A 3×10 cm long graft is cut from the broad fascia of the thigh, the base of which lies on the external condyle. An osteochondral suture is placed with the base of the femoral epicondyle backward to match the width of the graft.
- Introduction.
- The lateral ligament group of the ankle.
- Caused
- diagnosis
- Fibular collateral ligament (collateral ligament)
- DIAGNOSIS OF SIDELAND INJURIES
- CONSERVATIVE TREATMENT OF KNEE PRAGARALIDA INJURIES
- Knee Collateral Ligament Injuries 3.jpg
- Rupture of the cruciate ligament in the knee - treatment
- Torsion of the collateral ligaments of the knee - treatment
- treatment methods
- Oblique view of a female radiologist and her patient during a knee MRI scan in the clinic_637285-467-1.jpg
- ACS features.
- Bone contusions and microfractures
- diagnostic procedures
- Physical examination, which includes the following tests:
- Radiological examination.
- Symptoms of a knee collateral ligament rupture
- Treatment of torn collateral ligaments of the knee joint
- Causes of collateral ligament tear
- Treatment of the collateral ligament in the knee joint
- Surgery for a collateral ligament injury
Introduction.
Understanding the anatomy of the ankle ligaments is essential for proper diagnosis and treatment. An ankle ligament injury is one of the most common traumatic reasons for seeking medical attention. Chronic ankle pain is often the result of a ligament failure.
The ligaments of the ankle can be divided into three main groups: the lateral ligament group, the deltoid ligament group and the interosseous ligament group.
The lateral ligament group of the ankle.
This is the most commonly damaged ankle ligament. It plays an important role in limiting anterior displacement of the thigh and soleus flexion of the foot. The ligament is located in close proximity to the joint capsule and is often represented by two bundles. The bundles are separated by vascular branches of the brachial artery.
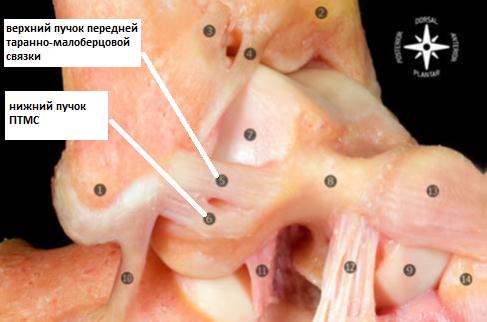
The anterior talaspinal ligament arises at the anterior border of the fibula, 10 mm from its apex. In the neutral position of the foot, it is strictly horizontal and attaches to the proximal part of the thigh bone directly at the border of the articular surface. The width of the base on the talus is 6-10 mm.
Plantar flexion of the foot puts pressure on the upper tendon bundle, while dorsiflexion of the foot only puts pressure on the lower tendon bundle.
Caused
- Simultaneous flexion, extension and rotation of the knee in the lower leg (the movement must be very rapid for the injury to occur);
- flexion, extension and inward rotation of the lower limbs;
- hyperextension of the knee joint;
- Blows to the knee joint.
- pain in knee; pain increases when trying to move knee;
- impaired mobility of the joint;
- Constant muscle tension in the upper and lower leg;
- swelling in the knee joint that increases in size;
- Bleeding under the skin after the injury.
Ligament injuries in the knee joint are usually accompanied by hemarthrosis, a build-up of blood in the joint cavity.
diagnosis
The doctor usually makes the diagnosis after an examination. After several tests, the doctor can confirm that the ligament is damaged and how severe the injury is.
- X-ray. This is required to distinguish a ligament injury from a broken bone.
- Ultrasound examination of the joints.
- MRI. All the ligaments and other anatomical formations of the knee joint are clearly visible in the pictures.
- Arthroscopy is the most accurate method for diagnosing a cruciate ligament tear. The doctor makes a puncture and inserts a miniature video camera into the joint cavity. Cruciate ligament replacement can be performed immediately during arthroscopy.
Fibular collateral ligament (collateral ligament)

Damage to the ligaments of the knee joint is a common injury that occurs more frequently in active young people, usually at home or while playing sports. Damage to the ligaments of the knee joint results from excessive movement of the joint (hyperextension, twisting of the limbs, adduction and inversion of the lower limbs). Sometimes the injury is also caused by an impact or pressure on the lower extremity. Patients with knee ligament injuries complain of pain, restricted mobility and swelling in the area of the joint. Diagnosis is made on the basis of history and clinical examination; X-rays can also be taken to rule out a fracture. An MRI scan of the knee joint, a diagnostic puncture or an arthroscopy are also indicated.
Knee ligament injuries are a common injury that occurs more frequently in active young people and mostly occurs at home or while playing sports. Ligament injuries in the knee joint result from excessive movement of the joint (hyperextension, twisting of the limbs, adduction and abduction of the lower limbs). Sometimes the injury is also caused by an impact or pressure on the lower extremity.
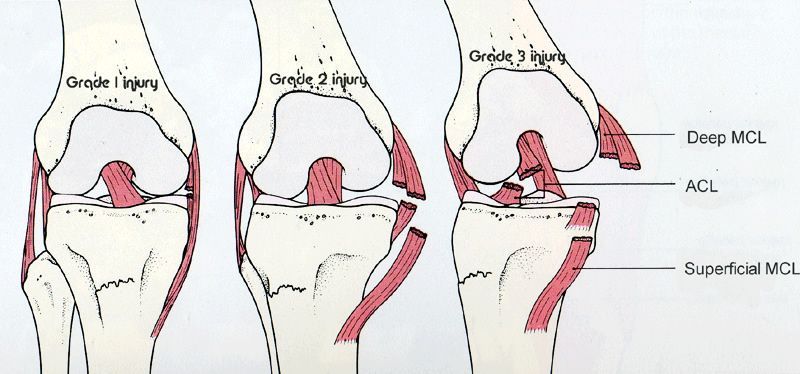
- Grade I. Partial rupture of the ligaments of the knee joint (individual fibers are torn). This is often referred to as a sprain, although the ligaments of the knee joint are actually inflexible and cannot be stretched;
- Grade II. Incomplete ligament tear (tearing of the ligaments of the knee joint);
- grade III Complete rupture of the ligaments of the knee joint. Usually associated with damage to other joint components (capsule, meniscus, cartilage, etc.).
In traumatology, a distinction is made between injuries to the collateral ligaments (outer and inner ligaments) and cruciate ligaments (anterior and posterior ligaments), depending on the location of the injury.
DIAGNOSIS OF SIDELAND INJURIES
The first medical examination immediately after the injury usually gives a very good indication of which ligaments are injured.
When examining the joint, the doctor looks for soft tissue swelling or bleeding and gently palpates the knee to determine where it is most painful.
The doctor may also perform specific stress tests to assess the degree of mobility in the lower extremity relative to the thigh. Stress tests for ligament injuries often provide valuable information. When the knee is loaded, the joint space on the side of the injury increases, indicating that the ligaments involved are insufficient. Ligament injuries can be partial or complete.

If the ligament is only partially damaged, the joint space is less open and the instability of the joint is not as pronounced. A stress test in the acute phase of the injury usually causes pain in the projection of the damaged collateral ligament.
A few hours after the injury, ligament damage is more difficult to diagnose due to swelling and muscle spasms. In such cases, the knee joint should be re-examined after a few days, when the pain and swelling have subsided.
Between exams, the joint should be protected with a cast, the limb should be elevated, and the patient should be on anti-inflammatory medication.
If hemarthrosis is detected in the joint, aspiration (removal) of blood from the joint is required.

Blood in the joint with a mixture of fat is a sign of bone or cartilage damage.
A radiological examination is mandatory to rule out bone damage.
X-ray guided stress tests are sometimes performed, and the width of the joint space opening can be documented as a result of such tests.
CONSERVATIVE TREATMENT OF KNEE PRAGARALIDA INJURIES
Isolated injuries to the inner and outer collateral ligaments rarely require surgical treatment. Partially injured ligaments of the knee (grades I and II) do not usually result in joint instability and are treated conservatively by reducing pain and swelling and limiting limb movement (use of a cast).
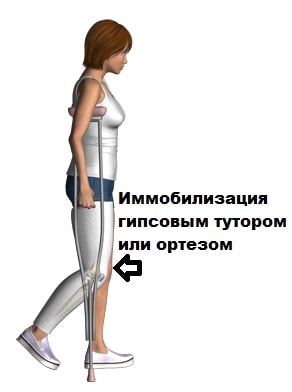
A cast is usually applied for up to 4 weeks, limb weight bearing is usually allowed as pain subsides and mobility on crutches increases.
Knee Collateral Ligament Injuries 3.jpg

Knee Collateral Ligament Injuries 3.jpg
When the collateral ligament of the knee is completely torn, it needs surgical repair or reconstruction. It is also necessary if the person concerned does not have any significant functional restrictions. The operation prevents the development of arthrosis.
Reconstruction is rarely undertaken. The doctors sew the band themselves, which is then fused together. This technique is less traumatic than reconstruction because no bone tunnels need to be drilled, but only 10 percent of patients are candidates for this procedure. It is performed when the collateral ligament is freshly damaged, in the distal area, with high quality and sufficient residual tissue.
It is most commonly performed on the collateral ligament of the knee. The 'gold standard' is autoplasty – reconstruction from the patient's own tissue, usually from the autogenous semitendinosus muscle. Synthetic materials such as lavsan are also used less frequently. At the clinic of Dr. Glazkov, the operation of a torn knee collateral ligament is performed using arthroscopic techniques, which reduces the traumatic nature of the procedure.
Rupture of the cruciate ligament in the knee - treatment
In the case of minor injuries without damage to the overall integrity of the ligament apparatus, conservative therapeutic measures are sufficient. For a knee ligament strain, medications are prescribed:

physical therapy
Non-pharmacological measures are prescribed, primarily physiotherapy (electromagnetic fields, fango, ultraphonophoresis with non-steroidal analgesics).
The length of time it takes to treat a sprained knee depends on the type of injury and its location. The average duration of conservative treatment is about a month. If a serious sprain is diagnosed, treatment includes surgery. The surgery is performed through an open approach or arthroscopy.
Torsion of the collateral ligaments of the knee - treatment
If a sprain of the inner collateral ligaments of the knee is diagnosed, the treatment is usually surgical. If a sprain is diagnosed in the back of the knee, treatment always includes physical exercises to strengthen the connective tissue structures. Stretched inner collateral ligaments of the knee joint are repaired by arthroscopy.
The tissues of the articular apparatus have the ability to regenerate (repair) the cells and fibers of the intercellular substance. The duration of the regeneration process depends on the individual characteristics of the human body, its age and the presence of a concomitant pathology. These factors affect how long it takes for a knee sprain to heal.
treatment methods
In the case of a partial tear (sprain) or even a complete tear of only one collateral ligament, conservative treatment of the patient is possible. However, in the case of a complete tear, surgery is preferable. This is because torn ligament structures do not always heal spontaneously.
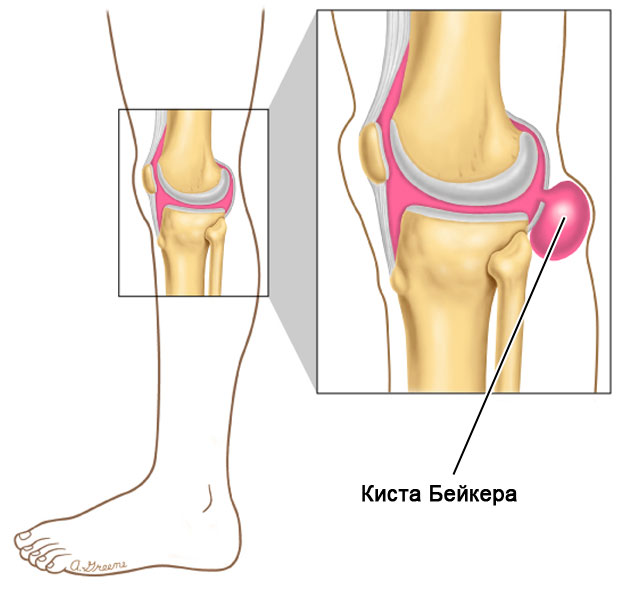
The consequences of an inappropriate therapeutic measure can be catastrophic for the patient. A permanent disability arises. When the acute phase is over, the pain subsides. However, the instability of the joint persists. When the medial collateral ligament is torn, the knee can swing outward easily because there is no force holding the joint in the correct position. In order to be able to walk normally again, the knee is immobilized either with a bandage or a special orthosis. However, this only solves the problem temporarily. Over time, the muscles of the lower leg atrophy, and long-term instability of the joint leads to osteoarthritis of the knee.
In order to avoid such problems in the future, the right choice of treatment is crucial. Instrumental studies serve this purpose: not only X-rays, which help to identify a hernia, but also MRI, which provide the doctor with more accurate information. After conservative treatment, the patient is monitored. If the instability of the joint persists, it is operated on.
Oblique view of a female radiologist and her patient during a knee MRI scan in the clinic_637285-467-1.jpg

Oblique view of a radiologist woman and her patient during the knee MRI scan in the clinic_637285-467-1.jpg
The basic principle of conservative treatment is to bring the medial (tibial) ligament of the knee to a state of complete functional rest. This creates the necessary conditions for the healing of the torn fibers. At the same time, the symptoms are treated in the acute phase (pain relief, regression of the swelling).
In the acute phase, immediately after the injury, the person concerned is carefully examined. A tear in the medial collateral ligament is usually caused by a blow to the lateral surface of the knee. This is usually a sports injury. It can be accompanied by damage to other intra-articular structures (meniscus, joint capsule, ligaments).
Sometimes surgery is done soon after the injury. However, if only the inner collateral ligament is damaged, conservative treatment is performed. The knee is punctured, irrigated, and the blood removed. A local anesthetic is administered internally to eliminate the pain. Usually 0.5 % procaine is used. A plaster splint is applied for 1 week. Once the joint swelling has subsided, it is replaced with a circular cast from the groin to the toes.
If the medial collateral ligament of the knee joint is torn, the tibia is brought into a lying position. This immobilization ensures that the mobility of the leg in the injured joint is restricted. Limb positioning reduces stress on the damaged ligament. The ligament remains in a relaxed position for a longer period of time, allowing the regeneration processes to proceed normally.
- Physiotherapy – various methods are used to improve blood supply to the joint, accelerate swelling reduction and normalize regeneration processes;
- therapeutic exercises – static exercises are recommended from the third day, in the convalescent period (after removing the plaster cast) it is necessary to move on to dynamic exercises aimed at strengthening the muscles of the limbs;
- Arthrotherapy – injections into the joint with hyaluronate and platelet-rich plasma, which accelerate tissue regeneration and prevent cartilage degeneration.
ACS features.
- Primary limitation of anterior tibial dislocation: 85 % resistance on the anterior drawer test when the knee is held in 90 degrees of flexion.
- Secondary limitation of tibial rotation and varus angulation: valgus at full knee extension.
- Proprioceptive function: presence of mechanoreceptors in the ligaments.
ISS injuries (Grade I-III) pose a particular challenge as they lead to post-injury stiffness of the knee. Most orthopedists initially treat the MCI injury (for six weeks) with a knee brace to limit mobility. During this period, the athlete goes through a comprehensive rehabilitation program. Only then is an ACL reconstruction performed.
Bone contusions and microfractures
Subcortical trabecular bone tearing (bone contusion) can result from pressure on the knee during a traumatic event and is particularly associated with a torn ACL. Accompanying meniscal and ISS injuries favor the progression of bone contusion. Focal signal abnormalities in subchondral bone seen on MRI (and not seen on radiographs) are thought to represent microfractures, hemorrhage, and swelling without disturbing adjacent areas or the articular cartilage. Bone contusions can occur in isolation from ligament or meniscus injuries.
Hidden bone injuries were found in 84-98 % of the patients with ruptured PCC. Most have lateral compartment injuries affecting either the lateral femoral condyle, the lateral tibial plateau, or both. Although most bone injuries resolve, irreversible changes can remain. The literature is unclear about how long these bone lesions persist, but it has been reported that they can persist for many years on MRI. Rehabilitation and long-term prognosis may be uncertain in patients with extensive bone damage and associated articular cartilage damage. In the case of severe bone impingement, it is recommended to delay the return to full weight bearing to prevent further destruction of the subchondral bone and further aggravation of the articular cartilage damage.
diagnostic procedures
An accurate diagnosis can be made by the following procedures:
Physical examination, which includes the following tests:
Radiological examination.
If an ACL tear is suspected, radiographs of the knee joint should be taken in normal and lateral views as well as in patellar projection. The standing, propped view allows an assessment of the joint space between femur and tibia. It also enables the intertrochanteric indentation index to be measured, which provides important prognostic values for ACL tears. The patellar tendon and its height are measured on a lateral x-ray. Tunnel vision can also be helpful. Merchant's X-ray not only shows the joint space between the femur and kneecap, but also helps determine if the patient has a dislocated kneecap. The presence of the following factors should be noted on the radiographs:
The index of the intercondylar notch is the ratio of the width of the intercondylar notch to the width of the distal thigh at the level of the popliteal fossa, as measured on a radiograph of the knee joint in tunnel view. The normal intercondylar indentation index is 0.231 ± 0.044. The intercondylar indentation index is greater in men than in women. In athletes with non-contact PCC injuries, the incision width index was found to be at least 1 standard deviation below the mean, meaning someone with a PCC injury is likely to have a small incision width index compared to the norm. This is measured with a ruler parallel to the joint line. The narrowest point of the indentation is measured at ruler level. In more chronic ACL injuries, there may be reduced intercondylar eminence, hypertrophy, or osteophyte formation at the patellar margin.
This is also one of the reasons women are more prone to ACL injuries than men. It was also observed that the internal angle of the lateral femoral condyle was significantly higher in female athletes with a PCC tear than in female athletes without a PCC tear. The width of the intercondylar notch was statistically smaller in athletes with an ACL injury than in non-injured athletes. In addition, it was found that the internal angle of the lateral femoral condyle was a better predictor of ACL rupture in young handball players than the width of the intercondylar notch.
Symptoms of a knee collateral ligament rupture
Patients experience pain and instability of the knee joint, but this is limited to the area of the tear.
The joint is swollen and its contours are smoothed. On the 2nd or 3rd day after the injury, there is a sometimes extensive bruise that extends down to the shin. Free fluid (hemarthrosis) is noted: a positive sign when kneeling and balancing the kneecap. On palpation, local tenderness is revealed in the projection of the injured ligament.
When the collateral ligament is torn, excessive deviation of the tibia to the side opposite the damaged ligament is noted. For example, if there is a suspicion of a tear in the medial collateral ligament, the doctor will hold the outer surface of the patient's knee joint with one hand and use the other hand to tilt the tibia outward. If the tibia can be tilted outwards much more than in a healthy leg, this indicates a tear in the medial collateral ligament. The patient's leg must be extended at the knee joint during the examination. For acute injuries, these examinations are performed after procaine is injected into the knee joint cavity and the knee is anesthetized.
After the acute phase has subsided, the knee joint remains unstable ('wobbling'), so that the patient is forced to support the joint with bandages or a special knee brace. Muscle wasting of the limbs gradually develops and symptoms of deforming gonarthrosis appear.
Laboratory and instrumental studies
If deforming osteoarthritis of the knee begins to develop, the clinical diagnosis can be confirmed by an X-ray examination using the equipment offered in the clinic. The X-ray clearly shows a widening of the joint space on the side of the injury.
[1], [2], [3], [4], [5], [6], [7]
Treatment of torn collateral ligaments of the knee joint
The acute phase of the injury is treated as an inpatient.
Conservative treatment of torn collateral ligaments of the knee joint
Isolated ruptures of one of the collateral ligaments are treated conservatively. A puncture of the knee joint is performed, which eliminates hemarthrosis, and 25-30 ml of 0.5%ige procaine solution is injected into the joint cavity. A plaster splint is applied for 5-7 days (until the swelling subsides), then a circular plaster cast is applied from the inguinal crease to the fingertips in a functionally favorable position with excessive deviation of the lower extremity (hypercorrection) towards the lesion. From day 3, UHF and static exercises are recommended. Immobilization lasts 6-8 weeks. After healing, rehabilitation treatment is recommended.
Surgical treatment of collateral ligament tears in the knee joint
There are several ways to surgically repair the collateral ligaments of the knee joint.
Tibial Collateral Ligament Plastic. Tibial collateral ligament tears are more common than fibular collateral ligament tears. They are often associated with injuries to the medial meniscus and the anterior cruciate ligament (Turner's triad).
In the past, the Campbell procedure was the most commonly used procedure to restore stability to the knee joint after a tibial collateral ligament tear. The material used for the plication is a strip of the broad fascia of the thigh.
Various methods have subsequently been proposed for surgical repair of the tibial collateral ligament: pinching, ligament plication with Lavsan, and the cancellous tendon.
In 1985, AF Krasnov and GP Kotelnikov developed a new method of autoplastic of this tape.
A soft tissue incision is made in the projection of the lower third of the tendon and the tendon is isolated.
A bone and periosteal suture is made in the area of the inner femoral epicondyle and the tendon is pushed underneath. It is then sewn to the periosteum at the entrance and exit. The flap is reinforced with transperiosteal sutures. The wound is sewn up.
Causes of collateral ligament tear

An isolated rupture of the collateral ligament is extremely rare due to the anatomical conditions and other typical injury mechanisms. When a collateral ligament is ruptured, the force of the injury is usually sufficient to damage what is known as the posterolateral (back-outside) complex, which consists of the external collateral ligament, the hamstring muscle tendon, and the posterolateral (back-outside) capsule of the knee joint consists. Although these injuries are fortunately rare, they do occur in younger patients when they engage in active sports that primarily require active use of the full range of motion of the knee joint. These sports include competitive sports such as soccer, basketball, and volleyball, as well as extreme sports such as skiing, skydiving, parkour, cycling, and similar sports.
A collateral ligament tear or an injury to the entire posterolateral complex cannot be overlooked. It is accompanied by a noticeable 'cracking' or 'crunching', severe pain and limited support. After a short time, swelling of the entire area of the damaged knee joint occurs.
Treatment of the collateral ligament in the knee joint

First aid must be given immediately and consists of strict exercise limitation, elevating the injured lower extremity, cooling the injured area, and expeditious transport of the casualty to a specialized medical facility. An orthopedist/traumatologist will examine the injured knee joint, recommend x-rays, and if a fracture of the lateral (outer) plateau (condyle) of the tibia cannot be confirmed, additionally recommend magnetic resonance imaging (MRI) of the knee joint. The quality and speed of diagnosis have a major impact on the outcome of treatment. Examination and treatment advice should be carried out by a competent physician with extensive experience, since isolated injuries of the lateral (external) complex are relatively rare and all structures of the knee joint must be carefully examined for concomitant damage.
The number of damaged structures in the knee joint determines the treatment strategy. A tear of the lateral collateral ligament cannot be treated without surgery, unlike e.g. B. A tear of the medial collateral ligament. The reason for this is the distance of the collateral ligament from the soft tissues of the joint and its greater isolation.
Surgery for a collateral ligament injury

- Rupture of the medial collateral ligament.
- Collateral ligament rupture.
- Posterior ligament of the head of the fibula Latinus.
- tibial ligaments.
- Anterior fibula ligament tear in the ankle.
- Image of torn ligaments.
- Axis of rotation of the knee joint.
- The intercondylar joint.
