It has a broad spectrum of activity against bacteria, fungi and unicellular microorganisms and has an antiviral effect 5 . It is used to treat and heal purulent wounds. However, given the potential consumption of the drug (up to 1 liter per day) and the cost of the antiseptic, treatment can be costly.

- Diabetic foot - symptoms and treatment
- Definition of the disease. causes of the disease
- The main 'triggers' for the development of ulcers on the WY are:
- principles of treatment
- Local treatment of ulcers
- necrectomy
- treatment of the wound
- Causes of trophic ulcers of the legs, ankles, feet and toes
- Diabetic Ulcers
- Venous ulcers
- Diagnosis of trophic ulcers
- Causes and risk factors
- Risks associated with the diabetic foot
- For stage 4 wounds.
- prevention
- Why is smoking cessation recommended for diabetic foot ulcers?
- clinical picture
- Treatment
- The main forms of trophic ulcers are.
- Treatment of trophic ulcers
- symptoms
- diagnosis
- classification
- Course
Diabetic foot - symptoms and treatment
What is diabetic foot? In an article by Dr. I. Esipenko, a vascular surgeon with 38 years of experience, will talk about the causes, diagnosis and treatment.
The article by Dr. Esipenko was written by literary editor Margarita Tikhonova and scientific editor Sergei Fedosov.

Definition of the disease. causes of the disease
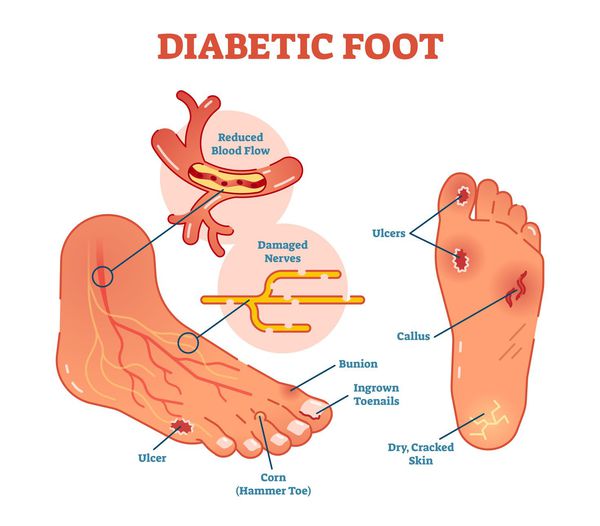
Diabetic foot (Diabetic Foot Syndrome, DFS) is a serious complication of diabetes mellitus in the form of infections, ulcers or destruction of deep tissues resulting from disruption of the macrostructure of the foot and microcirculation as a result of the destruction of nerve endings and nerve fibers. [10]
The main cause of DS is diabetes mellitus (DM). Although diabetic foot syndrome does not develop from day one when blood glucose levels rise above 7.0-8.0 mmol/L, any patient diagnosed with diabetes should be aware of this dangerous potential complication.
Chronic leg ulcers occur in 4-15 % of cases in people with diabetes. In some cases they are the first sign of advanced diabetes [10] .
The main 'triggers' for the development of ulcers on the WY are:
1. Wearing uncomfortable footwear. Any defect in footwear can lead to altered stress on the ankles, compression or abrasion of the skin, local microischemia, infiltration or necrosis:
- Inappropriate shoe size (smaller or larger than necessary);
- high heels and/or high heels;
- scars on the insole;
- defect on the sole;
- wet footwear;
- Shoes that are not appropriate for the season.
2. increased body weight.. Given the surface area of the feet, an increase in body weight (even by 1 kg) increases the stress on each individual ankle. The most vulnerable area is the sole surface.
3. Overgrowth of the epidermis (surface) of the skin. This process is due to disturbed skin metabolism against the background of DM (under the thickened epidermis – the 'callus' in the layers of the skin – microcirculation is impaired, which leads to microischemia and necrosis).
5. Stenoses (narrowing) and occlusions (blockages) of the main arteries. The lack of blood supply to the feet and lower extremities leads to micro- and macro-ischemia and the development of limb gangrene.
principles of treatment
In order for the treatment of trophic ulcers in diabetes to be effective, the following principles must be observed:
- careful preparation of the affected area;
- relief of the lower limbs;
- elimination of bacterial flora;
- compensation of the underlying disease;
- correction of swelling;
- Detection and treatment of concomitant diseases that do not allow a full healing process (anemia, liver pathology, chronic renal failure).
Each of the above steps should be followed as this is considered the 'golden rule' in wound care. If the steps are followed in full, healing of the trophic neuropathic ulceration occurs in 90% of the % cases.
Ischemic trophic defects, in addition to these measures, require revascularization (restoration of blood circulation in the affected limb), since the occlusion of the vascular lumen leads to their formation.

If the wounds are complicated by significant exudate, surgical treatment and detoxification of the patient's body are required.
Local treatment of ulcers
Treatment of trophic leg ulcers in diabetics includes general and local measures. Local treatment is based on the following procedures:
necrectomy
Dead tissue is considered a good breeding ground for bacteria. They also prevent the normal drainage of fluid from the wound surface and the formation of new tissue that allows healing. It is therefore necessary to remove necrotic areas as much as possible.
Stripping can be done with a scalpel and scissors, mechanically with a special machine that emits pulsating jets of water, or chemically with proteolytic enzymes. In another method, the doctor applies wet bandages to encourage the dead tissue to fall off.
Removal of areas of necrosis with a scalpel and scissors is the most common option, but is not used when the wound bed is articulated or when the trophic defect is ischemic. In the surgical treatment, the Volkmann spoon, a spoon-shaped instrument with a small surface, is used. It can be used to gently remove necrotic tissue fragments without destroying blood vessels.

Important: A trophic leg ulcer should be probed with a bullet probe because an optically superficial lesion may have a deep wound channel.
At the same time, the corns that form on the edge of the ulceration are removed. This reduces the pressure on the wound itself and improves drainage of the wound contents. There are cases when it is necessary to remove the nail plate. This is the case when the ulcer is partially on the nail bed or on the fingertip.
treatment of the wound
This step in the treatment of diabetic trophic ulcers is performed to reduce the number of pathogens on the surface of the affected area. There are a number of devices used for flushing, but using a syringe with a needle has proven to be just as effective.
Causes of trophic ulcers of the legs, ankles, feet and toes
Since the causes of ulcers can be very different, let's look at the most common ones.
Diabetic Ulcers
Diabetes (diabetes mellitus) – is a chronic endocrine disease associated with a disturbance in the metabolism of sugar in the body. Such long-term disorders lead to changes in various tissues of our body. Ulcers in the lower extremities are common in diabetes.
In diabetics, small vessels and nerves are damaged and gait is impaired, causing excessive pressure on the foot. This puts more strain on the soft tissue and leads to ulcers.
The inflammation in the affected area can lead to an altered sensation. Diabetes affects tissue nutrition, which slows skin regeneration, and infection can worsen wound progression. In this case, the area of \u200b\u200bthe lesion increases, and the neighboring skin and tissues are involved.
There is also the possibility that ischemic injury (localized interruption of blood flow) that impairs wound healing by reducing the supply of oxygen and all components necessary for healing.
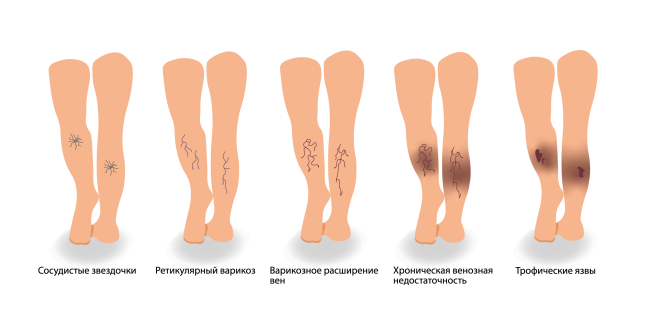
Venous ulcers
chronic venous ulcers arise from the effects of constantly increased venous pressure on the microcirculation of the skin.
Age, obesity, a large ulcer area, and poor adherence to pressure therapy adversely affect ulcer healing.
Diagnosis of trophic ulcers
If an ulcer develops, it is important to see a phlebologist, who will conduct a comprehensive examination, which usually includes the following tests
- general blood test
- blood sugar levels
- Prothrombin time (the time it takes for a blood clot to form)
- Partial thromboplastin time, a test to detect a blood clotting disorder
- Kidney and liver function tests
- Lipid profile (to assess risk of vascular disease)
- Glycated hemoglobin (helps analyze blood sugar levels over time)
- Prealbumin levels (helps assess patient's nutritional status) 5
The sensitivity of the diabetic foot should be checked annually 5 .
In addition, assessment of the arterial blood supply is important.
Causes and risk factors
The development of diabetic foot syndrome is related to permanently elevated blood sugar levels. The disturbed metabolism leads to the formation of ketone bodies and toxic compounds. Over time, blood vessels, capillaries, and arteries become stretched and deformed. Peripheral nerves are damaged. The body's immunity is weakened. Infection can enter open wounds and cause deep inflammation.
- mycosis. Fungal diseases accelerate the spread of ulcers into the deeper layers of the skin.
- Trauma. Due to their low sensitivity, patients do not feel scratches and injuries.
- Impaired blood flow. Low blood flow rate impairs wound healing.
- Neuropathic diseases. Conduction of nerve endings in the feet is reduced, so the patient does not feel any discomfort when wearing tight shoes. Skin damage occurs during this time.
- Ingrown nails. If the pedicure is not done correctly, the sharp edge of the nail will grow into the skin and infect the tissue.
Risk factors for diabetes are increased when there are comorbidities or the following conditions:
- Vascular diseases – varicose veins, thrombosis;
- Deformed feet – flat feet or valgus deformity;
- alcohol or nicotine abuse;
- Wearing tight footwear with uncomfortable shoes. This often makes the diabetic foot worse. Bubbles or water bubbles form. If they are scraped off, a wound remains. Wearing shoes increases the risk of infection and abscesses.
Endocrinologists distinguish between three groups of patients. The first group consists of diabetics, in whom the pulsation of the arteries in the foot is unchanged and sensitivity is preserved. The second group consists of patients who have a foot deformity, no pulsation on the weight-bearing part of the foot, and reduced sensitivity. The third group includes patients with past amputations.
Diabetics with coronary artery disease, vascular atherosclerosis, hyperlipidemia, and peripheral polyneuropathy are at higher risk of developing the syndrome.
Risks associated with the diabetic foot
Diabetic foot in diabetes is dangerous because in the first stage it takes years to develop. The patient does not feel any changes, there are no external symptoms and there is no pain. This is due to the death of nerve endings in the ankle. Gradually, the disease worsens and symptoms worsen in the later stages when medical therapy is ineffective. If the patient delays seeing a doctor, there is a risk that gangrene will develop. This can lead to surgery and even amputation.
The most dangerous is the neuropathic diabetic foot. When complications arise, phlegm quickly develops.
For stage 4 wounds.
- Bandage the wound with saline.
- Remove fallen necrotic tissue that impedes healing (use a sponge bandage);
- Apply an antiseptic dressing to reduce the bacterial load on the wound;
- If there is exudate from the wound, use an absorbent dressing.
If a pungent, unpleasant odor emerges from the wound, this can indicate a serious bacterial infection. In this case, antibiotics are required. But remember: Medicines can only be prescribed by a doctor!
Surgery may be needed: removal of the inflamed tissue to stop the infection from spreading. Bursitis cannot be cured at home. The postoperative wound should be treated with saline.
The use of gels and antiseptic solutions is not advisable!
Another serious complication of diabetes is diabetic osteoarthropathy or 'Charcot foot'.
Mechanism of formation of Charcot's footThe bones become brittle and numerous fractures occur, which the patient does not feel because of his reduced sensitivity. After the fractures, the bones don't heal properly and the foot deforms. Tissue nutrition is compromised, pressure on the foot is redistributed, and ulcers develop at the pressure points.
- The affected foot must be relieved to keep the person from stepping on it, and when walking, the affected foot should be disengaged whenever possible.
- If infection and inflammation develops, antibacterial therapy is required.
- Special orthopedic shoes must be worn.
- Surgery to remove abnormal bone conglomerates.
As soon as you notice the first symptoms of diabetic foot, see a doctor immediately!
If the foot is severely swollen, has developed chestnut brown spots, extensive necrosis, blackened toes or areas of the foot - urgent medical attention is required! Full surgery may be required!
prevention
In outpatient practice, it is important to identify patients who are at high risk of developing a foot ulcer. Patients are advised to have regular check-ups and watch for diabetes and concomitant hypertension and hypercholesterolemia.
Wearing special orthopedic shoes is recommended. If even a minimal ulcer appears, it is important to prevent infection by wearing clean underwear and shoes, treating the affected skin with antiseptics, not overloading the affected limb, and timely consulting a doctor to choose the right treatment.

Why is smoking cessation recommended for diabetic foot ulcers?
Smoking increases the risk of lower limb atherosclerosis, which causes cholesterol buildup on the walls of blood vessels
and their lumens are narrowed. This leads to a deterioration in the blood supply to the tissues.
Dermatovenereologist, Head of DCD Fee Clinic, St. Petersburg City Dermatovenereology Clinic

Trophic ulcers are long-lasting, non-healing wounds that develop as a result of impaired tissue supply. Can such wounds be treated and how?

How to recognize a trophic ulcer on the leg and what causes such a skin defect?

Characteristics and properties of povidone iodine. For what purpose is povidone iodine used? Instructions for use of Betadine ® solution, ointment, suppositories with povidone iodine.
clinical picture
The clinical picture is manifested by 'chills' and/or 'tiredness' in the legs and calf pain. However, pain syndrome with intermittent claudication occurs much later in patients with diabetic foot syndrome than in patients with chronic arterial insufficiency of the lower limbs without diabetes.
On physical examination, the skin is noted to be cool to the touch. Trophic abnormalities in the form of pigment spots, hair loss on the lower extremities, skin thinning, ulcerations of various sizes, nail plate deformities, and the presence of extensive tinea pedis may also be present.

Figure 3: Diabetic foot syndrome, neuroischemic form. Occlusion of the left tibial artery. Necrosis of the second toe of the left foot.
In contrast to the neuropathic form of diabetic foot syndrome, the pain syndrome can be intermittent and of variable severity, up to unbearable pain in the later stages of critical ischemia.
In patients with purulent-arthritic complications of diabetic foot syndrome, destructive changes in the foot develop against a background of 'complete well-being' and no discomfort.
When the main blood supply is interrupted, necrosis of the foot area is formed according to the angiosomal principle, that is, zoning of the blood supply.
Treatment
A multidisciplinary approach is the main strategy for treating abscess-destroying lesions of the foot in patients with diabetes. The following specialists are involved in the treatment of the patient: surgeon, angiosurgeon, radiologist, orthopedist, podiatrist, cardiologist, neurologist, endocrinologist, anesthesiologist, nephrologist, nephrologist.
This number of specialists is due to the variety of target organs affected by diabetes. Conservative therapy of GNO SDS serves to achieve the following goals: control of diabetes, improvement of blood circulation in the soft tissues, reduction of neuropathy, pressure relief of the affected limb, alleviation of acute inflammation and stimulation of local repair processes.
Treatment depends on the objective condition of the patient, the characteristics of the purulent-arthritic complications and the prognosis of the disease. The first prerequisite for treating the necrotic complications of diabetic foot syndrome is the control of diabetes, that is, blood sugar levels; a value of 5 to 9 mmol/l is considered optimal.
High glycemia correlates with increased postoperative complications and slow progression of the wound process. In addition, ketoacidosis, as a manifestation of diabetic decompensation, is a factor that favors the spread of infection.
An important factor determining the treatment tactics is the severity of the infectious lesions. Depending on the severity of the foot infection, they are classified as mild, moderate and severe.
The main forms of trophic ulcers are.
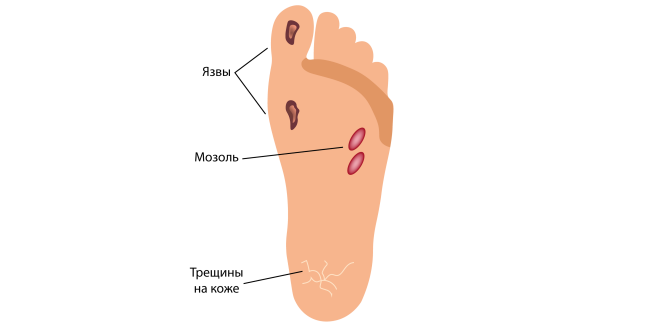
Trophic ulcers (long-term non-healing wounds) are the most common form of diabetic foot ulcers. Going to the doctor and treating the diabetic foot should not be put off, since this syndrome can lead to atrophy of the limbs. It is important to classify diabetic ulcers into neuropathic (in patients with normal blood flow in the legs) and neuro-ischemic (or ischemic) due to impaired blood supply. A small percentage of people with diabetes develop leg ulcers, usually caused by venous disease (venous insufficiency). What types of ulcers are more common? Contrary to popular belief, neuropathic ulcers are more common - they account for about 55-75 % of all diabetic ulcers.
While a severe circulatory disorder alone can lead to destruction (necrosis) of the skin, diabetic neuropathy itself does not destroy the tissues of the foot. However, it creates the conditions for small (and not so small) lesions to go unnoticed by the patient. A diabetic can cut his nails while cutting his nails and not feel pain, he cannot feel a foreign body in his shoes (a stone, a piece of broken glass, a forgotten sock, a coin accidentally fallen into the shoe), he can step on one lying on the floor Kick the paperclip and not feel it. Unfortunately, all of these examples in diabetes are absolutely real. The last type of harm (stepping on a button without the patient noticing) happened to the author of these lines in his practice no more than three times. Of course, all these injuries lead to the development of trophic ulcers.
Treatment of trophic ulcers
- Appropriate topical treatment. A new wound dressing can be applied daily or every 2 to 4 days (depending on the condition of the wound and the type of treatment).
a). Use of modern dressing materials (which, unlike gauze, do not stick to the wound). There are now a large number of such materials, belonging to different classes - alginates, hydrophilic fibers, atraumatic meshes, polyurethane foam dressings, hydrogels, hydrocolloids, etc. The choice of dressing is made by a medical professional (doctor or specialized nurse) based on a wound examination, hit by x-ray data etc.
b). Irrigate the wound with antimicrobial agents that will not damage the growing tissue - e.g. B. Miramistin solution, chlorhexidine, etc. Remember that iodine, alcohol, green and manganese-containing solutions are contraindicated in diabetes, as they slow down the healing process.
c). Regular wound care by a doctor or nurse (removal of non-viable tissue, blistering around the wound (often caused by neuropathic ulceration)). Usually performed every 3-15 days. - Protection of the ulcer from stress when walking. As long as the patient keeps stepping on the wound, the wound will not heal, no matter how expensive drugs or dressings are. Unfortunately, just a few steps a day can negate the effects of the ongoing treatment. Most neuropathic ulcers are painless, so the patient does not feel that they stepped on and damaged the wound. There are special relief devices to protect the wound. The 'low shoe', which does not put any strain on the forefoot when walking, was used for the first time in Russia. Today, however, according to international and Russian recommendations, the most effective offloading method is the offloading shoe (Contact Cast, see image on the right) made of polymeric fixation materials (which are now used instead of plaster). This method allows the wound to heal faster, relieves not only the forefoot but also the hindfoot and enables active living and working (in contrast to a 'low shoe').
- Competent use of antibiotics for wound infections (usually the choice of drug is based on the results of wound culture). Approximately 40-60 % outpatients with diabetic ulcers require antibiotics.
- Normalization of blood sugar levels (diabetes control). It is important that a patient with diabetic foot ulcers receives ongoing, quality diabetes care.
symptoms
Ulcerative abscesses do not occur randomly. There may be swelling accompanied by itching and crusting. The skin becomes thin and has a bluish tint. Pigmentation may occur in this area.
- chills and cramps in lower limbs at night;
- small droplets of liquid form on the skin if there is a blockage in the lymph;
- When the epidermis peels off, an ulcer forms with thickened edges;
- When touching the ulcerated area, there is severe pain;
- When bacteria settle in a bleeding ulcer, pus appears.
These symptoms appear gradually, leading to an exacerbation of the disease.
The lower limbs are the most common place for the manifestation of ulcers. The reason for this is the slowing down of blood flow in the blood vessels. If the tissue is not supplied with sufficient nutrients, lymphatic phenomena and a purulent coating form on the ulcer.
This type of disease is called trophic ulceration. If the patient has diabetes, ulcerative phenomena are formed on the heels and feet.
In most cases, the disease is caused by varicose veins. When skin damage occurs, even if it's not too severe, it leads to ulcers.
If ulcers appear on the lower leg, it means that there are major changes in the venous vessels. The area is enlarged and blood flow is compromised. At the same time, the patient suffers from severe pain.
If the extent of the ulcer is large, this indicates poor blood circulation. In this case, such a process is already protracted and exacerbations occur. If the ulcers are large, you should not try to treat them yourself, but quickly consult a doctor.
In the initial stages, when the ulcer bleeds, there may be an infection caused by the spread of bacteria or fungi. Pus forms and there is an unpleasant odor. If the process lasts longer, then the pus penetrates into the deeper layers, they become severely inflamed, and severe pain appears. It spreads to the games and the hock. If the case is neglected, an aggravated form of sepsis will develop.
diagnosis
When trophic leg ulcers appear, a specialist doctor is consulted who makes a diagnosis. Examination can accurately determine the extent of infection and the extent to which deep or superficial tissue is affected. Therefore, diagnostic measures are required before treatment can be prescribed.
- blood glucose test. Accurate determination of sugar levels is necessary, which is especially important if the patient has diabetes.
- Wasserman test. This is an analysis to detect antibodies to perform a serological test.
- Cytological examination. In this case, the presence of tumors is examined. The analysis is a check of the condition of the cells, their damage
- Bacteriological examination. It is important to determine the degree of infection.
If an ulcer is present, the doctor will review the test results. If necessary, he will prescribe an ultrasound examination of the vessels of the lower limbs and an X-ray examination using a contrast agent (angiography). Spiral CP, IT, and revascularization may also be prescribed. All these measures are necessary to accurately determine the extent of the disease.
Often the diagnosis is made by more than one specialist. He or she may be referred to a phlebologist. Such a specialist specializes in determining the nature and extent of the vascular disease of the legs. The doctor will conduct a consultation and may also recommend some examinations if necessary.
classification
Neuropathic form – disturbance of the sensitivity of the feet in the form of stockings or socks, dry skin and possible small cracks. Nerve damage is a common complication of diabetes - feeling in the feet is impaired to the point of total loss, and damage to motor nerves leads to muscle wasting. In the neuropathic form, some patients do not experience trauma, fever, skin eruptions, and sustain injuries that can lead to infection.
Osteopathic form - destruction of bones and joints leading to foot deformities, trophic ulcers and skin damage. Poor circulation weakens the bones and can lead to the breakdown of the bones and joints in the foot and ankle. A weakening of the ligaments leads to multiple dislocations of the foot bones and deformations. Bone fractures and pathological fractures are not accompanied by pain symptoms and can occur unnoticed by the patient until the skin is pierced by a bone fragment. In such cases, purulent complications and wet gangrene develop unnoticed.
Ischemia is a disruption in the blood supply to the foot with the formation of trophic ulcers and dry gangrene. It is caused by a blockage in blood flow due to arterial blockage caused by atherosclerotic plaque. Against the background of ischemia, there is dry necrosis of the fingers or toes, which easily develops into wet gangrene. The most dangerous thing about diabetes is that, given the reduced sensitivity, the patient can overlook the appearance of trophic ulcers and necrosis, solidifying his disease into diabetic phlegmon.
Diabetic phlegmon and gangrene is a severe, purulent destruction of the soft tissue and bones of the foot with impaired blood circulation. A phlegmon can also develop with preserved vascular patency, a gangrene only with blockage of the lower leg arteries. The causes of phlegmon and gangrene are different, but the result is usually the same: amputation. Only timely specialized surgical treatment can ensure the preservation of the limb. The frequent occurrence of purulent and putrefactive infections is due to the immune disorder characteristic of diabetics. The neuropathic form reduces alertness to trauma, and the infection easily penetrates the subcutaneous tissues, which leads to the development of diabetic phlegmon. Phlegmon is a purulent dissolution of the soft tissues. It can be caused by a variety of microorganisms, with the causative agents of gas gangrene being the most dangerous. Infection in diabetes quickly leads to poisoning and sepsis. When sepsis develops, the general condition of the patient deteriorates dramatically, the functioning of the liver and kidneys is impaired, and severe pneumonia often develops. If sepsis is not diagnosed and treated early, the prognosis is extremely poor.
Course
Once a diabetic foot has developed, diet and sugar control, proper foot care, regular foot exams, and timely doctor visits are crucial. In this case, complications rarely arise. In European countries with a well-developed podiatry, the development of diabetic gangrene is very rare. The number of diabetic amputations has decreased tenfold in Europe, but in Russia diabetic gangrene is the main cause of high amputation rates.
The most dangerous and extreme stage of diabetic foot syndrome is the development of gangrene on the foot. The diabetic foot is the leading cause of non-traumatic peacetime amputations. In Russia there are up to 70 000 amputations annually due to diabetic gangrene.
Diabetic gangrene with accompanying anaerobic infection is not uncommon. It leads to necrosis of damaged tissue and infection of blood and healthy tissue. The disease progresses very quickly and often leads to death.
Trophic ulcers are another complication, most commonly found on the sole or big toe. They can also form on the sides of the foot from ill-fitting footwear. If left untreated, they can lead to serious infections. The classification of diabetic complications also includes trophic lesions of the skin of the feet.
Read more:- Photo: Diabetic heels.
- Why amputate legs for diabetes?.
- X-ray of Charcot's foot.
- Indications for amputation.
- Metatarsal amputation.
- foot in Latin.
- The reamputation is.
- Insoles for diabetics.
