MRI offers doctors an excellent opportunity to diagnose complex diseases, such as: b.

- Ultrasound of the lower limbs (final)
- Muscle hernia in ultrasound examination
- CAUSES OF LATERAL LIGAMENT TRENCH
- SYMPTOMS OF COLLATERAL LIGAMENT INJURY
- How does an MRI scan of the ankle work?
- Preparation for the procedure
- Treatment of a tear of the anterior fibula and sagittal joint ligament
- Evaluation
- Example of an MRI image of the ankle joint
- contraindications
- Prevention: tips for prevention
- Possible diseases
- Make an appointment ENT doctor You can make an appointment by phone
- Professional medical help
- Reasons for prescribing surgery
- Folk treatment methods
- Diagnosis of knee pain
- Which doctor can help?
- Our specialists
- fees
Ultrasound of the lower limbs (final)
The anterior talocrural ligament (ATL), one of the most biomechanically important ligaments of the ankle, is also the most commonly injured ligament and is caused by abnormal tension reversal. To identify the ligament, either the extreme distal end of the fibula must be palpated or located in the transverse plane prior to the ultrasound examination. The transducer should then be moved forward and slightly anterior until the fibula and talus are visible. An oblique PTMS may be slightly hypoechoic due to anisotropy, but changing the transducer angle using the heel-toe maneuver should reveal a normal echogenic fiber pattern.
PTMS injuries show similar symptoms to other ligament injuries on lower limb ultrasound. In acute partial ruptures, the ligament is hypoechoic with some intact fibers. In acute full-thickness ruptures, the fibers are discontinuous or absent and are replaced by a heterogeneous hematoma. Rupture fractures can be seen as echogenic foci near the ligament attachment points. Dynamic imaging using the 'anterior drawer test' can help differentiate between partial and complete tears. On ultrasound examination of the lower limbs, movement of the plateau can help visualize intact ligamentous fibers, and asymmetric subluxation of the anterior plateau suggests ligamentous insufficiency. This maneuver is performed with the patient in the supinated position, the probe is placed over the talar ligament, and weight is placed on the posterior portion of the calcaneus. In a chronic tear, the ligament may be absent, thinned, or thickened, but the patient should have no accompanying pressure symptoms. If an ankle collateral ligament injury is suspected, the calcaneal ligament should also be examined, which usually ruptures as a result of a PTMS tear and appears as a hypoechoic and thickened band adjacent to the calcaneus.
Muscle hernia in ultrasound examination
Muscular hernias often present a diagnostic dilemma as patients may be guided by pain, cosmetic mass, or concern about swelling. A muscle hernia occurs when a normal muscle protrudes from its normal anatomical compartment (shell) into the subcutaneous fat through a defect in the underlying fascia. Nearly 90 % of the muscle hernias seen on ultrasound occur in the lower limbs. The tibialis anterior muscle is most commonly affected, but often the fibula, calf, soleus, quadriceps and hamstring muscles are also affected. Associated pain may be due to transient muscle compression or superficial nerve entrapment; however, some have described an association with chronic compartment syndrome, which may represent a different etiology of pain. Treatment depends on the symptoms and may vary depending on the certainty that the lesion is benign. Patients receive therapy ranging from activity modification, compression stockings, and nonsteroidal anti-inflammatory medications to surgery with fasciotomy.
When performing ultrasound examinations, certain technical considerations can improve diagnostic accuracy. Muscle mass should be manually palpated and marked with a pen as abnormalities can be difficult to palpate with an ultrasound probe. Free use of the gel as a surrogate allows light compression to ensure that the hernia is not reduced or obscured, and dynamic assessment during muscle contraction or when positioning the patient can highlight the hernia.
Normal fascia should appear on ultrasound as a thin echogenic line directly over the muscle. A muscular hernia is diagnosed when imaging shows a defect in the echogenic fascia in which a portion of the underlying muscle protrudes through and beyond the fascia, often taking a mushroom shape. The muscle hernia may be slightly less echogenic than the adjacent normal muscle and may be secondary to anisotropy or muscle wasting. Blood vessels are occasionally found crossing the fascia at the site of injury and this is thought to be a possible cause of focal weakness of the fascia.
CAUSES OF LATERAL LIGAMENT TRENCH
Damage to the collateral ligaments can occur during sports such as skiing or soccer. During a direct impact on the outer surface of the knee, the joint space on the inside of the knee opens, causing the medial collateral ligament to overstretch and tear.
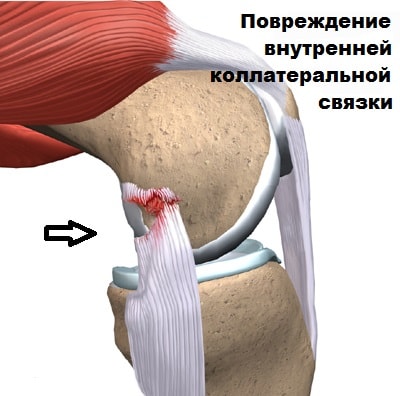
If the effect of the damaging substance continues and the joint space opens further, the anterior cruciate ligament and the medial meniscus will gradually rupture. An injury to the lateral collateral ligament usually results from a sprain of the knee joint, a direct blow to the inside of the knee, or to the front of the shinbone.
SYMPTOMS OF COLLATERAL LIGAMENT INJURY
A collateral ligament tear is usually associated with severe trauma. Damage to the collateral ligaments of the knee joint causes acute pain. Some patients hear a clicking or popping sound at the time of injury.

The tissue surrounding the knee joint swells. Subcutaneous effusions (bruises) occur in the projection of the damaged ligament on the outside or inside of the knee joint.
Damaged ligaments located inside the knee joint (anterior cruciate ligament and posterior cruciate ligament) can cause bleeding into the joint cavity, which doctors call hemarthrosis.
After the injury, the patient often complains that the knee joint 'jumps' or 'cracks' when walking.

How does an MRI scan of the ankle work?
An MRI scan of the ankle examines the following anatomical aspects:
- The relationship between the articular surfaces in the ankle joint and the popliteal area of the foot.
- The condition of the subtalar joint.
- The integrity of the medial and lateral malleolus is checked. The tendons of the tibialis posterior muscle and the tibialis anterior muscle, the long toe flexor muscle, the long and short fibula muscles are unchanged or inflamed.
- There is no deformity or inflammation along the tendon of the tibialis posterior muscle.
- The deltoid ligament is intact.
- The retention of the humeral tendon is intact.
- The anterior and posterior interosseous ligaments are intact, the interosseous syndesmosis gap is flat and not expanded.
- The anterior fibrocartilaginous ligament cannot be felt because it has detached from the lateral malleolus.
- The posterior sagittofemoral ligament is thickened and splayed by stretching and can be identified along its length.
- The posterior edge of the talus is not deformed.
- The heel tendon (Achilles tendon) has no pathological features. The soleus fascia is evenly thickened and the tarsal canal is unchanged.
- The ankle and subtalar joints themselves are not deformed.
- The muscles are not deformed and have homogeneous MRI signal intensity.
MRI of the brachial plexus (MRI of the cervical spine and shoulder joint)
Preparation for the procedure
In most cases, MRI of the ankle is performed without contrast material and does not require any special preparation. In the diagnostic clinics in St. Petersburg, closed and open CT scanners are used for MRI of the ankle joint. The examination takes about 30 minutes under comfortable conditions. Before the MRI scan, the patient must remove all metal objects. To obtain high-quality MRI scans, the person being examined must not move. Therefore, a comfortable position must be assumed before the examination. The report will be issued or sent by email one hour after the examination.
In most medical centers in St. Petersburg, the cost of an MRI scan of the ankle includes the examination, recording of the images on an electronic disk and a written report from a radiologist. As a bonus, some centers offer a free consultation with an orthopedist about the results of the MRI scan of the ankle.
Treatment of a tear of the anterior fibula and sagittal joint ligament
If the anterior fibula and fibro-femoral ligament are completely torn, it is best to repair both ligaments. A free autostendinous tendon graft (e.g., a tendon of the tendon of the biceps femoris muscle) is used with rigid fixation by absorbable or interference screws.


Drilling a canal on the anteroinferior surface of the talus, 17 mm deep, 5 mm in diameter.


The previously removed m-gracilis tendon transplant is fixed with one end in the talus

The tendon is guided in the canals to form the fibula-femoral ligament and the fibula-femoral ligament

Screw fixation in the tension position in the fibula

Drilling out the canal in the heel bone in projection of the insertion point of the patellofemoral ligament
Evaluation
At the end of the procedure, we receive a series of digital images of the ankle with a description of the abnormalities found and a formal report with a detailed transcription and recommendations from the diagnostician. Medicine is an area in which we want to be 100 % safe. We are therefore happy to offer you a second, independent report upon request.
Example of an MRI image of the ankle joint
On a series of MRI images of the left ankle, the conditions in the joint are undisturbed. The bones that make up the ankle joint have a normal configuration and are correctly aligned. The indentation formed by the knuckles is well defined. The cartilage covering the ankle, subtalar and scaphoid joints is ground down and the joint spaces are not narrowed. The synovial membrane is hypertrophic. Areas of local, non-intense bone marrow edema are found in the anterolateral parts of the tibia and the internal parts of the lateral malleolus. The anterior cruciate ligament of the talus shows increased MR signal intensity, evidence of partial damage, and swelling of fatty tissue in the adjacent areas. The other ligaments of the joint show no significant signs of rupture. The intercondylar ligament between the talus and the calcaneus is intact. The Achilles tendon exhibits normal thickness and excursion, with a non-intense increase in signal in the distal portions of the tendon, while overall tension of the tendon is maintained. The fatty tissue surrounding the tendon is unchanged. The tendon and soleus aponeurosis are unchanged. The peroneal soft tissue is unchanged. Fluid accumulation in the ankle and subtalar joint cavity. conclusion: MR evidence of deformative osteoarthritis of the ankle and subtalar joint, stage II; Anterior fibular ligament injury; Achilles tendinopathy. Intra-articular effusion.
- Answering all questions about the examination results and findings
- Help explain the results of the CT scan without using complicated radiological terms
- carry out the examination and offer treatment if necessary.
contraindications
Although MRI is very safe and provides a wealth of information, not everyone is a candidate for an MRI scan of the ankle. The scanner's strong magnetic field interacts with metal objects and can interfere with embedded medical devices. Therefore, an MRI scan is not performed on people with installed heart valves, pacemakers, neurostimulators and cochlear implants. Patients with insulin pumps for administering metered medication are also not eligible for examination. The decision to allow such patients to undergo MRI scans depends on whether the implant's data sheet states that the device is MRI compatible.
Restricted patients include those who have a non-removable metal object in their body - shrapnel, bullets, staples, needles, metal plates, blood vessel clips. The strong magnetic field can heat or loosen the metal, causing burns or internal bleeding.
MRI scans are safe for pregnant women and children, but expectant mothers are advised not to have an MRI scan in the first three months of pregnancy without a doctor's referral.
Prevention: tips for prevention
Preventative measures should be taken to preserve the medial collateral ligaments and reduce the likelihood of injury. It is important that patients recognize and prevent the movement mechanisms that lead to ligament injuries. Remember to protect your knees while exercising. The exercise technique should be carried out with good quality. Footwear with orthopedic properties should be chosen. Care should be taken in situations where there is a high risk of knee ligament injuries. Older people should use a cane to get around.
Possible diseases

In a healthy person, the ligaments can become fatigued if there is too much talking. In this case, it can help to protect your voice. However, hoarseness sometimes occurs as a result of various diseases.
Diseases in which hoarseness occurs:
To find out what a person is sick with, you should consult a doctor for an initial consultation.
Schedule an appointment
ENT doctor
You can make an appointment by telephone
or via the online appointment system on the website
It's easy to tell if an adult has a hoarse voice due to a cold or other illness. It is not always possible to determine the cause yourself. The doctor looks at the neck and sees changes there that a normal person would not notice in the mirror. If in doubt, he can refer you to an ENT doctor or phoniatrist - a specialist in the vocal system.
- Blood test – shows whether the disease is viral or bacterial in nature;
- Laryngoscopy – a detailed examination of the ligaments using a laryngoscope;
- Chest x-ray – if tuberculosis infection is suspected.
You should go to your doctor with the results of diagnostic tests, but do not try to interpret them yourself. Your doctor will prescribe treatment and give you advice on how to improve your voice as quickly as possible.

Also read: Why the runny nose doesn't go away
Professional medical help
Therapy is carried out both conservatively and surgically. Treatment of the knee ligaments is determined by the doctor.
Non-surgical treatment of a recent ligament tear on the side or within the joint and treatment of a partial ligament tear of the knee joint includes:
- administration of PWS;
- application of cold;
- immobilization of the limb;
- If there is blood in the joint, it is removed with a syringe;
- if necessary, a bandage or special joints are applied.
All of these measures are carried out in the first 3-4 days after a sprain or strain. This is followed by therapeutic exercises and massages.
Important: In the first phase of treatment, the leg must not be put under maximum strain, actively moved or kicked. Recovery is significantly accelerated by rest.
If the patient comes to the doctor late and the symptoms of a torn knee ligament are no longer so severe, physical therapy is recommended, which should begin with simple, slow movements, the amplitude of which is gradually increased.
Also read: What treatment is recommended for knee ligament inflammation?
Reasons for prescribing surgery

If conservative therapy does not produce satisfactory results, surgery is the last resort. Symptoms of instability in this case include:
- Intermittent or persistent pain;
- Lack of control over the movement of the knee;
- Recurrent subluxations; shunting;
- fluid accumulation;
- Signs of inflammation.
Arthroscopy is the gentlest form of treatment and is performed under local anesthesia.
Folk treatment methods
Effective recipes from grandmothers can be used for home treatment:
- Grated raw potatoes are applied to the affected area until the mixture dries completely.
- A mixture of badyga and white clay, diluted with water to the consistency of a foam, is applied to the knee for 30 minutes.
- Applying a grated aloe or kalanja leaf reduces pain and swelling.
- Boil 2 parts horseradish in 8 parts boiling water for a few minutes and add 1 part honey to the liquid. After 24 hours, cool the remedy in the refrigerator and take 2 (tablespoon) before each meal.
Such treatment should be carried out under the guidance of a specialist, since such methods do not eliminate the effects of rupture of ligaments in the knee joint, but only relieve pain and swelling.
Diagnosis of knee pain
In order to quickly fix the problem, it is important to know the cause. This is difficult to do alone. It is best to leave it to specialists to determine the cause of the pain using modern diagnostic tests. The patient will be asked to undergo the following procedures:
| diagnostic technique | Time |
|---|---|
| General blood test | 10 mins |
| Ultrasound examination of the knee joint | 30 minutes |
| X-ray examination | 10 mins |
| Magnetic resonance imaging of the knee joint | 30 minutes |
Only after a thorough examination of all the results can the doctor know exactly why the patient has pain on the inside of the knee. This data will also be used to develop an effective treatment program.
Which doctor can help?
The biggest mistake many people make is that they try to solve the problem themselves. This often has catastrophic consequences: the spread of the disease, the occurrence of complications. Such pain should only be treated by specialists. If you have similar symptoms, you should urgently consult a doctor:
Our specialists
The prices stated on this page are not a public offer. Please call us at 8 (495) 255-37-37 to inquire about costs and appointments.
fees
These specialists quickly diagnose lateral knee pain from the inside. At the first appointment, the doctor examines the patient, listens to the complaints and asks the patient:
- How long have the symptoms existed?
- Are there any other signs of discomfort?
- Has the person concerned suffered any knee injuries in the recent past?
- Has the affected person tried to treat the condition themselves? By what means?
- Does the patient suffer from chronic illnesses?
- Is he/she taking medication?
- Are you allergic to medications?
- Femoral collateral ligament.
- tibial ligaments.
- Rupture of the medial collateral ligament.
- tibial fasciitis.
- Treated subluxation of the ankle.
- Collateral ligament rupture.
- Axis of rotation of the knee joint.
- Ligament damage in the right ankle.
