An isolated type A fracture without displacement is stable and requires minimal fixation until the fracture heals with a tight bandage or orthosis, primarily for reasons of comfort.

- Necessity of fibula fixation in tibia fractures 2016.02.05 Necessity of fibula fixation in tibia fractures
- Borderland Orthopedics Kiev, Ukraine 2015.07.02 Borderland Orthopedics Kiev, Ukraine
- Treatment of dislocation of the sternum end of the clavicle 2014.10.29 Treatment of dislocation of the sternum end of the clavicle
- Treatment of a luxated clavicle 2014.10.29 Treatment of a luxated clavicle 2014.10.29 Treatment of a luxated clavicle
- Treatment of fractures of the lateral end of the clavicle 2014.10.29 Treatment of fractures of the lateral end of the clavicle
- Intracranial internal fixation of collarbone fractures 2014.10.29 Intracranial internal fixation of collarbone fractures
- Treatment of diaphyseal fractures of the clavicle 2014.10.29 Treatment of diaphyseal fractures of the clavicle
- Treatment of collarbone fractures and dislocations of adjacent joints 2014.10.29 Treatment of collarbone fractures and dislocations of adjacent joints
- Postoperative treatment of scaphoid fractures 10/29/2014 Postoperative treatment of scaphoid fractures
- Surgical approaches in the treatment of scapula fractures 2014.10.29 Surgical approaches in the treatment of scapula fractures
- Home ' Directions ' Lower Limb Fractures ' Treatment of Fractures of the Foot Bones ' Treatment of Fractures of the Ankle Bone.
- Pelvic fracture with displacement
- Treatment of a heel head fracture
- Class B: Type II fractures of the calcaneus neck
- clinical picture
- X-rays
- Conclusions.
- Pathophysiology of Fractures
- Treatment
- Open fracture
- First aid
- Causes of radial head fractures
- symptoms
- Anatomical Features
- mechanism of injury
- How is the ankle repaired after a fracture?
- Physical therapy and massage for the ankle after a fracture
Home ' Directions ' Lower Limb Fractures ' Treatment of Fractures of the Foot Bones ' Treatment of Fractures of the Ankle Bone.
For fractures of the talus without dislocation immobilization with a circular plaster cast up to the knee joint is indicated, and a splint is inserted into the plaster cast. A dosed load is possible after 3 weeks, the duration of the immobilization is 6-7 weeks.
Restoration of ability to work within 1.5-2 months.
For an isolated fracture of the posterior femoral process The immobilisation in the soleus flexion position is carried out for 6 weeks. However, prolonged immobilization in the equinus position of the foot prolongs recovery of ankle function significantly. For this reason, some authors recommend surgical treatment of a posterior process fracture, that is, its removal.
Pelvic fracture with displacement
Class B: Type I fracture of the ankle head. This injury is usually the result of a direct impact, e.g. B. a fall on a fully extended foot. Power is transmitted from the forefoot to the talus, which rests on the front edge of the tibia.
The following symptoms are usually observed in the patient PainsPain, swelling, congestion, and tenderness on palpation of the talar head and talicofemoral joint. Ankle mobility is normal, although inversion of the foot increases pain over the talofemoral joint.
A normal projection scan is sufficient to diagnose this fracture.
Treatment of a heel head fracture
The emergency treatment for these fractures includes ice packs, elevating the limb, immobilization with a thick, tight bandage, and referral for an urgent doctor's visit. Some orthopedists prefer early partial weight bearing based on tolerance, while others recommend a short boot cast for 6-8 weeks followed by supine for 12 weeks. Some surgeons recommend a weight-bearing cast for 6-8 weeks as a treatment option.
fractures fractures of the head Fractures of the talar head can be complicated by the development of osteoarthritis or chondromalacia.
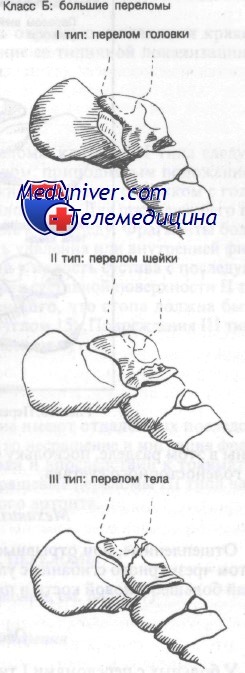
Class B: Type II fractures of the calcaneus neck
typically, fractures usually occurs with acute hyperextension of the foot and ankle and is commonly associated with automobile accidents and falls from height. The hyperextension pushes the neck of the talus into the anterior border of the tibia. Continuation of this force can result in ligament rupture, fragment dislocation, underfoot dislocation, or dislocation of the talar shaft.
The patient suffers from marked overpronation of the foot associated with pain, swelling, and severe tenderness to slight palpation or movement.
This fracture can be best best seen through on a normal x-ray in lateral projection. Oblique projections can be helpful for slight subluxations or dislocations.
clinical picture
Ankle fractures are common in athletes (skiers, soccer players, rock climbers) and also in older people with osteoporosis.
In the medical history, patients report an acute twisting of the foot, followed by severe pain and an inability to stand on the foot. This clinical picture is often indicative of an injury more serious than just a sprain. The joint is swollen and there may be deformity. The location of the pain is clinically important; if both ankles are involved, a double injury (bony or soft tissue) should be suspected.
X-rays
X-rays should be taken from at least three views: anterior, lateral, and oblique. The level of the fracture is clearly visible on the x-rays. The mechanism of the injury can be reconstructed on the basis of the X-ray images and the correct treatment can be planned and carried out.
The swelling is usually significant and increases rapidly, especially in severe injuries. If the swelling lasts for several hours, then the final tactic is postponed for several days. During this time, the limb is elevated so that the swelling can subside. This can be accelerated by active footwork (it also reduces the risk of deep vein thrombosis).
Fractures, unlike ligament injuries, are detected on X-rays. However, an experienced doctor can also detect indirect signs of soft tissue injury on an x-ray. These signs include widening of the intercondylar space, asymmetry of the joint space, and displacement of the plateau.
As with other intra-articular injuries, ankle fractures must be accurately reduced (translated) and secured in the correct position for healing. An unrepaired talar displacement or residual step on the articular surface increases stress on the ankle and predisposes to osteoarthritis.
Fractures in the ankle area are often unstable and may require surgical treatment.
Conclusions.
1. A method was developed and put into practice for the treatment of complicated fractures and dislocations of the talus (types III, IV, V) based on immersion osteosynthesis with pins or screws and external fixation with modular pins and nails with subsequent removal of the fixation pins and insertion of a rotation device.
(2) The advantages of the proposed technique are the strain relief of the articular surfaces of the ankle and ankle-foot joint (elimination of myocompression), early functioning of the ankle joint by the articulating device, the possibility of axial support of the limb in the splint and a dosed Loading of the foot while maintaining the gait stereotype.
3 In the treatment of crush fractures and plate dislocations, the above advantages of the external fixation apparatus outweigh the disadvantages of the external design, which is the reason for using the developed method.
1 Nikitin PV Diagnostics and treatment of foot bone injuries – K.: Phoenix, 2005. – 192 s.
2. Nikitin PV Results of treatment of patients with fractures and dislocations of the talus // Journal of Orthopedics, Traumatology and Prosthetics – 2004. – No. 3 – p. 3037.
3 Palamarchuk VV Treatment of fractures, ankle bone fracture dislocations, subtalar dislocations of the foot and adjacent injuries: dissertation, – X., 2002, – 21 p.
4 Canale ST, Kelly FV. Fractures of the calcaneus neck: a long-term evaluation of seventy-one cases // J. Bone Jt. Surg – 1978. – Vol. 60A, No. 1 – p. 143156.
5 Hawkins LG Fractures of the neck of the talus // J. Bone Jt. Surg. surge – 1970 r. – Vol. 52A, no. 5. – p. 9911002.
6. diGiovanni CW, Patel A, Calfee R, Nickisch F. Osteonecrosis in the Foot // J. Am. Acad. orthopedic Surg-2007,-15,-208217.
7 Fortin PT, Balazsy JE, Talar fractures: evaluation and treatment // J. Am. Acad. orthopedic surge 2001. – 9. – 114127.
Pathophysiology of Fractures
OpenThere is a tear in the covering skin and contact between the fractured bone and the surrounding area through the wound lumen.
pathologic fractures Occur when a small or minimal force causes fracture of an area of bone originally affected by disease (eg, osteoporosis, cancer, infection, bone cysts). Osteoporosis Osteoporosis is a progressive metabolic disease of bone that reduces bone mineralization (bone mass per unit volume) and disrupts bone structure. Read more These fractures are often referred to as stress fractures or pathologic fractures.
Stress Fractures Stress fractures are small, incomplete fractures that often affect the shafts of the metatarsal bones. They are the result of constant stress. Stress fractures are not. Read more that result from the repeated application of moderate force can occur, for example, in long-distance runners or marching soldiers carrying heavy loads. Normally, bones damaged by moderate-force micro-injuries regenerate spontaneously during periods of rest, but repeated force application to the same site encourages further injury and causes micro-injuries to propagate.
Treatment
The bones heal at different rates depending on the age of the patient and concomitant diseases. For example, in children they heal much faster than in adults; in diseases that affect peripheral blood flow (e.g. diabetes, peripheral vascular disease), healing is slower.
Fractures heal in 3 overlapping phases:
The inflammatory phase occurs first. A hematoma forms at the fracture site and a small portion of the distal bone is resorbed. If the fracture line is not initially visible (eg, in some nondisplaced fractures), it usually becomes visible 1 week after injury when a small amount of bone has been resorbed.
During the reconstructive phase A callus forms. New blood vessels form, allowing cartilage to form along the fracture line. Immobilization (such as a splint) is required during the first two stages to allow new blood vessels to form. The repair phase ends with the clinical healing of the fracture (ie there is no pain in the fracture area, the injured limb can be used without pain and clinical examination shows no displacement of bone fragments).
The rebuilding phase includes the ossification of the originally cartilaginous callus as well as the destruction and repair (remodeling) of the bone tissue. During this phase, patients should be encouraged to gradually regain movement of the injured limb, usually with weight.
Open fracture
Easily recognized by the trauma surgeon as the bone fragments are clearly visible due to the soft tissue destruction. This is the most severe stage, as infections and pathogenic bacteria quickly invade the open wound. Untimely treatment can lead to gangrene. Left untreated, gangrene can be fatal.
The bone is damaged without tearing the soft tissues or allowing infection. Often the bone is misaligned, so specialists use X-rays to make an accurate diagnosis. Fractures that cause acute pain and impair limb mobility also fall into this category. If left untreated, the fracture can deform the bone.
First aid
If a fracture is suspected, the injured person should be completely sedated, immobilized and the fracture site fixed. The arm can be wrapped around the torso with a scarf, bandage, or with a thick board or piece of rebar. The leg can be connected to the rebar, a board or a sound leg.
If a spinal fracture is suspected, place the person on a firm wooden board or other firm, flat surface. Depending on the severity of the injury, either take the casualty to a trauma center immediately or call an ambulance. In the multi-specialty clinic of the CELT, fractures are treated by highly qualified trauma surgeons.
Causes of radial head fractures
The most common causes of fractures of the radial head are accidents in the home/work/sports. Less commonly, fractures are caused by osteoporosis. The extent of the fracture of the radial bone depends on the type/location of the traumatic impact:
- Fractures of the lower third of the radius bone - the main cause is a fall from a person resting on the palmar/dorsal surface of the wrist, less commonly a severe blow to the dorsal surface of the wrist.
- Fractures of the middle third of the wrist are mainly caused by a blow to the radial side of the forearm.
- Upper third fractures result from a fall onto an outstretched hand.
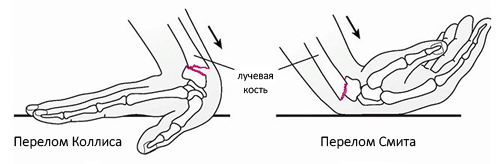
Fractures in the typical position without displacement/dislocation are most often caused by a straight-arm fall. Depending on the type of displacement, different types of injuries are distinguished Colles fracturesFractures in which the distal part of the arm is displaced backwards and Smith's fracturesFractures where the distal fragment is displaced towards the hand (see figure below).
The main cause of a fracture of the radial bone in the diaphyseal area is a blow to the radial side of the forearm. A radial bone fracture in the head area is most commonly caused by a fall on an outstretched hand. In 60 % cases, there is simultaneous damage to other anatomical structures contortion Dislocation of the forearm bone. An anastomotic fracture of the radius bone with dislocation of the wrist of the ulna? (Galeazzi injury) is caused by a fall on the non-flexed forearm with simultaneous compression of the swollen soft tissues, veins, arteries and nerves.
Factors such as the following greatly increase the likelihood of fracture:
symptoms
The main symptoms of a radial bone fracture include:
- Pains. Patients complain of a stabbing pain that worsens when they try to twist (perform rotational movements) their forearm. Pain syndrome is especially pronounced with open fractures, especially with displaced fragments.
- Creping Bone Fragments. Appears under the fingers when trying to move the bone as a characteristic crunch. However, it is not advisable to check the crunch yourself, as this can lead to even more displacement of the bone fragments.
- Local swelling of the tissue. It is caused by a cascade of reactions that contribute to an inflammatory process in which blood vessels dilate and fluid partially penetrates the tissues, causing swelling. If there is a hematoma at the fracture site, the swelling will eventually turn purple.
- Abnormal shoulder mobility. Is an absolute sign of a fracture, but can only be checked by a doctor.
- shortening of the arm. This symptom occurs in radius/elbow fractures with longitudinal displacement of the fragments.
However, each site of a radial bone fracture is characterized by specific symptoms. For example, a radial head fracture is characterized by acute elbow joint pain that worsens on palpation and attempts to flex or rotate the arm. The examination shows a deformation of the joint and a restriction of movement, hemarthrosis i swelling. A particularly strong restriction is found in rotational movements of the forearm. In cases where a fracture of the radial head is accompanied by a dislocation of the forearm, there is greater deformity, complete immobility of the joint and often circulatory and sensory disturbances (numbness in the fingers) in the distal area.
Anatomical Features
The talar bone is small and lies between the tibia and heel bone.

About 60 % of its surface is of hyaline cartilage than Os talus is involved in three joints at the same time:
- The ankle, the block ostalus with the shin.
- Talus and calcaneus - its posterior process with the heel bone.
- Talaneo-femoral – the head of the talus with the navicular bone, part of the Chopara joint.
The hyaline cartilage causes osteochondral fractures of the talus (approximately 4 % of injuries), which often result in osteoarthritis and compromised biomechanics of the foot.
The talus is encased by strong and dense ligaments that provide stability to the joints mentioned, thus preventing its fractures:
When walking and running, am os talus 100 % of body weight when walking and running, giving it a considerable, though not unlimited, margin of safety.
mechanism of injury
A fracture of the talus is usually caused by three different pathologic processes:
- Compression between the shin and heel bone. These injuries result in compression fractures of the shaft of the Ostalus.
- Hyperextension of the foot resulting in a fracture of the head and neck of the ankle bone.
- Excessive flexion resulting in a fracture of the posterior process ostalus.
These injuries result from high-energy impacts: traffic accidents, sporting events, falls from heights, etc.
The injuries are common os talus Injuries to the os talus often occur in combination with a fracture of the heel bone and damage to other bones of the tarsal, metatarsal, and distal tibia.
How is the ankle repaired after a fracture?
There are many proprietary techniques for repairing a broken ankle, but not all produce a positive result. It can be a fracture of the tibia, fibula, ankle bone, or all three at the same time. Depending on the location of the fracture, certain muscle groups, tendons and nerve tissue are affected. For this reason, ankle recovery after a fracture can only be treated individually. You need to see an experienced specialist and get comprehensive treatment there.
Before you begin healing an ankle fracture, you need to make sure that all fractures have healed and the bone has healed properly. X-rays must be taken for this purpose. The joint should then be worked on gradually to improve blood flow to the soft tissues and speed up the healing process. The easiest way to do this is with manual therapy techniques.
Physical therapy and massage for the ankle after a fracture
Physical therapy after an ankle fracture can begin as early as two weeks. Before the cast is removed, the muscles of the arch of the foot and the lower leg are particularly stressed. For this purpose, the doctor develops special series of gymnastic exercises. They increase muscle tone, which improves blood flow to the injured area and accelerates bone marrow formation.
After the cast is removed, the treatment of the ankle is continued, including the joint and its ligaments. The exercises are aimed at improving flexibility and mobility and at releasing the resulting contracture.
Proper ankle massage after a fracture, combined with osteopathy and reflexology, helps eliminate pain and stiffness and improve blood circulation. Massages should be performed by a medically trained professional. It is a fact that after a severe heel fracture, any improper movement by a massage therapist can result in severe nerve fiber injury. This can lead to complete paralysis of the foot and toes.
In our chiropractic clinic we offer you rehabilitation after an ankle fracture with physiotherapy and massage. Here you benefit from experienced doctors, special techniques and extensive equipment.
dr med., chief physician of the clinic
Read more:- The shaft of the heel bone.
- Fracture of the heel bone.
- Complete separation of the articular ends of the bones.
- tibia and fibula.
- pelvic subluxation.
- Fracture of the calcaneus of the foot.
- Fracture of the articular process of the heel bone.
- Anatomy of the heel bone x-ray.
