When the distal biceps tendon is ruptured, patients usually feel severe pain in the elbow joint. The tendon usually tears when lifting heavy objects. The mobility of the elbow joint is usually not impaired after a tendon rupture. Swelling, soft tissue loss in the ulnar fossa, and rupture of the biceps tendon and deformity of the biceps brachii are common.

- Rupture of the biceps at the elbow
- Our team
- Maxim Bessarab
- Artak Mikhaylovich Kharchyan
- Genrikh Olegovich Krasnov
- Classification of injuries
- An important tip from the editors!
- Treatment of rupture of the long head tendon of the biceps brachii
- History and physical examination
- Radiological diagnosis of biceps tendon rupture
- Treatment of anterior cruciate ligament tears in the clinic
- Prevention of anterior cruciate ligament rupture and medical advice
- Prevention of joint fractures and injuries and medical advice
- Methodology: the main steps
- Efficacy of surgical treatment of ACL rupture
- Types of tendon surgery treatment
- Tenodesis of the distal part of the biceps
- Removal of a hemangioma
- Diagnostic evaluation of tendonitis
- signs
- Treatment
Rupture of the biceps at the elbow
A rupture of the distal biceps brachii tendon is defined as partial or complete detachment from its attachment point at the radial bone. This injury is more common in middle-aged men who do heavy work or play sports. The rupture of the distal biceps tendon is not as rare as previously thought. In the vast majority of cases, patients with this type of injury require surgery by a specialist.
Failure to operate will inevitably result in reduced upper limb strength and a significant cosmetic defect in the shoulder region. This article discusses the causes and factors behind the rupture of the distal biceps tendon, as well as the symptoms, diagnosis, and treatment of this injury.
The distal tendon of the musculus biceps brachii attaches to the protuberance of the radius bone. Proximal, that is, from above, the biceps muscle is connected to the scapula by two tendons. The biceps muscle is quite strong and spans the forearm over the humerus from the shoulder blade.

As the biceps contracts, it flexes the upper limb at the elbow. When the tendon ruptures, function of the entire upper limb and elbow joint can be affected. Flexion of the elbow and supination (outward rotation) of the forearm are usually limited. Patients with a biceps tear have poorer exercise capacity. The distal biceps tendon usually separates from the radial bone.

Important nerves and vessels are located in the immediate vicinity of the distal insertion of the biceps tendon on the forearm. The consequences of tendon insertion surgery on the radial bone are serious and sometimes lead to complications.
Our team

Maxim Bessarab
- md
- Specialist in arthroscopic and minimally traumatic joint and foot surgery
- dr Bessarab is very experienced in all conservative and surgical
and surgical treatment of sports injuries - He performs more than 500 arthroscopic surgeries a year.

Artak Mikhaylovich Kharchyan
- Orthopedic traumatologist of the highest category
- Candidate of Medical Sciences
- Head of department of a large city hospital in Moscow.
- Expert recognized in Russia in the field of joint endoprosthetics and the treatment of bone fractures using gentle methods.
- dr Kharchian conducts more than 400 high-tech operations a year

Genrikh Olegovich Krasnov
- traumatologist and orthopaedist
- Member of the Russian Association of Orthopedic Traumatologists and the Russian Arthroscopic Society.
- Experienced in methods of conservative and surgical treatment of joints
- Specialized in orthopedic orthotics, shock wave therapy
- Performs up to 300 arthroscopic surgeries per year
Classification of injuries
Injuries can be classified according to the degree of fiber deformity:
- Grade 1 violation; also known as 'ligament strain' because only a small percentage of the tendon fibers are damaged;
- Grade 2 injury: This injury is characterized by the fact that the ligament is not functionally damaged but a large percentage of the tendon fibers are damaged;
- Grade 3 Injury: This is the most severe and dangerous variant as the ligament is torn and all the fibers are damaged. Another possibility is that the ligament snapped at its attachment point. It becomes clear why the ligament can no longer fulfill its actual function when it is so badly damaged.
An important tip from the editors!
Everyone uses cosmetic products, but studies have shown terrible results. The shocking news of the year is that 97.5 % of popular shampoos contain substances that are toxic to our bodies. Check your shampoo for sodium lauryl sulfate, sodium lauryl sulfate, coco sulfate, and PEG. These chemicals can damage your strands, leaving them brittle, dry and misshapen.
Worst of all, this crap collects in the pores and blood in the organs and can cause cancer. We strongly advise against using products containing these substances. Our editorial experts tested shampoos, and the products from Mulsan Cosmetic came out on top.
The only manufacturer of pure natural cosmetics. All products are manufactured under strict control of certification systems. We recommend visiting the official online store mulsan.ru. If you have doubts about the naturalness of the cosmetics, check the shelf life, it shouldn't be more than 11 months.
Treatment of rupture of the long head tendon of the biceps brachii
Surgical treatment of the rupture of the tendon of the long head of the biceps brachii
Surgical treatment in the hospital is recommended for men of working age: The distal end of the torn tendon is immobilized transversely in the area of the intercostal sulcus or slightly lower. The limb is immobilized with a thoraco-radial cast for 5-6 weeks.
Approximate length of incapacity for work
The return to work takes place after 6-10 weeks.
History and physical examination
After hearing your complaints and taking your medical history, the doctor will examine the shoulder joint. In the case of a complete rupture of the biceps tendon, the diagnosis is usually immediately 'visible' by the characteristic deformation of the muscle.

Fig. A rupture of the biceps tendon is easily recognized by the characteristic contracture of the muscle.
Diagnosing a partial tear is more difficult. Your doctor may ask you to bend your arm at the elbow and contract your biceps muscle. If you feel pain at this point, it could be a partial tear of the biceps tendon.
Your doctor will also consider other possible shoulder joint problems when choosing the best treatment plan. The biceps tendon can also tear in the elbow joint area, but this is less common. When the biceps tendon tears in the area of the elbow joint, you will see a 'slack' in the tissue over the elbow fossa. Your doctor will look closely at this area during the exam.
Biceps tendon tears are commonly associated with conditions such as rotator cuff injuries, impingement, and tendonitis. Your doctor may recommend additional tests to diagnose these problems.
Radiological diagnosis of biceps tendon rupture
X-ray picture. X-rays cannot show the soft-tissue structure surrounding the biceps tendon, but they can help diagnose other underlying problems with the shoulder or elbow.
Magnetic resonance imaging (MRI). This examination serves to assess the anatomy of the soft tissue structures and to diagnose partial or complete tendon ruptures.
Treatment of anterior cruciate ligament tears in the clinic
This treatment helps reduce swelling and pain.
- Application of cold compresses.
- puncture of the knee. This is necessary if the tear has caused internal bleeding.
- Applying a cast or splint. This helps to immobilize the limb. As a rule, physical activity is restricted for 4-6 weeks.
- Taking nonsteroidal anti-inflammatory drugs. These relieve the pain and allow the acute inflammation to subside.
If necessary, bed rest or walking with crutches is recommended. As soon as the cast or splint is removed, a complex of rehabilitation measures is carried out. The aim is to restore the muscles and function of the knee. If necessary, physiotherapy treatments are prescribed. The doctor can then prescribe physical therapy treatments for the patient. The exercises are individually tailored to each person and only performed under the supervision of a physiotherapist.
These exercises are performed only when conservative measures are ineffective or inefficient. Today, special attention is paid to arthroscopic plastic surgery. This procedure is minimally invasive and avoids damaging healthy tissue.
Key benefits of arthroscopy include:
- High precision of the intervention. A special camera is used during the operation. Thanks to the camera, the surgeon can see even the smallest damage in the joint. This enables an uncomplicated operation and shortens the rehabilitation period.
- A lengthy preparation of the patient is not necessary. A plaster cast or complicated orthopedic constructions are not required before the operation.
- Minimal aesthetic compromises. After the operation, only a small scar remains on the knee, which is hardly noticeable to others.
- Minimum hospital stay. The patient stays in the clinic for only 2-3 days.
- Rapid rehabilitation. Already 1-1.5 months after the operation, the patient is able to walk independently.
Prevention of anterior cruciate ligament rupture and medical advice
To prevent damage to the anterior cruciate ligament, our trauma surgeons recommend the following
- Strengthen and support the band. To do this, do a few simple exercises.
- Lead a healthy lifestyle and eat a healthy diet. Eat a healthy diet and get enough protein, vitamins and other nutrients.
- Get enough rest, especially if you are doing strenuous physical activity. Joints can only recover by themselves after exercise if you get enough sleep.
- Check your body weight. Excessive weight puts additional strain on the ligaments.
It is also very important to visit the doctor regularly. Your doctor will continually monitor the condition of the anterior cruciate ligament (ACL) and provide recommendations for offloading if you experience excessive strain.
Important!!! It is particularly important to consult a specialist if you experience discomfort in the area of the ligament under stress or at rest and complain of pain, swelling and other signs of pathological changes.
To make an appointment with a traumatologist, use the special form on the site or call the number provided.
Prevention of joint fractures and injuries and medical advice
This is how you prevent joint injuries and torn ligaments
- When engaging in sports and other physical activities, be careful to avoid injury.
- Treat all joint problems in a timely manner.
- Treat even minor injuries in good time.
- In the event of increased stress, consult your doctor regularly.
If you would like to have joint injuries and torn ligaments treated, give us a call or submit an inquiry online. Our specialist will schedule you an appointment with a trauma surgeon that suits you.
Methodology: the main steps
Bandoplasty does not require any special preparation on the part of the patient. It is only necessary to abstain from food for a few hours until the planned procedure. The rest of the preparation is done by the medical staff. The surgical intervention is carried out in several stages:
- application of general or spinal anesthesia;
- treatment of the skin on the knee with antiseptic solutions;
- Inserting the arthroscopic instruments through one or more small punctures/incisions;
- Evaluation of the lesions, demarcation of the surgical field;
- Extraction of non-reparable tissue if necessary, repair of meniscal injuries;
- Insertion of grafts, fixation;
- Cleaning the wound surface with antiseptics;
- sew up.
Depending on the method of ligament surgery, the severity of the injury, and the presence of concomitant injuries, it may involve additional steps.
Efficacy of surgical treatment of ACL rupture
Ligament repair is often the only surgical treatment that can restore full function of the knee joint. According to statistics, the therapy is successful in 85-93 % cases. More than half of the operated professional athletes were able to return to active training without impairment. Experienced trauma surgeons have identified several reasons why the bandoplasty was not as successful as planned:
- Rotational stability was underestimated, other damage to knee joint structures was not repaired;
- plasticity was performed with technical errors, without taking into account the individual anatomical features of the patient;
- the biological prerequisites for the acceptance of the transplant were disturbed, e.g. B. due to incorrectly selected fixation elements;
- no individualized and appropriate rehabilitation was carried out.
In many cases, failure to achieve the predicted outcome of ligamentoplasty was due to inadequate medical supervision of graft attachment.
Types of tendon surgery treatment
When choosing the best type of tendon graft for a patient, the doctor considers the type and location of the injury. The following surgical techniques are used in modern traumatology
- tenorrhaphy. If a tendon tears, the tendons are sewn up. Silk, nylon, capron thread and thin tantalum wire are used as sutures.
- tendoplasty. Tendonoplasty is used to repair damage caused by severe degenerative or inflammatory diseases. Autoplasty uses patient tissue, alloplasty uses synthetic implants, and xenoplasty uses biomaterial of animal origin.
- tenolysis. Reconstructive surgery to remove adhesions from traumatic scars, including those involving the periarticular capsule.
- tenodesis. An operation in which a diseased tendon is relocated and converted into a passive ligament. It prevents deformation and/or excessive mobility of the affected joint.
- tenotomy. A surgical technique in which the tendon is cut to lengthen it.
- transposition. In tendonoplasty, the tendon is detached from its permanent attachment point and attached to a different location. This common procedure closes post-traumatic damage to another deep flexor or extensor tendon and corrects a neurogenic deformity caused by damage to the nerve trunk.
Tenodesis of the distal part of the biceps
Tenodesis tendonoplasty is performed in cases where the tendon is detached from the underlying bone. It is repaired by making a small cut in the front part of the biceps. In tendonoplasty, a cortical nodule and interference screw are used to attach the elastic attachment to the bone.
Removal of a hemangioma
A tendon plication is necessary when tendons are compressed or otherwise damaged by hypertrophy. The tumor-like mass is removed using traditional open-access techniques or arthroscopically. In the past, regional anesthesia was used in the trauma ward.
Diagnostic evaluation of tendonitis
Initial diagnosis is based on physical examination and a series of functional tests. It can be confirmed by an instrumental examination:
- Ultrasound examination of the body area with the injured tendon;
- MRI, which is particularly insightful for assessing the condition of soft tissue structures;
- X-rays to rule out or confirm concomitant bone injury;
- Arthroscopy to study the condition of the articular cavity.
Based on the interpretation of the results of diagnostic tests, the doctor determines the most effective therapeutic measure.
signs
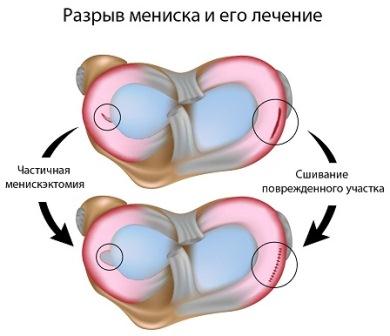
A meniscus tear causes swelling, restricted movement and pain. After a tear, patients feel unstable in the knee joint and experience pain when performing certain activities. Unfortunately, many people do not go to the doctor immediately, but wait until the injury heals 'by itself'. In this case, it is possible to relieve the pain, but only after people have returned to their normal level of activity. If the meniscus is only slightly damaged, it's possible to live comfortably and experience pain only when squatting or doing other activities that put stress on the knee joint. However, there is always a risk that the meniscus will tear permanently after some time.
The type of meniscus tear determines the need for surgery. For example, a 'knob grip' type tear, where the meniscus is almost completely torn off, can block movement. The type of injury to the knee joint is determined by the doctor using special clinical tests, MRI and X-rays.
Treatment
Treatment for meniscus tears depends on the type of meniscus injury. The doctor may stitch the meniscus or remove the damaged area. Repair of a torn meniscus is best performed through arthroscopic surgery. Before arthroscopy, these operations were performed in an open manner. However, open surgery is a very invasive method that often leads to complications such as osteoarthritis. In some cases, osteoarthritis occurs 10-15 years after open surgery. The open operation has changed the joint in such a way that nothing other than endoprosthetics can help with the development of arthrosis. The fewer interventions in the joint, the better.
In addition, after arthroscopic surgery, the patient recovers faster, a long hospital stay is not required, and the rehabilitation period is shorter. Patient recovery and rehabilitation time after arthroscopy is reduced by a third, if not by half. After the arthroscopy, the reconstruction of the joint begins the next day and can take up to a week, depending on the damage to the joint, the prospects for healing and the age of the patient. Bed rest is required for the first 24 hours after surgery. You can stand up, but only on crutches, with little weight on the ankle. After this period, the doctor decides on conservative methods of treatment. Physical therapy, physiotherapy, cold therapy, exercise bikes, swimming, etc. may be prescribed to the patient. A return to normal life is possible three to four weeks after the operation.
Read more:- Thigh tendon rupture.
- Rupture of the ligaments of the ankle.
- Rupture of the medial collateral ligament.
- Collateral ligament rupture.
- Rupture of the radial-clavicular joint.
- How much does knee surgery cost?.
- How long it takes for the ligaments to heal.
- How much does shoulder surgery cost?.
