What you should never do if your child has bruises on their feet:

- Cold hands and feet: norm, fever, connection to diseases
- 'Cold-blooded' women and 'hot-blooded' men
- Definition of the disease. causes of the disease.
- Causes Exfoliative Keratolysis
- Symptoms of exfoliative keratolysis
- Types of foot bruises in children
- Symptoms of leg injuries in children
- How to measure your child's foot size according to age
- How to measure your child's feet
- Similar video:
- Complex regional pain syndrome in children
- Bone tumors as a cause of leg pain in children
- Foot care in childhood
- Recommendations on foot hygiene and the choice of shoes and stockings for children
- Pediatric care for teenagers
- Pedicure for children (teenagers) in the salon
- Recommendations for the use of grooming products for teenagers
- Consequences of onychocryptosis in children
- Treatment options for an ingrown toenail
- Conservative treatment
- surgical method
- How does a child grow and what are growing pains?
- What are growing pains like?
- What kind of skin itching is there and what causes it?
- Localized itching of the skin
- itching all over the body
- Which doctor should I go to if I have itching?
Cold hands and feet: norm, fever, connection to diseases
Are cold hands and feet a sign that something is wrong with the blood flow in the small vessels in the limbs? The blood does not reach the capillaries and does not warm the fingers? This is most likely the case when the hands and feet get very cold, even though it is warm enough outside or in the house. And if you yourself are somehow accustomed to such phenomena, your friends and just those around you, who happen to notice the abnormal temperature of the human body, rarely do without remarks and the question: 'Why such icy hands? Of course, one can consider oneself healthy, but cold hands still cause some discomfort, and the owner of the problem begins to try to get rid of it.
Even more questions and concerns arise when the child's feet and hands get cold, especially if the child is still an infant. The grandmothers who worry most about this are those who have raised their children and have somewhat forgotten the physiology of young children and are therefore terrified of hypothermia and colds. In an effort to keep the child warm, they occasionally touch their hands and nose, check that their feet aren't freezing, and admonish the young parents. When are cold hands and/or feet normal and when should they be taken as a sign of illness? The reader will find answers to these and other questions about cold extremities below.
'Cold-blooded' women and 'hot-blooded' men
Some people always walk around in socks and warm sweatshirts, even though it's quite warm inside and out. What is the reason for that? Why do people tolerate the same ambient temperature differently? Why is it that in old age the 'cabbage leaves' from clothing no longer bother and doctors recommend that small children dress cooler than adults? Here's why:
- Women get colder over the course of their lives leading up to the symptoms of menopause - this is quite natural. The constant fluctuations in hormone levels caused by the physiology of the body affect thermoregulation in one way or another. It gets even more difficult with the onset of menopause, which can bring about such changes in thermoregulation that women in general are sometimes unable to properly recognize and feel temperature, and humbly experience hot flashes and colds as symptoms an unfortunate period and perceive their own means of combating it, albeit not always successfully;
- Men Men who are by no means athletically built, that is, tall, slender, thin, asthenic men, also have some fear of the cold, although less so than women. But tall physiques with a well-developed musculature or subcutaneous fat layer go 'chest first' and are not afraid of the cold because they have good thermoregulation;
- The heat exchange process decreases with age – Very old people start to dress warmer;
- The child's thermoregulation mechanisms are not yet stable, However, with age, heat production and heat transport improves, and cold hands and feet no longer frighten parents.
It should be noted that apparently healthy people almost always have vegetative dystonia, or vitamin and micronutrient deficiencies. When you're on a diet, your hands can start getting cold, especially when you're hungry, and if you've been sitting in a cold room for a long time, you might find that your feet freeze (you have to get up and get socks), although some do People wear socks, scarves and cravats all the time indoors and outdoors in fairly warm weather.
Definition of the disease. causes of the disease.
Exfoliative keratolysis (exfoliative keratolysis) – is a focal, symmetrical desquamation of the skin on the palms, fingers and less commonly the soles of the feet. It is characterized by dry skin and air-filled superficial blisters.
Exfoliative keratolysis is also known as recurrent focal palmar desquamation, dry lamellar dyshidrosis, and recurrent palmar desquamation.

The disease is widespread and often chronic, but benign. Exfoliative keratolysis is more common in children and adolescents and less common in adults. It is often confused with psoriasis, eczema or chronic contact dermatitis. In people with excessive hand sweating, the condition worsens in warm weather and may be associated with hyperhidrosis – increased sweating [1].
Formerly, exfoliative keratolysis was called dyshidrotic eczema and thought to be caused by sweat glands. This connection has since been refuted, but the term 'dyshidrotic eczema' is still used [2].
Dyshidrotic eczema, also known as pomfolix, may precede exfoliative keratolysis. This eczema causes fluid-filled blisters to form on the fingers, toes, palms, and soles of the feet, and causes severe itching [2] . The cause of dyshidrotic eczema is not known, but it is likely that many factors contribute to the development of this condition. In most cases, the cause and the predisposing factor cannot be determined [17] .
causes Exfoliative keratolysis
It has been suggested that exfoliative keratolysis may be caused by a fungal lesion, but further studies have not confirmed this hypothesis.
Possible triggers of exfoliative keratolysis:
- Friction and contact with water[3][6];
- Soaps, detergents and solvents: The chemicals in it can crack and blister your hands;
- allergies: Food, air pollutants, and other substances can trigger skin allergies;
- Stress: Can not only cause, but also aggravate the course of the disease;
- Hot climate: Warm weather increases perspiration, which can lead to flaky skin;
- exposure to salt water;
- dry skin.
Symptoms of exfoliative keratolysis
Exfoliative keratolysis is often asymptomatic, with only small skin lesions on the back of the hand [5]. Skin peeling is preceded by air-filled blisters that are never filled with fluid [3] . In some cases, the disease begins with only focal skin desquamation without blistering.
When the blisters are opened, broad, mesh-like, round, or oval lesions remain. These peel off, spreading to the periphery and forming large, round, lacy areas.

The desquamated epithelium loses its protective function and becomes red, dry and cracked. Desquamation may be preceded by mild itching or burning, and in some cases the desquamated epithelium may be painful (3).
The rashes are always symmetrical. Sometimes deep cracks form on the fingertips, the skin becomes hard and numb, and it takes 1-3 weeks to heal completely. Exfoliative keratolysis can recur several weeks after new skin has formed at the exfoliation site.
Types of foot bruises in children
Depending on the depth of the injury suffered by a child with a bruised leg, experts distinguish four degrees of severity:
- The first, mildest, degree is characterized by minor soft-tissue changes, minimal pain, and no skin damage;
- The second degree is characterized by contusion of muscle structures with bruising and swelling;
- The third stage involves ligaments and tendons;
- The fourth stage is characterized by significant damage to all structures, including cartilage and bone, extensive subcutaneous hemorrhage, and long-term impairment of limb function.
Most young children are diagnosed with first- and second-degree contusions that require short-term treatment. Serious injuries are more common in adolescents and children who have been in life-threatening situations (car accident, building collapse, etc.).
Symptoms of leg injuries in children
The main symptom is a sharp pain that comes on suddenly at the time of injury. Within 3-15 minutes of impact, the injury site will swell and the skin will be hot to the touch and red. In the case of severe bruises, small capillaries rupture, which is noticeable as hematomas and bruises. Falls and collisions with hard objects can also cause abrasions and scratches on the skin of different depths.
A child with a bruised foot complains that the foot is swollen, it burns, is numb, and hurts when it steps on it. The gait changes: the children try not to put all their weight on their feet and look for additional support.
How to measure your child's foot size according to age

There are average values that give a rough idea of the length of a child's foot at his age. However, it is important to remember that every child is different and in some cases the measurements taken on a specific child will not match those that are generally accepted. So if you decide to measure your child's feet by age, the table will only give you an approximate value.
How to measure your child's feet
Measure the foot while standing on the floor or other flat, smooth surface. Place a piece of paper under the foot and trace the outline of the foot with a pen or pencil. It is best to measure both feet at the same time. If they are different lengths, choose shoes based on the size of the larger foot. Add half a centimeter to the result if you want to buy shoes for the summer and one and a half if you want to buy shoes for the winter.
For younger children who are not yet able to stand securely, you can measure the length of the foot with a piece of string or a regular school ruler. With this simple tool, you can draw an imaginary line from the center of the heel to the edge of the child's big toe.
This line should not be straight, but slightly angled.
If you have measured your child's feet to know how many centimeters they are, you can use the foot measurement chart, which tells you how many centimeters your child's feet measure for a specific shoe size. You can also find the foot measurements for each model in our catalogue.
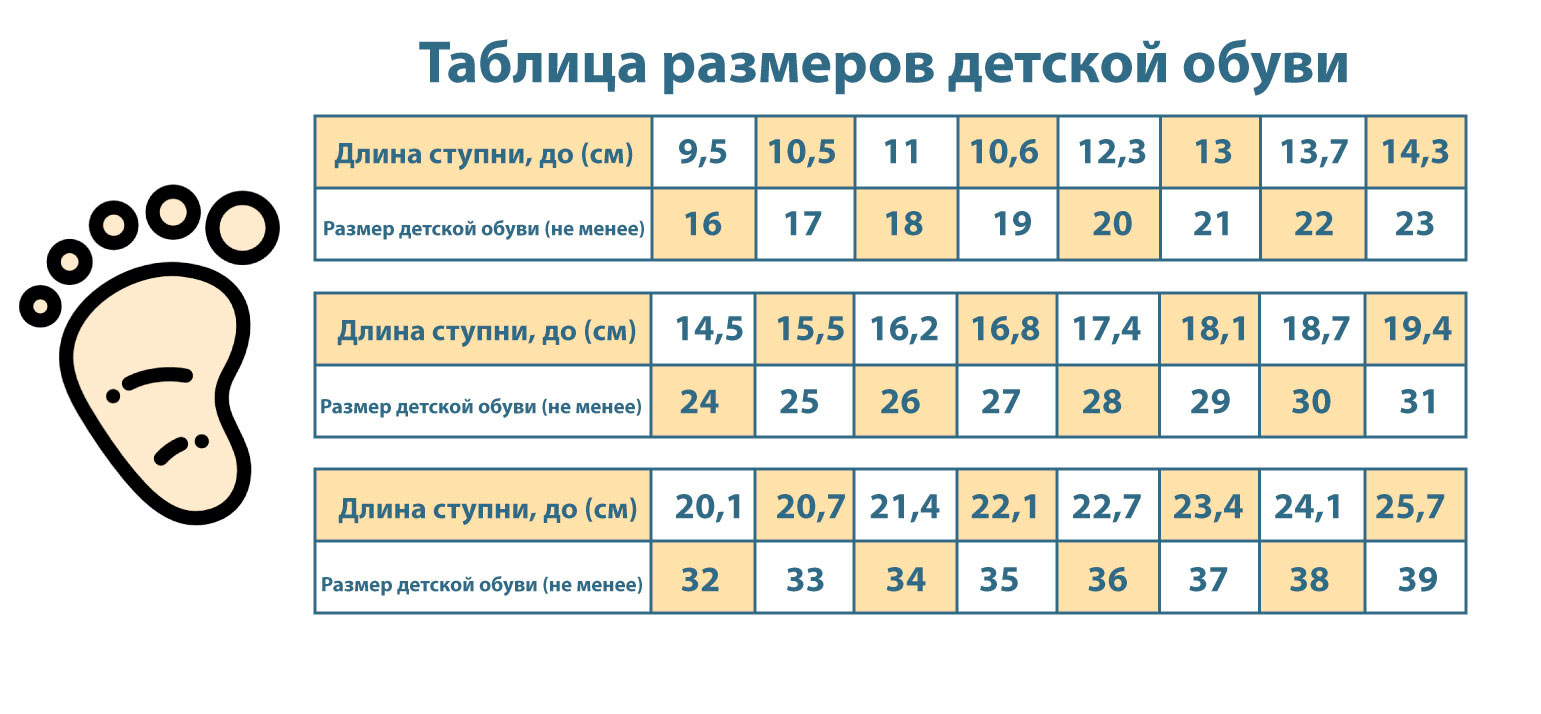
Choosing the right shoe size for children is very important. Do not buy shoes or sandals that are too long or too short for your child's needs as they will not be comfortable to wear.
Similar video:
Complex regional pain syndrome in children
Complex regional pain syndrome in children can develop after (often minor) trauma or without any triggers. Clinical signs include marked pain, hyperesthesia (increased sensitivity to stimuli), allodynia (painful sensations in response to non-painful stimuli), limitation of movement of the affected limb to bizarre posture, and sometimes swelling of the limb and skin changes (marbling, pale skin, reduced skin temperature).
Diffuse musculoskeletal pain syndrome is characterized by sleep disturbances (insomnia, lack of freshness upon waking, daytime sleepiness) and the presence of painful trigger points in soft tissues in the absence of other symptoms suggesting an organic pathology. In some cases, it may be a manifestation of chronic fatigue syndrome.
Diffuse musculoskeletal pain syndrome is often associated with a state of stress of which the parents may not be aware (stressful situation at school, bullying or other forms of violence, pressure from parents). A thorough physical examination and an appropriate number of additional examinations are necessary to rule out organic disease.
Sometimes the syndrome diffuse musculoskeletal pain syndrome can manifest itself in an organic disease such as B. JIA, develop. Treatment (both outpatient and inpatient) must be individualized and multidisciplinary.
Bone tumors as a cause of leg pain in children
Malignant tumors (osteogenic sarcoma, Ewing's tumor) are rare. They are manifested by pain or swelling and sometimes pathological fractures. Osteoid osteoma is a benign tumor that usually occurs in adolescents, often in boys. It usually affects the femur or tibia.
Pains More pronounced at night, reduced by taking salicylates. Sometimes a slight local pain sensitivity is noted. In most cases, the diagnosis can be made by a radiograph: there is a well-defined, radiopaque focus of osteoid tissue surrounded by a zone of osteosclerosis. If the X-ray is negative, a CT or MRI scan is required. The treatment is surgical in nature.
Foot care in childhood
The main goal during this period is to acquire the useful habit of regular foot hygiene.
Children up to the age of 5-7 years have physiological flat feet. Children are born with flat feet and the arches of the feet do not develop until the child begins to walk and certain muscles are activated.
Children's nails are thin, often trapezoidal, and may curve upwards (koilonychia). These features often lead to ingrown nails. When the nail plate reaches a certain age, it takes on an 'adult' shape.
There are therefore two main goals in children's foot care: the formation of a correct foot arch and the prevention of ingrown toenails.
Recommendations on foot hygiene and the choice of shoes and stockings for children
When shopping for new shoes and socks for your child, keep the following recommendations in mind:
Make a wise choice. Both shoes and socks should be the right size. Allow for +0.5 cm for children, as they grow very quickly. Don't buy too big. Shoes should fit snugly on the foot and have a heel (1-1.5 cm) that does not protrude beyond the heel. The sole should bend easily.


Teach children to take care of their own foot hygiene - wash their feet every day and trim nails on time.
When cutting and shaping the nails, the corners should not be sharp, but should be slightly rounded so that they do not grow in and put pressure on the skin of the adjacent toes.
Before your child's pedicure, you can apply an enzyme serum and then gently clean the side rollers with an orange wand. This also helps to gently trim your child's nails, especially if they are broken and have chipped corners.
Pediatric care for teenagers
By the age of 11 or 12, the arches of the feet in children are fully developed, so at this age it is already possible to assess whether flat feet are present or not. Hyperhidrosis – excessive sweating of the skin – can also occur due to hormonal changes in the body. On the feet, this uncomfortable feeling is exacerbated by wearing closed-toe shoes and heavy loads. Damp skin can be traumatized by nail shafts. Ingrown nails can form on the nail plate. Because the nail is still thin and not fully developed, it is more prone to deformation than in adults. This also leads to ingrowths. The skin on the soles of the feet peels due to the increased moisture. Moisture is also a factor that favors fungal infections. Add to that hormonal imbalances that can weaken the immune system, study stress, lack of sleep, and psychological factors, and it's not uncommon for teenage feet to develop other problems. For example, the appearance of warts.
Pedicure for children (teenagers) in the salon
At this age you can and should start pedicures in the hairdressing salon. Careful consideration should be given to the choice of salon and qualified professionals to work with the feet of children and young people.

Pedicures for children (teens) are very different from pedicures for adults. During the process, the side rollers are gently cleaned with a special softener. The cuticle is not disturbed because the matrix is still very close to it. The nails are shaped accordingly and, if necessary, the soles are polished.
Recommendations for the use of grooming products for teenagers
At the first signs of hyperhidrosis, you should use Terra or Comfort powder. These absorb excess moisture well and have deodorizing and antibacterial properties.
Consequences of onychocryptosis in children
If onychocryptosis is suspected, it is advisable to consult a competent specialist doctor in order not to aggravate the situation and reduce the risk of possible complications. It's important to remember that ingrown nails in children are often the cause of infection of the affected area, leading to an abscess. A podiatrist can help maintain normal nail growth and prevent ingrown nails.
If not treated properly, onychocryptosis can also lead to abscesses, fungal infections, bone infections and general blood poisoning. In such cases, treatment can last up to several months.
In immature children, the infection can spread quite quickly and have unpleasant consequences. This is especially dangerous for the health of a weakened child, e.g. B. a child with diabetes or another serious illness.
The problem of the ingrown nail is always approached with care in pediatrics, recommending immediate treatment and a number of necessary therapeutic measures.
Treatment options for an ingrown toenail
The disease is classified according to its severity. Depending on the severity, medical treatment of ingrown toenails in children is divided into conservative, orthopedic, curative and surgical treatment.
Conservative treatment
Outpatient treatment is simple but produces measurable results in the early stages of ingrown toenails in children. For this purpose, you should not waste time and use the services of a podiatrist who is well versed in the treatment of onychocryptoids. The specialist will conduct the correct treatment and provide recommendations for personal care.

Many problems can be avoided by observing hygiene rules, using modern cosmetic products and warm foot baths. In some cases, the specialist will show you how to properly apply band-aids at home to open deep shafts.
If pain occurs, you should not hesitate, because a podiatrist can only help in the initial stages.
surgical method
If pustules and granulation formations appear, which indicate a neglected condition, surgical treatment is carried out. It is important to choose a good specialist who will correctly assess the need, answer all questions and competently conduct the procedure.
There is no consensus among medical specialists. Whether surgical treatment is advisable, especially in benign forms of the disease, depends solely on the doctor's experience.
The main types of surgical treatment include:
- Resection of the marginal nail plate. This type of surgery is performed under local anesthesia. The ingrown nail piece is freed from the damaged skin, excised and the surgical wound is sewn up with blind stitches. This method is fraught with complications: there is a high risk of injuring the growth layer, which will lead to its pathological deformation. The operation is quite complicated and there is a risk that it will happen again later.
How does a child grow and what are growing pains?
The rate of growth is highest in the womb and gradually decreases after birth until puberty, after which it increases again rapidly.
Great attention is paid to the growth of the newborn because of its importance in the overall assessment of development. In the first year of life, a child usually grows by 25 cm. Between the ages of 1 and 4 the child grows about 10 cm per year and by the age of 4 has reached a size of 100 cm ('Meterkind', ie with a height of 1 m and a weight of about 16 kg). After that, growth slows down somewhat (about 5 cm per year) until puberty. Puberty is characterized by rapid growth (10-15 cm per year) and is caused by the influence of pituitary somatotropic hormone (PTH) and increased production of sex hormones (androgens and estrogens).
Somatotropic hormone, insulin-like growth factor 1, sex steroids and thyroid hormone are important hormonal regulators of growth. Interestingly, reduced insulin levels or existing insulin resistance in adolescence have a negative effect on growth. Of greatest interest are the hormone-like peptides (growth factors) synthesized in the body. Their interactions with the corresponding receptors trigger cascades of cell signaling reactions that specifically regulate gene activity. More and more growth factors are being discovered and information about their properties is accumulating rapidly.
Growth will continue as long as the epidermal growth plates remain. Sex hormones (estrogen, testosterone) cause the epiphyseal growth plates to close in late adolescence. The cartilage is completely replaced by bone and natural growth is stopped.
The final human height depends on the size of the long bones (tibia and femur). Androgens help to close the epiphyseal growth zones, stopping growth.
Growing pains are not recognized by all physicians, are not treated as a diagnosis, and are clinically insignificant leg pains.
What are growing pains like?
Children describe growing pains as painful, stiff leg muscle pains above or below the knee, sometimes below the knee (the pain is usually localized to the knee and/or lower leg). Usually both legs are affected. Some children complain of abdominal pain or headaches during these episodes. It should be noted that these are intermittent pains that usually appear in the evening or at night; sometimes a child suddenly wakes up in the middle of a deep sleep at night and complains of leg pain. Growing pains never occur during the day. When it comes to growing pains, regardless of the severity of the night pain attack, the child always feels good in the morning.
The disease is often hereditary. Growing pains are common in preschool and school age children. About half of all children complain of unpleasant, painful sensations in the legs during the period of active growth. They are slightly more common in girls than in boys. Certain risk factors have been identified. This includes running, climbing or jumping during the day.
What kind of skin itching is there and what causes it?
A distinction is made between localized and generalized itching of the skin.
Localized itching of the skin
more localized Term for an itching concentrated in one place. It is most common in the area:
- anus (with hemorrhoids, worms, anal inflammation);
- external genitals (in diseases of these organs, in women also during menopause);
- Hair on the scalp (pediculosis).
Local itching can also be caused by dry skin, insect bites, and allergic reactions.
itching all over the body
more general Generalized itching (i.e. spreading throughout the body) can have a number of causes, including.
- liver disease (including viral hepatitis);
- endocrine disorders (e.g. diabetes)
- certain blood disorders;
- skin diseases;
- mental disorders;
- Certain types of cancer.
Which doctor should I go to if I have itching?
In case of localized itching, a dermatologist should be consulted. Sometimes an allergic origin of the itch is revealed, in this case a visit to an allergist-immunologist is recommended. If there is itching in the genital area, a gynecologist should be consulted.
If the itching of the skin is generalized, you should first consult your family doctor. A full examination will likely be needed to determine the cause of the itching.
Your GP's qualified and experienced doctors will help you determine the cause of your itching and prescribe an effective treatment.
Do not self-treat. Contact our specialists who will make a correct diagnosis and prescribe treatment.
Read more:- hole in the heel.
- heels in teenagers.
- What the surgeon examines in teenagers.
- How a child's feet grow at the age of one.
- Heels for girls 12.
- The outer arch of the foot hurts, why.
- Why are the big toes crooked?.
- Shoes for swollen feet.
