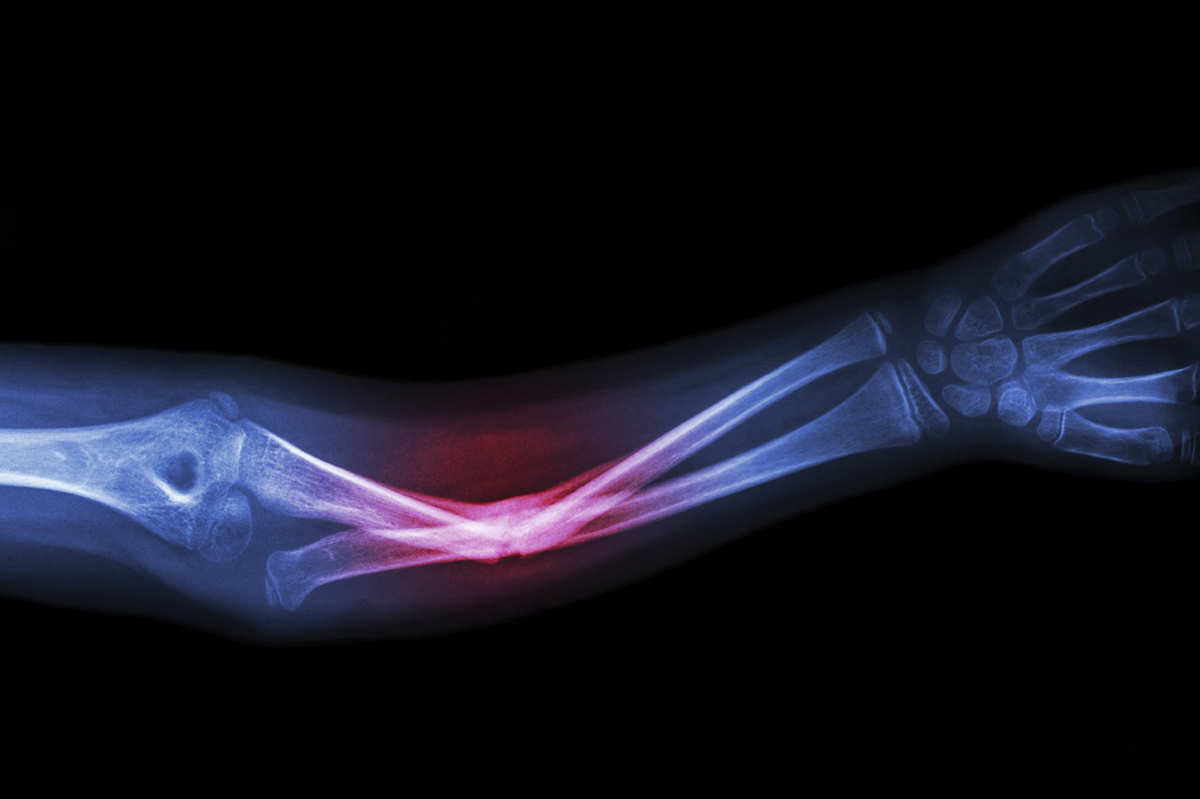
The following measures are usually sufficient to detect associated fractures X-rays Anteroposterior and lateral views are usually sufficient. In patients with impaired distal circulation, arteriography should not delay surgery. In patients with anterior or posterior displacement and a normal distal pulse, arteriography should be performed to rule out arterial damage. Patients with internal or external dislocation and normal distal pulse should be closely monitored for signs of ischemia.

- Bone dislocation in a joint
- Examination of knee dislocation
- Fractures of the shoulder bone
- Distal and proximal intra-articular fractures: causes
- Medical treatment of a sprain
- Special features of rehabilitation after hip fractures
- Hip orthoses
- Treatment of fractures of the radius bone and ankle joint
- rehabilitation and recovery
- symptoms of an injury
- causes
- Which doctor should I contact?
- What are contortions?
- How is it diagnosed?
- Dislocation fracture of the wrist
- Symptoms of injury
- Causes of Wrist Fracture
- clinical picture.
- symptoms, course
- diagnosis
Bone dislocation in a joint
Dislocations within the knee joint should be classified as an orthopedic emergency. Patients with a dislocation are rarely admitted because most dislocations resolve on their own before they reach the emergency room. Making a diagnosis is often difficult. Vascular and neurological disorders often occur after knee dislocations. With 30-40 % of fibula dislocations, the popliteal artery is injured. The fibula and tibial nerves are injured during these dislocations.
contortions are classified according to the direction of movement of the shinbone in relation to the femur. Anterior dislocations are common; in one group of cases they accounted for almost 60 % of all knee dislocations. However, in the authors' experience, posterior dislocations are more common. Tibial dislocations can be divided into anterior, posterior, internal, external and rotational dislocations, which also include anterolateral, epicondylar and posterior dislocations. They can also be divided into open and closed injuries, dislocations with fracture and simple dislocations.
Any kind contortion Each dislocation has its own specific mechanism of injury and characteristic associated injuries, which will be discussed in this article.

The anterior dislocation of the knee joint – is the most common type of sprain and is usually caused by hyperextension of the lower limbs. The typical cause is that the patient steps into a hole while walking quickly, which leads to hyperextension and dislocation. The hyperextension causes a tear of the posterior capsule, anterior cruciate ligament, and an incomplete tear of the posterior cruciate ligament. The collateral ligaments usually remain intact, but the popliteal artery is often damaged by sprains or injuries.

Examination of knee dislocation
accuracy diagnosis The diagnosis of a dislocated knee joint depends largely on the care and professionalism of the doctor.
axiomSignificant instability of the knee joint after injury should be considered a result of the dislocation until proven otherwise.
Undiagnosed Undiagnosed dislocated knee Patients may experience adverse effects. In a large study of 245 dislocations of this type, damage to the popliteal artery was found in 32 % cases. Damage to the popliteal artery must be repaired within the first eight hours of injury, otherwise up to 86 % of these injuries will result in amputation. Permanent ischemic disorders of the lower leg and foot were found in 66 % patients in whom amputation could be avoided.
axiomsAcute knee injuries complicated by instability and absence of pulse in the distal arteries should be urgently treated with revision surgery.

Swelling of the popliteal fossa due to popliteal artery injury following a sprain
spasm Popliteal artery spasm is an unlikely cause of lower limb ischemia, and angiography should not delay surgery. The distal extremity and foot are always examined, using a Doppler device to check skin temperature, pulse and blood pressure. Even if the foot is warm and there is no cyanosis, the artery can be severely damaged.
Preliminary Investigation in an acute knee injury with suspected dislocation should be limited to examination, palpation and examination of the distal neurovascular bundle. The patient has a history of injury and the chief complaint is pain. Hemarthrosis may not be present because the tear in the joint capsule allows blood to leak into the surrounding tissue. As shown in the illustration, a bulge in the popliteal fossa may indicate a damaged popliteal artery. In all patients, the distal vessels and nerves should be examined as early and completely as possible. At the same time, the ligaments should also be carefully examined. Hyperextension should be avoided as it causes unnecessary stretching of the peroneal nerve. The valgus deviation of the tibia when the knee joint is extended serves to protect the peroneal nerve from overstretching.
Fractures of the shoulder bone

The shoulder joint is one of the most complex and mobile joints in the human body. It is essentially a joint between the fairly strong upper arm bone and the shoulder blade. The humerus has a head and the shoulder blade has a socket. The entire structure of the joint is made up of numerous cartilages, ligaments and muscles of the upper limbs.
The muscles attach to special protuberances of the humerus - the major and minor tubercles. If the fracture of the shoulder joint is above the tuberosity, it is called an intra-articular fracture. If it is below the nodules, it is an extra-articular fracture, i.e. outside the joint. The humeral head often breaks down into several fragments that may be displaced relative to each other.
Distal and proximal intra-articular fractures: causes
Depending on which end of the humerus is affected, a distinction is made between proximal (closer to the shoulder) and distal (closer to the elbow) fractures.
An intra-articular fracture of the distal humerus is a serious injury diagnosed in 0.5-2 % of all patients with fractures. It accounts for up to 19 % of intra-articular fractures of the ulna.
Most distal region fractures occur in children between the ages of 3 and 11 years. A common cause of injury is falling onto an outstretched hand. An analysis of the statistics for this type of injury in adult patients shows that intra-articular fractures of the elbow also occur most often in adults as a result of a fall from their own height. The second most common cause is road traffic accidents. Isolated cases include sports (non-professional format), falls from a height and twisting of the arm by another person.
These injuries most commonly occur in older people with falls on the shoulder or elbow joint.
Medical treatment of a sprain

If you experience a traumatic sprain, you should seek medical attention as soon as possible (preferably within the first two to three hours after the injury). Otherwise, it may be difficult to reduce the injury due to swelling and reflexive muscle tension.
In the event of a sprain, the injured area must be protected, cooled and given painkillers.
If there are no complications, the dislocation is reduced closed. In most cases, the manipulation is performed under local anesthesia. General anesthesia may be used for major joint injuries or late treatment. The occurrence of complications is an indication for open reduction.
There are currently several possible techniques, e.g. B. Kocher, Janelidze, etc. The choice of a particular technique depends on the clinical case, the skills of the attending physician and many other factors.
After the joint pops, the affected area is immobilized. The duration of immobilization depends on the location of the dislocation and its characteristics.
Common sprains can only be treated through surgery.
In 2017, researchers from the Saratov State Medical University named after VI Razumovsky published a paper whose results prove that arthroscopic stabilization is a modern and highly effective method in the treatment of habitual shoulder dislocations.
Special features of rehabilitation after hip fractures
Hip fracture surgery is just the beginning of treatment. After the operation is completed, rehabilitation is required to regain full mobility. No matter how advanced and expensive a joint prosthesis is, without proper rehabilitation a person will not be able to move properly.
A dislocated hip fracture requires special attention because it is a complex type of injury. It must be treated by a qualified specialist who is familiar with such situations. Healing may take longer, but with proper treatment, this type of fracture has a good prognosis.
Rehabilitation after a fracture should begin as early as possible. The beginning of physical activity should be determined by the treating doctor. As a rule, it is already possible to sit up in bed and bend your leg slightly on the 5th and 6th day after the operation. After 2 – 3 weeks it will be possible to stand up and walk with crutches. You will gradually be able to move around using a walker or cane. If all the doctor's recommendations are followed, you will be able to walk independently after 8-9 months.
Rehabilitation after a hip fracture begins with exercises in bed and breathing exercises. The exercises are then carried out while sitting and, after a while, standing. The tissue of the hip joint will gradually regenerate and strengthen. Consistent and systematic exercise helps speed recovery and resumption of physical activity.
Other aids for rehabilitation include:
Hip orthoses
Special bandages or corsets for the hip joints accelerate the healing process. They are made of strong, elastic fabric and have rigid mounting plates. The orthosis securely immobilizes the injured joint and can be used before and after an operation. The corset has a compressing and massaging effect and has a warming effect. It holds the pelvis securely in the correct position and supports the ligaments.
High-quality treatment of hip fractures in Moscow takes place at Yusupov Hospital. Qualified traumatologists, surgeons, rehabilitators and physiotherapists with extensive experience in eliminating this pathology work here. Doctors will create the best treatment plan that will provide the fastest and safest restoration of lost function. How long it takes for a hip fracture to heal depends on the type of injury and the individual characteristics of the patient (age, presence of concomitant diseases, etc.). Doctors at Yusupov Hospital draw up an individual rehabilitation plan for each patient. In this way, the most effective treatment and best results can be achieved.
An appointment with a specialist, further information about the rehabilitation center and other questions can be requested by phone at Yusupov Hospital.
Treatment of fractures of the radius bone and ankle joint
Proper first aid for a radius fracture will avoid complications related to the injury and speed recovery from a displaced radius fracture. The aim of first aid is to relieve pain, protect the affected limb and prevent damage to the soft tissues around the fracture site. Once the fracture is closed, the limb is immobilized with a bandage. If there is an open fracture, the bleeding is stopped and the wound is treated with an aseptic bandage and then immobilized. If the fracture of the radius bone is displaced, no attempt should be made to restore the normal position of the bone fragments at the accident site in order not to damage the surrounding tissues, blood vessels and nerves.
Initial care for patients with a fracture of the radius bone takes place in the trauma clinic. The trauma surgeon assesses the victim's condition to determine the scope of further treatment and prevent the development of complications. Once the fracture is confirmed, the anatomical and functional integrity of the injured limb is restored and the hand is immobilized to prevent displacement of the bone fragments.
The traumatologist pushes the bone fragments together and fixes them with a plaster or polymer bandage. For some fractures of the radius bone, doctors perform closed or open reduction followed by immobilization with spokes, also using an external immobilization device. After treatment, patients need to restore upper limb function.
rehabilitation and recovery
Full recovery from a radius bone fracture includes restoration of bone structure and limb function (mobility and sensitivity). Even with completely adequate treatment, persistent immobility in the joints and muscles of the upper limbs makes it difficult for the patient to perform movements in the joints that were previously accessible to him. The recovery process after an injury is lengthy and requires patience and willingness to work.
The rehabilitation specialists of the Yusupov Hospital begin work on the joints and muscles as early as possible in the event of a fracture of the radius bone. The timing of the start of rehabilitation measures depends on the type of fracture and the treatment method. If the fracture is treated conservatively, finger exercises will begin after 3-5 days as soon as the swelling has subsided.
First, passive movements are carried out. With your good hand, take the finger of the broken limb and gently bend it in all joints. Stretch all fingers except the thumb in this way for 5-7 minutes, 3 times a day. After a week of training in this way, active movements are started. The patient can begin to bend the fingers independently, without the help of the other hand. It is very important that the load is distributed correctly. If pain or swelling occurs during exercises, the exercises should be stopped.
The passive movements in the fingers are started simultaneously with the active movements in the elbow and shoulder joints. The patient raises and lowers his arm and bends it at the elbow. These exercises should be performed at least twice a day for 3-5 minutes, gradually increasing the load. After 3-4 weeks, when active finger movements do not cause pain, the load on these joints increases. Take a lump of playdough and knead it in your fist. This exercise should be done as many times a week as possible. Once the cast is removed, you can begin exercising with a wrist expander. You should do the exercises at least three times a day for 5-7 minutes.
symptoms of an injury
The main symptoms of a sprain are an unnatural shape of the joint and severe pain with the slightest movement of the affected limb. Deformation or enlargement of the joint is a sign of a bone sprain. Pain syndrome is caused by compression of nerve endings, disruption of the integrity of tissues, vessels and ligaments. It is a reaction of the pain receptors, of which there are many in the bone joint area. Therefore, the first aid for a sprain is to take painkillers and ensure complete rest of the injured limb. Dangerous if:
The absence of a pulse is an indication of damage to an arterial vessel. This may have been caused by a severe dislocation of a bone. Another sign is pronounced cyanosis of the skin. Numbness in the injured limb is an indication of compression of the nerve bundle by the dislocated bones. In this case, the patient should be taken immediately to a hospital for professional treatment.
causes
Dislocations of the bones in the joint occur due to sudden mechanical influences from the outside - from a shock, a fall, a jump or the limbs becoming trapped in a narrow space. If this is not done consistently, damage to ligaments, muscles, blood vessels and nerve fibers will inevitably occur. All of this is located in the joint capsule, which surrounds the articular portions of the bones. Dislocated joints are most commonly diagnosed in people who:
- had previous limb injuries;
- had a history of joint disease;
- suffer from a disease that causes bone destruction;
- who are exposed to severe physical stress;
- play sports actively.
When providing first aid for sprains, the type of injury must always be taken into account. In open dislocations, for example, the integrity of the bone is compromised. The wound allows access to the joint capsule. It is therefore important that it is sterile. Clean gauze should be placed under the bandage or splint, and the joint itself should be bandaged. The wound should not be cleaned of dirt, but treated with antiseptics!
Which doctor should I contact?
If a limb is severely swollen, bruised or visibly deformed after a fall or blow, and the slightest movement causes unbearable, stabbing pain, you should immediately go to a medical facility. A doctor with the following specialty should be consulted:
What are contortions?
- Complete: the articular surfaces of the bones completely lose contact with each other
- partial: the surfaces are partially in contact
- closed: without broken skin
- open: with skin injuries
- fresh: less than 3 weeks after injury
- long-term: more than 3 weeks after the injury
- congenital, acquired, traumatic, pathological, habitual
Dislocations can be accompanied by injuries to other structures of the musculoskeletal system:
- Breaks, fractures (dislocations with fractures)
- Rupture of vessels or nerves
- Partial or complete rupture/strain of ligaments, tendons
- Muscle damage
How is it diagnosed?
- Assessment by a trauma surgeon
- X-rays in multiple projections for fractures
- MRI or CT scan.
CT or MRI is helpful for sprains in complex cases, such as: B. in the diagnosis of chronic injuries, suspected fractures, tears of the musculoskeletal system, sensory disorders in the affected area, etc.
With MRI, changes in the loose tissue of the joint can be better seen, while with CT, changes in the bones can be better seen.
X-rays are useless for detecting damage to ligaments, tendons, or muscles and only reveal the bones and fluid that collects around the damaged joint.
MRI Clinic Network specialists are highly experienced in interpreting CT and MRI scans for all types of sprains, including chronic sprains.
Other tests are performed to detect injuries that may occur as a result of a sprain. If vascular damage is suspected, a CT angiography is also carried out. Electromyography is used to examine nerve conduction.
Dislocation fracture of the wrist
The type of injury can vary depending on how the injury occurred. The direction and strength of the impact determines how the arm is deformed. If the fall occurred on a bent arm, the bone is displaced to the back of the arm. If the impact occurred on a straight hand, the shrapnel travels toward the thumb. A shift may occur:
Another classification distinguishes fractures not by location, but by the type of injury. Their names are associated with the names of the doctors who first described the disease in detail:
A fracture of the wrist is often accompanied by a bruise, a ligament strain or a dislocation of the joint. This usually happens when you fall. In some cases, the dislocation results in an open injury. This occurs with a very hard or sharp impact, causing bone fragments to break through the soft tissues and skin. This case is considered the most serious of the related injuries.
Symptoms of injury
The extent of disabling symptoms depends on how severe the injury was. Additional complications such as sprains, splints, soft tissue and skin damage also play a role. Often a fracture is confused with a bruise without additional signs because the external symptoms are similar. Only a doctor can make the correct diagnosis through a physical examination. A fracture can be diagnosed based on the following signs, so you can go to the hospital:
- acute pain in wrist, forearm and hand;
- Inability to move the forearm freely;
- swelling of the wrist;
- bruise on wrist;
- Abnormal bone mobility;
- Localized temperature increase;
- A characteristic crunching sound at the time of injury.
A displaced wrist fracture also results in an externally visible deformity of the hand. With an open injury, tendons and splinters are visible in the wounds.
Causes of Wrist Fracture
In most cases, this type of injury is caused by a combination of extreme mechanical stress and age-related changes in the body. In addition, bone diseases such as tuberculosis, osteoarthritis or osteoporosis can make the situation worse. Professional athletes are also at risk. The most common causes of injuries are
- falls;
- severe vertical impacts; and
- bone twisting;
- bending or twisting;
- Strain through the arm or hand;
- strong pressure;
- Contact with a hard rib.
Injuries can occur both at home and at work. In the first case, older women are more at risk, in the second case, men are at greater risk, regardless of age. In children, this type of injury is not very common due to the high flexibility of the bones.
clinical picture.
symptoms, course
A patient with a complete acute dislocation of the kneecap almost always notices the appearance of the deformity and complains about it when seeing a doctor.
If the patient tries to move the knee joint independently or with the help of others, it is sometimes possible to straighten the kneecap again. When taking an anamnesis, a patient may say that he has dislocated his knee, when in reality he has dislocated his kneecap. Dislocation can be caused by physical activity, direct trauma, or normal movement of the knee joint.
During the initial examination of the patient, deformity and swelling in the knee joint area are noticeable, and clinical examination may be difficult. As a result, the clinical diagnosis of concomitant injuries to the knee joint, such as cruciate ligament or meniscus tears, is also difficult. The limited mobility of the knee joint with a patellar luxation is due to pain and swelling of the soft tissues in this area.
When examining the knee joint, you should assess the condition of the medial condyle and the ligaments that hold the kneecap in extension, perform cruciate ligament tests, and examine the projection of the joint cavity for tenderness. Palpation of the knee joint reveals pain on the medial side of the patella, and the patient is distressed when attempting to move the patella outward. Swelling may also be seen on the medial side of the joint near the inner part of the quadriceps muscle of the thigh (VMO).
Flexion and extension of the knee joint may be limited due to pain, but if some flexion of the knee is possible, lateral displacement of the patella may be felt compared to the contralateral, intact knee joint. The lateral part of the knee joint is often painful when palpated. The doctor must also check and assess the full range of motion of the joint. In elderly patients with patellar dislocation, rupture of the quadriceps tendon proximal to the patella may occur, resulting in significant limitation of active extension of the lower extremity and soft tissue loss in this area that is difficult to detect in the presence of a hematoma. The patient should be instructed to move the extended leg forward and if this is not possible, active extension should be checked. If possible, the patient should also be examined in a standing position to determine the axis of the lower limbs and detect varus or valgus deformity [11].
diagnosis
Diagnosis of the disease or condition (group of diseases or conditions), medical indications and contraindications to diagnostic methods
2) Anamnestic examination (direct or indirect trauma to the knee joint, sudden flexion of the knee joint at home, during a fall, while dancing, playing sports)
3) Instrumental examination (X-ray, MRI, CT, ultrasound).
Dislocation of the kneecap usually occurs spontaneously. In 80 % of patients, the kneecap may dislocate spontaneously or unilaterally; the remaining patients require specialist treatment (conservative or surgical treatment). Patients with patellar dislocation experience severe pain, deformation of the knee joint due to displacement of the kneecap, limitation of movement in the joint, and impairment of the lower extremity.
Patients with spontaneous dislocation complain of pain in the front area of the knee joint, swelling of the knee joint and restricted movement [12].
The diagnosis of kneecap dislocation is made based on the symptoms, the anamnesis and the clinical examination. Various clinical tests (Fairbanks test, Bassett test) have been described to assess kneecap instability [13, 14]. Physical examination is of great importance in the diagnosis of patellar luxation, but there is currently no evidence to support the use of a specific test. Further research is needed to confirm the applicability of tests to assess patellofemoral joint instability [15].
comment. The Fairbanks test (Moving Patellar Apprehension Test) is performed in the supinated position with the patient's knee joint flexed to 20°. The inner edge of the kneecap is felt and an attempt is made to move it laterally. The patient reflexively tenses the quadriceps muscle to prevent the kneecap from dislocating.
Read more:- This is what a dislocated leg looks like.
- The lateral dislocation is.
- The key to a chopper joint is.
- How do you treat a sprained ankle?.
- dislocation of the foot.
- Diagram of a joint with and without a dislocation.
- Lisfranc joint.
- The sit bones.
