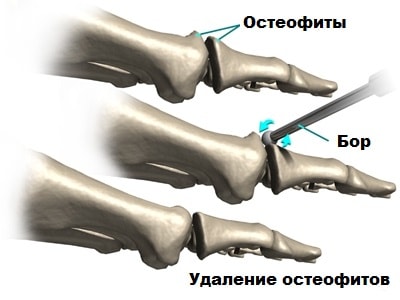
In some cases, exostoses, or growths around the joint, prevent the finger from flexing. These growths cause problems with walking and prevent the thumb from pushing off the ground normally when walking.
Healectomy is a joint-preserving surgery that removes the bony growths around the joint, especially in the upper part of the joint, thereby increasing mobility and reducing pain.
It is also supplemented by an osteotomy of the first metatarsal bone to reduce the pressure of the articular surfaces against each other. The aim of the operation is to shorten the first metatarsal bone, thereby reducing the pressure of the metatarsal bone on the big toe and therefore also the pain.
After shortening, the bone is fixed in its new position using intra-articular screws. This procedure is more commonly performed on younger patients when there is a chance of extending the life of the joint.

Causes and mechanism of hallux valgus formation
The main cause of the development of the deformity is usually connective tissue weakness, which can manifest itself as transverse flat feet, excessive joint mobility, varus, stretching of ligaments, fascia and skin. There is a hereditary predisposition - as a rule, the patient's closest relatives (mothers or grandmothers) also have this deformity. Other factors such as high heels, walking in uncomfortable, tight or short shoes are secondary and only contribute to hallux valgus. The second group of causes of hallux valgus are congenital malformations, foot injuries and a number of diseases in which the neuronal control of the lower leg and foot muscles is disturbed (e.g. poliomyelitis). In addition to ligament weakness, uneven tension in the muscles that guide the first toe back and forth and a genetic tendency to form an exostosis on the inside of the head of the first metatarsal bone play a role in the development of the disease. As the deformity progresses, the imbalance in muscle tone worsens and the metatarsophalangeal joint becomes unstable. The inner surface of the joint is constantly irritated by contact with footwear, causing the head of the metatarsal bone to shift and a bony protrusion to form, further aggravating the deformity. The change in shape of the foot results in a redistribution of loads - the area of the heads of the third and second metatarsals is constantly overloaded when walking. This leads to pain and osteoarthritis not only in the first, but also in the second and third metatarsophalangeal joints.
Patients complain of pain in the area of the first metatarsophalangeal joint. The pain increases after walking or standing for long periods of time and eases with rest. Pain at night may occur, especially after heavy weight bearing on the foot. The pain syndrome can vary widely in its severity and severity, from discomfort (usually in the early stages) to severe burning or persistent, excruciating pain. The severity of the pain is not always clearly related to the size of the deformity, although symptoms are usually more pronounced when the head of the first metatarsal bone is significantly displaced. As the deformity progresses, the foot increasingly loses its normal shape, it becomes wider and flatter, the first toe 'lies' on top of the second toe, and there are often accompanying deformities of the second toe. Combined with a 'bump' in the projection of the metatarsophalangeal joint of the big toe, this has a significant impact on the appearance of the foot. In addition to pain, cosmetic defects and problems with shoe fitting are often the reason why patients visit traumatologists and orthopedists. Young women in particular often complain about this. On visual inspection the foot is flat. Deformation and mild to moderate congestion are visible in the projection of the first metatarsophalangeal joint. The first toe is tilted outward and at an angle to the others. Palpation is painless or slightly painful, with bony exostosis and thickening of the skin on the inside of the foot in the area of the metatarsophalangeal joint. Mild local swelling may be present. Movement in the I metatarsophalangeal joint is usually restricted (the degree of restriction can vary widely), and maximum extension of the I toe can cause pain.
Diagnosis of hallux valgus
The diagnosis of hallux valgus is made based on the symptoms and x-ray findings. An x-ray of the first metatarsophalangeal joint of the big toe is taken. For a more accurate assessment of the pathology of the adjacent anatomical structures, if necessary, radiographs of the 2nd and 3rd metatarsals are also taken. The degree of hallux valgus is determined by two measurements: the angle between the 2nd and 1st metatarsal bones (intermetatarsal angle) and the angle, in which the first toe in relation to the 1st degree of hallux valgus:
- 1 degree.– Less than 12 degrees between the metatarsals, the deviation angle of the 1st toe is less than 25 degrees.
- grade 2– Angle between the metatarsals less than 18 degrees, the deviation angle of the 1st toe is greater than 25 degrees.
- grade 3– Angle between the metatarsals greater than 18 degrees, deflection angle of the 1st toe greater than 35 degrees.
In addition to the degree of deformation, the severity of the arthritic changes is also assessed using x-rays. The presence of osteoarthritis is indicated by joint narrowing, deformation of the joint bed, marginal hypertrophy and osteosclerosis of the subchondral area. In some cases, an MRI or CT scan may be performed to more accurately assess pathological changes in the foot. The MRI examination of the foot is used to examine the soft tissues, the CT examination of the foot is used to examine the bony structures. In the case of diseases that are associated with impaired nerve control of the muscles, consultation with a neurologist is necessary.
Treatment tactics for a stiff big toe
First of all, it is advisable to reduce the load on the foot as much as possible. Therefore, avoid long walking, wear comfortable shoes and use insoles.
Your doctor may prescribe topical or systemic nonsteroidal anti-inflammatory drugs to relieve pain. If these remain ineffective, glucocorticosteroid blockades are indicated.
Physiotherapeutic treatments complement the treatment plan. So, in 2018, researchers from Evpatoria published a work proving the effectiveness of magnetic therapy in combination with diadynamics in the treatment of osteoarthritis.
In addition, massages and therapeutic gymnastics can also be prescribed.
In severe cases, surgical intervention is required. 'Arthrodesis is considered the gold standard treatment for big toe stiffness, in which the joint surfaces are removed and the bones are fused together.
Clinical observations
Operations using the AMIC® technique on the metatarsophalangeal joint of the big toe have been actively carried out in Germany since 2016 (particularly in the Rummelsberg and ATOS clinics).
The results of chondroplasty of the first metatarsophalangeal joint in 20 patients over a period of 24 months have now been examined and described in detail. By the end of follow-up, no patient complaints or situations requiring revision surgery were identified.
In Moscow led a team of specialists from the Nasonova Scientific Research Institute of Rheumatology and Orthopedics. Moscow carried out a series of procedures for plastic surgery of the first metatarsophalangeal joint using the AMIC technique with the Chondro-Gide matrix.
The severity of the patients' joint pain, which was quite high before the operation, decreased significantly by the third month of follow-up, and by the sixth month it had almost completely disappeared.
However, what distinguishes Chondro-Gide from the aforementioned methods of metatarsophalangeal joint plastic surgery is the fact that. The mobility of the joint was almost completely restored by the 12th month of the follow-up examination – to an average of 70 % of the physiological norm (up to a maximum of 80 %).
In this way, patients have a real chance to avoid a disabling operation and maintain the natural function of your joints.
Rehabilitation after surgery
From the 14th to the 20th day, a postoperative VALGO shoe, designed in Italy specifically for ankle surgery, is worn.
A bandage is applied on days 14 to 20. The postoperative dressing is removed.
As soon as the bandage is in place, the most important phase of treatment begins – rehabilitation. To this end:
- Physiotherapy and physical therapy are prescribed;
- Injections of plasma (PRP therapy) and prosthetic synovial fluid are continued to facilitate sliding in the joint.
Such a health problem can be effectively addressed by contacting the doctors in our clinic in a timely manner. We look forward to your visit and remind you that free telephone consultations are offered for patients from other cities.
Cost of Hallux Rigidus treatment
The final cost of the operation will be determined during the consultation and will depend on the following factors:
- the stage of osteoarthritis and the degree of deformation of the foot;
- the extent of the operation (whether 2, 3 or more toes are affected), etc.
- Operating surgeon
The operation for osteoarthritis of the first metatarsophalangeal joint takes 15-20 minutes. You can walk again immediately after the operation.
- Member of the Italian Medical Order
- Member of the Italian Society of Orthopedic Traumatology (SIOT)
- Member of ALOTO (Association of Orthopedic Traumatologists of Lazio)
- Member of the Society for Rehabilitation (SIMFER)
- Active member of the Society for Foot Surgery (SISPEC)
What is hallux valgus grade 1
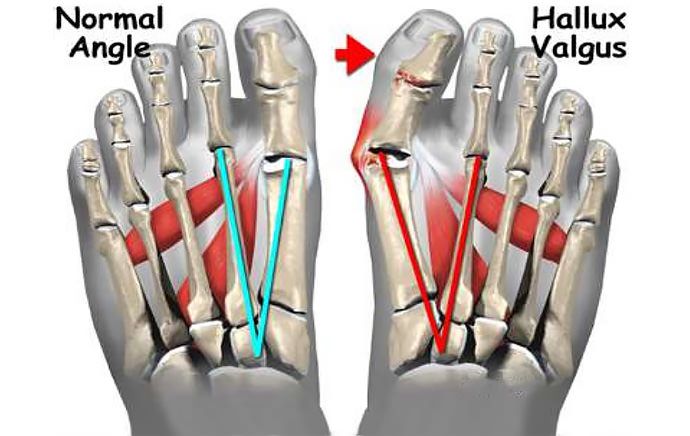
Hallux valgus is an outward deviation of the big toe, whereby the bulge that forms at the base of the toe is nothing other than the medial side of the metatarsal head. If the cause of the misalignment persists, the thumb deviates further into the resting position, the first metatarsal bone retracts further inward, and its head expands to form a bony callus that can withstand constant pressure and friction. However, in stage 1, these changes are barely visible to the naked eye and symptoms such as pain, significant thickening, etc. are not yet present. However, patients may experience fatigue in their legs after a long walk or other physical activity. However, this is often perceived as normal and not taken seriously. This is the insidiousness of the disease and the reason why most patients only see an orthopedist in later stages. Normally, the interdigital angle between the 1st and 2nd metatarsals should not be greater than 10°, and a deviation of the thumb from the 1st. Hallux valgus grade 1 is said to occur if the interdigital angle is greater than 10° but less than 12° and the deviation of the big toe does not exceed 25°. Visually detecting such changes is therefore difficult, if not impossible. Therefore, it is important to undergo an orthopedic examination at least once a year if there are signs of disease progression. In this way, the pathology can be diagnosed at the first stage and measures can be taken to stop its progression and eliminate it. If the disease is left untreated, the deformity will progress and lead to collapse of the first metatarsophalangeal joint. This leads to a significant cosmetic impairment in that not only the big toe but also the neighboring toes are twisted and painful swelling occurs. In addition, the risk of synovitis, arthritis and arthrosis of the affected joints increases dramatically. In later stages, patients have great difficulty walking because they are in constant pain and their shoes no longer fit.
Treatment of hallux valgus grade 1

Treatment of grade 1 hallux valgus is primarily conservative because it does not cause any other pain or discomfort. However, in some cases, minimally invasive surgery may be indicated to achieve optimal results.
Once the diagnosis is confirmed by foot x-rays and plantography results, it is advisable to review living habits and lifestyle. Eliminating the factors that cause metatarsal misalignment is essential for maximum treatment effectiveness.
Therefore, all patients are recommended to be careful when choosing footwear for everyday use and to give preference to orthopedic models with a wide toe box and a comfortable square heel. Such shoes ensure that the load is evenly distributed across the support points of the foot, provided there are no flat feet, and, above all, do not constrict the toes. This helps to stop the progression of pathological changes.

However, that doesn't mean that women with grade 1 hallux valgus have to give up nice shoes with pointed toes and high heels forever. Such shoes can be worn on special occasions, events, etc. but should be avoided in everyday life.
It is recommended not to wear them for more than 2 hours at a time.
Even when treating grade 1 valgus deformity, it is important to normalize weight to reduce the load on the foot. In some cases this can be done with little effort and simply more physical activity; in more severe cases, additional help from a nutritionist may be required. However, strict diets of any kind are not recommended. They are unable to provide all the substances your body needs to function properly. Therefore, such a weight loss option does more harm than good. Always maintain a varied and balanced diet, which is easier to achieve with the help of a qualified nutritionist.
,Hello!' – Network of the Clinic for Spinal and Joint Health
For more than 10 years we have specialized in the treatment of musculoskeletal disorders in various stages of the disease without surgery. ,Hello!' is the clinical base of the country's leading universities, which train specialists for the most sought-after professions in medicine. The clinicians are a team of experts from the PFUR faculty who, together with leading Israeli specialists, have developed unique treatment protocols that meet the standards of the Russian Ministry of Health.
symptoms
Osteoarthritis of the metatarsophalangeal joint of the big toe is initially noticeable through fatigue in the legs, which occurs even with minimal physical activity. Diagnosis is particularly difficult in older people who do not see a doctor and attribute the disease to natural physical changes. As the condition worsens, you may experience difficulty walking, numbness, and an uncomfortable grinding sensation.
The following symptoms also indicate the development of osteoarthritis of the big toe:
- Redness of the skin in the affected area due to hypersensitivity;
Osteoarthritis never goes away on its own, it just gets worse. Therefore, an appointment with an orthopedist or trauma surgeon should be made at the first signs.
The 'Halo! – Network of spine and joint clinics
For more than 10 years we have specialized in the treatment of musculoskeletal disorders in various stages of the disease without surgery. ,Halo!' are the clinical bases of the country's leading universities, training specialists for the most sought-after professions in medicine. The clinics' doctors are a team of experts from the PFUR faculty who, together with leading Israeli specialists, have developed unique treatment protocols in accordance with the standards of the Russian Ministry of Health.
Osteoarthritis is more likely to occur in areas that are exposed to high stress:
- At the base of the toes is the metatarsal bursa.
Bursitis of the metatarsal
The tarsus is the middle part of the foot and consists of five long bones to which the toes are attached. Metatarsal bursitis occurs due to increased stress on one of the bones. The soft tissue between it and the skin is compressed and the bursa initially begins to deform mechanically, followed by inflammation. The symptoms worsen if the affected person walks barefoot on a wooden or tiled floor as the bursa is put under direct strain.
The inflammation can affect the upper part of the toes. The main cause is poor shoes that put a lot of pressure on the joint. The constant friction causes pain, swelling and redness. Wearing shoes becomes torture; even socks can cause discomfort.
Another variant is the interdigital form. The pathology develops when the capsule between the toes is compressed. Main causes of bursitis of the longitudinal arch of the foot:
As we age, the arch of the foot lowers and the metatarsals begin to press on the capsules next to the toes. There is no swelling and the pain spreads to the toes. Comfortable, wide shoes can help relieve the discomfort.
Inflammation of the metatarsophalangeal joint of the big toe
One of the most common forms is capsulitis of the metatarsophalangeal joint at the base of the big toe. There is a large tubercle on the bone, which is subject to increased friction.
The joint becomes deformed, crooked, and the thumb can move to the other finger. The skin thickens and becomes red; Blisters and corns form and pain occurs. Patients have difficulty choosing comfortable footwear; in summer you can wear sandals that do not compress the affected joint capsule.
Bursitis of the heel
- Retrocalcaneal pouch – lies between the calcaneus and the heel and protects the tendon from friction. The bursa becomes inflamed due to thinning of the fat pad.
Causes of the disease:
The main causes of joint destruction are osteoarthritis of various etiologies, rheumatoid arthritis and geriatric arthritis. The cause of this condition may be a disorder of the biomechanics of the foot, a previous inflammatory process in the joint, or an injury to the joint. Hereditary factors should be considered. Premature cartilage degradation and the development of a hallux rigidus are the result of permanent damage to the first toe. Age-related joint changes also play a role - the cartilage tissue becomes thinner over the years.
The most common symptoms are pain and swelling in the joint. The sooner you see a doctor, the greater the chance of long-term joint damage. Conversely, the longer you put pressure on your thumb, the more the metatarsophalangeal joint deforms. An orthopedist will diagnose hallux rigidus after a thorough examination of your foot. For a more accurate and correct diagnosis, an x-ray of the foot should be taken.
The treatment:
Regardless of the degree and stage of the disease, treatment begins with conservative measures. It is mainly symptomatic and aims to reduce pain in the joint. This is done by restricting movement, wearing correct orthopedic footwear (loose, with a low heel and special cushioning insoles), gel toe insoles, non-steroidal anti-inflammatory drugs, foot contrast baths, massages and physiotherapy treatments. Invasive treatments – intra-articular corticosteroid injections – are also used.
In surgical treatment, a distinction is made between joint-preserving procedures such as the removal of bone deposits (cheilectomy) or joint resection and adjustment surgery or arthrodesis (immobilization of the big toe joint). Due to the good long-term results in young, active patients, arthrodesis of the metatarsophalangeal joint is still preferred.
The variable severity of the clinical and radiological manifestations of the disease is a key factor in determining the treatment of the disease.
Read more:- metatarsophalangeal joint.
- Metatarsophalangeal joint of toe 1.
- Stages of hallux valgus.
- chalgus valgus.
- Shapar joint.
- ICD 10 chalgus valgus.
- Deflection of the first toe.
- flatfoot μb.
