The classification is used for the most common bone tumors (osteosarcoma, Ewing's sarcoma, chondrosarcoma, etc.). The stage is determined by histological examination and instrumental data (radiographs, osteoscintigraphy, etc.).
- Bone sarcomas: treatment and diagnosis
- What are the different forms of bone cancer?
- osteosarcoma
- Ewing's sarcoma (bone marrow tumor)
- What is a disarticulation and why is it indicated?
- Indications and contraindications
- contraindications.
- Anatomy.
- Physical activity.
- Indications for hand amputation.
- Consequences of surgical failure.
- The disarticulation of the thigh is. Disarticulation of the femur is a surgical technique. Disarticulation and amputation: indications, technique, complications
- Procedure of disarticulation of the hip joint. Technique of the thigh disarticulation according to Petrovsky
- prosthesis supply
- Caused
- signs
- treatment of sarcoma
- prevention of sarcoma
Bone sarcomas: treatment and diagnosis
K bone cancer On the other hand, bone sarcomas can have different clinical courses (from very slowly growing to rapidly growing or metastatic tumors).
bone sarcoma can occur in all bones of the skeleton. However, the long bones, especially the femur, tibia and humerus, are most commonly affected. Less commonly, the pelvis, shoulder blade, and ribs are affected.
Secondary (metastatic) bone tumors are much more common than primary bone tumors. The most common metastases affect the vertebrae, ribs, pelvic bones, etc.
The most common types of cancer that metastasize to the bones are breast, lung, prostate, kidney and thyroid cancer.
What are the different forms of bone cancer?
osteosarcoma

One of the most common forms of bone cancer. This tumor occurs mostly in children, adolescents and young adults and is slightly more common in men than women. Osteosarcoma can develop in any bone of the skeleton, but tends to develop in the long bones, especially in the lower limbs, which mainly form the knee joint.
Clinically, two forms of osteosarcoma are distinguished: fast-growing tumors with an acute onset and severe pain, and slower-growing tumors with less clinical manifestation. In the case of fast-growing tumors, lung metastases can be discovered during the initial examination.
Osteosarcoma differs from other bone sarcomas in its aggressiveness. This is reflected in the tendency to rapid growth and early hematogenous metastases. Metastases usually become clinically evident 6-12 months after the first symptoms of the disease. The most commonly affected area is the lungs.
Ewing's sarcoma (bone marrow tumor)
This is the second most common malignant bone tumor in children and adolescents.
The tumor usually develops in the second decade of life and rarely occurs in children under the age of 5 years. Boys are affected more often. Unlike osteosarcoma, Ewing's sarcoma tends to affect the bony diaphyses and flat bones, including the pelvis, scapula, ribs, and vertebral bodies.
The preferred sites for Ewing's sarcoma are the long bones of the limbs and pelvis. Clinically, Ewing's sarcoma often manifests itself with fever, leukocytosis and accelerated blood sedimentation as well as pain in the affected bone. There is local congestion of the skin.
What is a disarticulation and why is it indicated?
Disarticulation is an operation to lengthen the limb along the joint line, usually without crushing the bone.
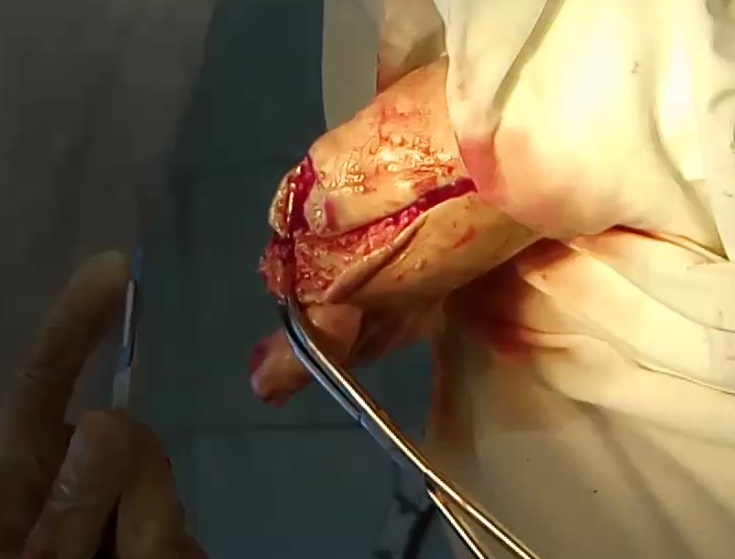
It should only be performed when there is a strong indication for it, as the resulting residual limb is uncomfortable to replace and generally causes physical and psychological discomfort. The peripheral part of the limb is removed along the gap between the condyle and the socket, and the operation is performed in three stages: first the soft tissues are removed, then the ligaments and joint capsule, and finally the wound.
Disarticulation is a radical treatment and can only be recommended when all other treatment options have failed. Unlike amputation, disarticulation does not compromise the integrity of the bone because the incision is made above the surface of the bone head.
The aim of the intervention is to remove the limb in order to prevent the development of pathological conditions, inflammation and tissue infections that can be life-threatening for the patient.
Indications and contraindications

In cases where it is not possible to save the limb, where irreversible processes are taking place around the joint and the patient's life is in real danger, the surgeon recommends hip disarticulation to replace the removed limb if possible .
A condition that can be corrected by other surgical procedures or conservative methods does not constitute an indication for disarticulation unless there is objective evidence that other treatment is unsuitable.
All indications for surgical intervention fall into three general groups. The first group includes vascular diseases associated with the development of gangrene. The second group includes trauma, and the third group includes tumors, congenital deformities, and incurable bone inflammation.
Thus, a compartmentalization of the lower limbs is made along the joint
- if the main nerves and vessels are damaged;
- if the limb has been severed
- in the presence of tumors;
- In cases where the injury connected the limb to the lobe;
- in cases of fourth-degree frostbite and burns;
- with sclerosing vascular disease of the limbs;
- when two-thirds of the soft tissue perimeter is damaged along with the large vessels and nerves;
- gangrene and sepsis;
- with a purulent process in a wound of the hip joint;
- for long-lasting trophic ulcers that cannot heal.
As for the contraindications, the main one is the presence of post-traumatic shock. The operation can be performed only after the patient has been brought out of this state by the attending physician. An acute general condition is not always a contraindication, but the patient should be stabilized beforehand if possible.
contraindications.
The main contraindication for amputation is An undeveloped line of demarcation, that separates healthy skin from dead tissue. In this situation, the surgeon does not know how high the amputation should be because the area of adequate blood supply has not yet been identified.
In general, amputation of a limb is contraindicated when it would result in impairment of quality and duration of life (situations where a person's life is at stake should not be considered). However, this contraindication does not apply to amputation of the nose.
Anatomy.
We know from anatomy classes that the number and general arrangement of the phalanges are the same in the hands and feet. The thumb has 2 phalanges and the other fingers have 3 phalanges.
The phalanges of the feet differ from those of the hands only in size, with the bodies of the phalanges of the feet being shorter, especially in the front row, and compressed on the sides.
The body of each phalange is like a metatarsal bone, convex above and concave below. On one side the head of the phalanx is slightly concave to articulate with the corresponding metatarsal and the head on the other side has a block surface to articulate with the second phalanx.
Patients should be informed about possible complications after surgery, as well as prevention and treatment. Patients should be informed about the pathogenesis of pressure zone formation in order to avoid further problems. Patients should perform daily foot skin self-examination. Patients should be referred to an orthopedist for proper footwear selection.
Using thick cotton socks and choosing the right footwear will help prevent pressure points and possible damage to the skin of the feet.
Physical activity.
- In the first 1 month after the operation, the foot should not be exposed to any physical stress.
- In a horizontal position, the operated leg should be kept above heart level if possible. Standing foot is allowed (just for balance).
- After 1 month. Post-operative exercise can be started by adding one exercise every 2-3 days, starting with 2-3 minutes and increasing to 5 minutes three times a day.
Recommended exercises:
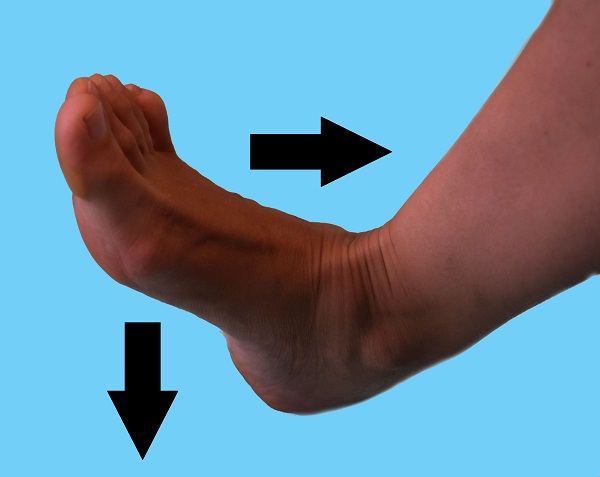 Push-ups – rhythmic movements of the foot to and from each other.
Push-ups – rhythmic movements of the foot to and from each other.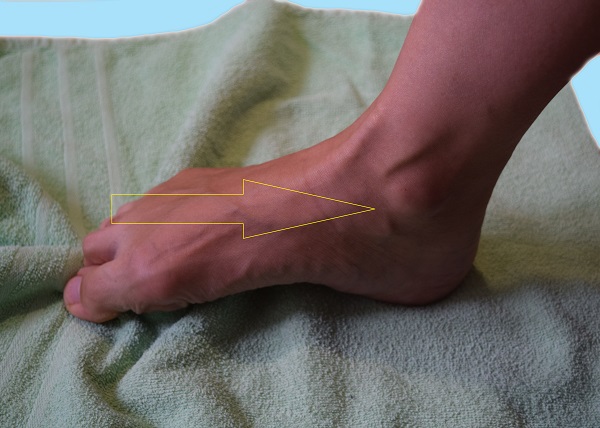 Towel - Lay a towel on the floor and use your fingers to pull it towards you.
Towel - Lay a towel on the floor and use your fingers to pull it towards you. Pinch and spread your toes together.
Pinch and spread your toes together.
If you feel pain, stop the exercise and elevate the limb.
- After 2-3 months, take an X-ray of the foot.
- Monitor your blood glucose levels (glycated hemoglobin, blood glucose measurement).
- After 2 weeks, do a complete blood and urine test.
- Order orthopedic shoes from an orthopedic company 2-3 months after the postoperative wound has healed.
The information contained in this resource is for educational purposes only and is in no way a substitute for a visit to the doctor. For people over 18 years of age.
Reprinting of extracts from articles is permitted with an active hyperlink to the site.
Indications for hand amputation.
A patient who presents to the specialist clinic (Osterhofen) knows that amputation is the very last resort to save life when all other options for rescue have been exhausted. No sane doctor would prescribe amputation alongside less dangerous and traumatic solutions. Reducing the number of amputations performed is a priority for the specialist clinic (Osterhofen).
- Immediate indications for amputation are:
- complex vascular diseases
- dry gangrene
- Third and fourth stage chronic ischemia
- Large venous thrombosis, impassable thrombus in the arterial columns of the limb.
Consequences of surgical failure.

Often, metabolic disorders develop in the hand due to blockages in the subcutaneous arteries and capillaries. This leads to a lack of nutrients and oxygen in the tissues. Cell death begins. The first symptoms are not alarming - pale skin and loss of sensitivity, occasionally cold hands. Then a rapidly growing ulcer develops. Therefore, in order to prevent the spread of the infection, the following measures are being considered amputation. The attempt to avoid amputation of the hand in favor of gentle treatment leads to a generalization of the bacterial infection to internal organs. If necrosis has developed in the finger, only the dead finger is removed. A resection of the hand is performed when the necrosis affects all fingers or the metacarpal area.
The disarticulation of the thigh is. Disarticulation of the femur is a surgical technique. Disarticulation and amputation: indications, technique, complications
Some surgeons interpret the name of this complex surgical procedure as meaning only half of it, namely the removal, the amputation of a limb, and devote the other, more important part of the operation - the creation of a new organ, the amputation stump, to the responsible Have a function and should not cause suffering to the patient - not enough attention. One could even say that the name of this complex operation, consisting of the single word 'amputation', is unfortunate as it does not convey the meaning of the entire surgical procedure. For example, 'operation to amputate a lower limb (thigh, arm at the level of...) and create a stump through...' would be more accurate. (after the name of the originator of the operation or methodology). With this in mind, amputations should only be performed by surgeons familiar with modern amputation techniques.
All the great surgeons, hundreds of names, have studied extensively in performing amputations. Here I would like to mention SI Spasokukotsky, E. Lexer, NN Burdenko who wrote the book 'Amputation as a neurosurgical operation'. In recent years there have been many valuable new proposals that have helped improve this operation. The correct closure of the amputation stump wound is not an easy task and requires some time. It is not an immediate operation, as in the past when the limb was severed by circular cutting of the soft tissues and sawing through the bone (guillotine method) or the soft tissues were divided by two strokes of a double-bladed knife that cut the limb nearby of the bone punctured and formed two 'transfusion' flaps - anterior and posterior. The bleeding was then stopped and the operation completed. There were no perfect methods of pain relief, and the earlier the surgery was done, the less pain the patient endured. The term 'amputation' was sufficient for such surgical procedures as it defined the nature of the procedure.
Procedure of disarticulation of the hip joint. Technique of the thigh disarticulation according to Petrovsky
In the supine position, a semi-oval flap is incised along the anterior surface of the thigh. The iliac vessels are exposed and tied off above the gluteal ligament. Below the gluteal ligament, the sartorius, iliacus, and pectineus muscles are divided in layers. The neurovascular bundle is exposed. The femoral nerve, femoral artery, and femoral vein are transected between the ligatures. Then the Mm. tensor fasciae latae, rectus femoris, gracilis, adductor longus, adductor brevis, adductor minimus, obturator externus and adductor magnus divided in layers.
The anterior surface of the hip joint is then exposed and opened along the anterior border of the acetabulum. The hips are moved slightly to the side and partially forward due to gravity; the round ligament of the hip prevents full displacement and is crossed with scissors so that the femoral head is fully anteriorly displaced and the posterior hemisphere of the joint is exposed. This part of the capsule is divided with a scalpel and the Mm. gemelli cut through; after additional anesthesia, the sciatic nerve is severed. The hamstrings are severed and the limb removed.
The disarticulation of the thigh can also be performed in other ways. After preliminary ligation of the femoral artery, an excessively convex posterior aponeurotic skin flap and a smaller anterior flap are excised. After the anterior lobe is detached and thrown up, the femoral vessels are ligated; the muscles at the level of the tip of the greater trochanter are crossed in the same plane; the nerves are shortened. The femur is severed at the level of the acetabulum. The muscles over the neck are relaxed, the joint capsule is opened, the bone stump is grasped with forceps and rotated to free it from the muscles, ligaments and capsule. The femoral head with the rest of the femur is removed. A final hemostasis is performed. The posterior flap of skin is sutured to the anterior flap of skin. The wound is drained. The advantage of this technique is that the scar is on the front of the stump and not on the bottom as is the case with Farabeef excision. The residual limb also has no excess soft tissue, mainly muscle, which facilitates prosthetics.
prosthesis supply
Depending on the type of prosthesis and the condition of the residual limb, there are different ways to insert and remove the prosthesis. It is also important whether both sides of the prosthesis need to be prosthetic or not. Your doctor will show you the correct way to put on a prosthesis in a special training session.
Before applying the prosthesis, the skin at the electrode attachment site should be slightly moistened. This helps reduce skin resistance and improve electrical conductivity between the muscles and skin of the residual limb and the electrodes of the prosthesis. Without wetting, it may take some time to establish good contact so that the prosthesis can be optimally controlled.
The prosthesis should be cared for and cleaned daily. To remove traces of sweat and skin particles, wipe the prosthesis with a damp cloth. Remember to clean the prosthetic glove according to the care instructions and check for tears. If you find cracks, replace the glove. If you wear an insole, care for it daily according to the instructions.
Depending on the design of your prosthesis, you may need to learn how to clench and open your hand, twist it in different directions, and bend and straighten your elbow. You can also replace parts of the prosthesis.
The next step is to practice the movements regularly. This allows you to control your prosthesis automatically, think less about how to use it and keep your muscles contracted for longer.
Use skittles, various games like Jenga, 'trees' with clothespins that can be moved vertically or horizontally. To do this, you have to constantly twist and grab something with your prosthesis.
After these control and repetition exercises, you are ready for more complex movements. The daily training is specially tailored to your daily needs. The exercises are designed to do what is important in your daily life and work.
You start with simple activities like folding a towel, then the exercises become much more complex, e.g. B. when cooking. Exercises also include dressing and undressing, opening a bottle and pouring a drink, and even dealing with your work station. Plus, being able to eat unaided with a knife and fork is a big step toward independence. You will be surprised how much your prosthesis can do.
Caused
The causative agent is the bacterium Clostridium perfringens, which invades damaged tissues. The main sources of infection are gunshot wounds, lacerations and injuries resulting from operations.
The pathogenic bacteria can also penetrate into the abdominal cavity, thereby provoking the onset of the disease. In most cases, this happens when eating food contaminated with gas gangrene bacteria or during operations on the colon or appendix.
signs
Pathology develops very quickly. The incubation period can last from a few hours to 2 or 3 days.
- deterioration in general well-being;
- Increased heart rate (tachycardia);
- low blood pressure;
- high fever (over 38 °C);
- change in skin color (yellowing);
- Attacks of acute pain in the wound.
At the first sign of infection, an infectious disease doctor or surgeon should be consulted immediately.

treatment of sarcoma
Cardiac sarcoma is difficult to treat and metastasizes quickly. Often, patients require a heart transplant, which, unfortunately, does not exclude the possibility of a relapse. The doctor may prescribe symptomatic treatment, chemotherapy, and anticancer drugs. Soft tissue sarcomas must first be surgically removed. If regional lymph nodes are visible, they must also be removed, followed by histological examination.
Radiation therapy may be prescribed after surgery to destroy any remaining malignant cells and reduce the risk of recurrence. In this case, chemotherapy is usually prescribed, choosing drugs depending on the type of sarcoma. The following drugs are used in chemotherapy: ifosfamide (Ifex), doxorubicin (Adriamycin), epirubicin, dacarbazine, docetaxel (Taxotere), temozolomide (Temodar), vinorelbine (Navelbine), gemcitabine (Gemzar), eribulin (Halaven).
The most recommended treatment and maintenance of remission is targeted therapy. Targeted therapy allows for more precise treatment aimed directly at the tumor area. Like any other type of cancer, osteosarcoma is best treated with surgery. This may require amputation and excision. Radical methods of excision are possible in advanced stages of the disease, when the tumor disintegrates with strong adhesions, there are pathological bone fractures and bleeding.
If the tumor cannot be surgically removed, radiation therapy can be given. This is most commonly used for Ewing's sarcoma and bone lymphoma. Chemotherapy may be given before surgery to shrink the tumor and determine susceptibility to chemotherapy.
prevention of sarcoma
There aren't many ways to prevent sarcoma, but you can try to control some of the negative influences on your body that can help prevent the disease from developing.
- Take care of yourself and treat infections and inflammatory processes in the body. If you have herpes, consider taking antiviral medications such as aciclovir, famciclovir, or valacyclovir during an exacerbation.
- Try to put yourself less in dangerous situations. If you hurt yourself, try not to hurt yourself again.
- Avoid eating foods that contain carcinogenic substances and chemicals.
- Avoid places with radioactive radiation.
- Avoid exposing your skin to UV rays for a long time. If you plan to be in the sun for a long time, you should protect your skin with a hat and breathable clothing that shields your body from the sun's rays as much as possible. To protect your face and limbs, buy a sunscreen with a high sun protection factor, e.g. B. Avene sunscreen spray SPF 50+, Achromin sunscreen extra protection SPF 50, Librederm Bronzeada sunscreen for face and décolleté spf 50, sunscreen for children spf 60, Achromin sunscreen extra protection for face and body spf 50, Nuxe sun spf 50 or other protective products with high sun protection factor.
- The toe formation.
- The reamputation is.
- Life after a leg amputation.
- Indications for amputation.
- Cubic Bone.
- prosthetic legs.
- prosthetic leg.
- Child has a bump on his foot.
