Avoid excessive consumption of sweets, alcohol and caffeinated drinks.

- Recovering from a fracture of the 5th metatarsal
- Causes of a fracture
- Treatment of metatarsal fractures
- Complications of metatarsal fractures
- diagnostic methods
- Symptoms and stages
- Acute
- Subacute
- Chronic
- surgical treatment
- Causes and symptoms of a fracture
- Symptoms of a metatarsal fracture
- Principles of Diagnosis
- Treatment
- symptoms of the disease
- Causes of a marsupial bone fracture
- Which doctor should I see?
- Fractures of the anterior row of the hyoid bone.
- Fractures of the metatarsal bone
- Rehabilitation after a foot fracture
- massage
- physical therapy
- PHYSICAL THERAPY
- Stages of rehabilitation
- symptoms of the disease
- Causes of nonunions and healed fractures
- Which doctor should I see?
- The diagnosis
- Treatment of marching foot
Recovering from a fracture of the 5th metatarsal
Rehabilitation after a metatarsal fracture avoids foot deformity, arthritis and pain.
A fracture of the metatarsal bone is rare. To accurately diagnose it, a thorough examination must be carried out.
Because of the similar symptoms, a metatarsal fracture is often confused with a sprain or bruise.
Treatment and rehabilitation after a metatarsal fracture heals is a serious matter. All medical advice must be followed to avoid further foot deformity, arthritis and pain.
Causes of a fracture
A metatarsal fracture usually occurs as a result of trauma, an overload of the joints (when the foot is subjected to constant stress).
- sudden, abrupt pressure on the foot when jumping;
- falls;
- certain sports (strength sports, extreme sports);
- footwear (tight, uncomfortable, uncomfortable);
- striking the foot with a heavy object;
- accidents (at work, in traffic);
- constant exertion, lifting heavy objects and work activity.
However, with timely treatment and good rehabilitation after a fracture of the 5th metatarsal bone, this injury can be controlled.
Treatment of metatarsal fractures
Neck fractures without class A dislocation requires the use of ice, pain medication, elevation of the limb, and 24-hour observation as severe swelling may occur. A short plaster cast should then be applied for 4-6 weeks. For displaced neck fractures, ice, limb elevation, pain medication, and urgent referral to an orthopedist for repositioning are indicated. Non-displaced diaphyseal fractures of metatarsals II-V can be treated with elevation, ice packs, pain medication, and a thick compression bandage in the first 24 hours. Afterwards, wearing a Thomas metatarsal pad under the forefoot and using crutches is recommended.
Full resilience full resilience Full weight bearing is indicated depending on tolerance. For diaphase I fractures of the metatarsal bone without displacement, a short cast must be placed on the tibia with weight bearing on the limb for 2 to 3 weeks; A short plaster shoe is then applied for another 2 weeks. Diaphyseal fractures of metatarsals II-V with displacement require repositioning. If referral to an orthopedist is not possible, the toe is treated with a distraction splint under local anesthesia. The distal portion of the tibia is contoured with weights. After repositioning, a soleless cast is applied from the tips of the toes to the top of the foot. At this point, traction is interrupted and the cast is continued to the tibial tubercle. X-rays after reduction are highly recommended. After 4 weeks, the plaster cast should be replaced with a plaster shoe for another 3-4 weeks. Fractures of the first metatarsal bone with displacement require referral to an orthopedist for reduction. If this is not possible, closed reduction should be performed using the above technique. If this is successful, a plaster cast should be applied for 6 weeks. Fractures that do not respond to closed reduction may require open reduction.

Complications of metatarsal fractures
Fractures of the neck and diaphyses of the metatarsal bone with transverse fracture Fractures of the neck or diaphyses of the metatarsal bone with transverse or angular displacement often lead to keratosis of the sole. An early referral to an orthopedist is therefore advisable. Transverse fractures of the proximal part of the V bone or diaphyseal fractures of the other metatarsals are often difficult to heal and therefore require referral to a specialist.
Publisher: Iskander Milewski. Release update date: 3/18/2021
The information contained on this website requires consultation with your doctor and is not a substitute for a direct discussion with your doctor.
Please refer to the User Agreement for further details.
diagnostic methods
A marching foot fracture is diagnosed like other fractures. The difference is that the patient's condition allows him to go to the emergency room independently. The attending physician then asks the patient about his or her job, recent changes in physical activity, and the presence of chronic illnesses. An x-ray and general examination are then performed to assess the current condition of the body. The fissures can be seen in different stages of development on the x-ray.
If damage to structures such as blood vessels, tendons or nerve endings is found, an additional examination of the foot using computer tomography (CT) or magnetic resonance imaging (MRI) is recommended. Based on the complete examination, doctors make a diagnosis and decide on treatment.
Symptoms and stages
A fracture of the metatarsal bone is accompanied by the following symptoms. It is not uncommon for the injury to manifest itself in different ways, but the general symptoms are as follows:
- The first symptom is the development of pain syndrome during physical activity, which subsides after rest but does not disappear.
- The condition persists and a stabbing pain occurs in the foot with every movement, which can spread to the lower leg.
- As soon as a microfracture occurs, the soft tissues react with swelling, less often with a hematoma.
Acute
At this stage, the first changes in the bone tissue - microfractures - are visible. This is due to the thinning of the tissue as a result of regular stress. The body responds to the injury by using resources to rebuild. The acute stage is therefore characterized by a strengthening of the metatarsal bone, its stiffening.
Subacute
The compacted bone continues to be subjected to regular traumatic loads, so the resulting microcracks do not have time to heal and begin to merge into a single crack. At this stage, moderate pain occurs that increases when walking, running, or exercising.
Chronic
A syndrome of microcracks, combined with the depletion of the body's resources due to regular, strenuous physical activity, leads to the development of a fracture. Due to its structure, the tarsal bone often breaks in the shape of a 'green branch'. This means that the elastic, resilient periosteum remains intact, but the internal bone structures break. This condition is referred to as 'marching foot'.
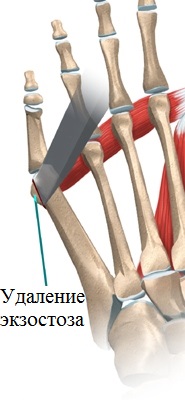
surgical treatment
If conservative treatment fails and x-rays show that the heads of the fourth and fifth metatarsals are separated, surgery is indicated. Surgery can restore the normal relationship between the bones of the foot.
For small deformities, the operation can be limited to a simple resection of the exostosis (nodule) of the head of the fifth metatarsal bone. This is a quick and uncomplicated procedure that can be performed on an outpatient basis.
If the angle between the fourth and fifth metatarsals is too large on the X-rays and conservative treatment is usually no longer effective, surgery is the only way to help the patient.
If the deformity is advanced, an osteotomy (cutting the bone) of the fifth metatarsal bone is performed, the bone fragments are brought into the correct position and then fixed with special screws.
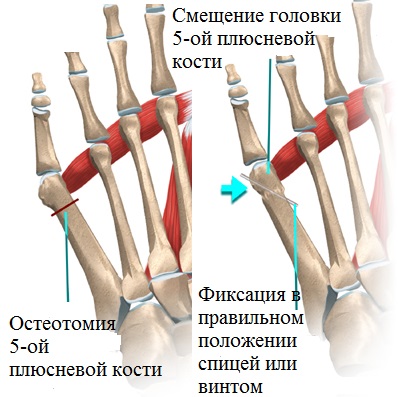
The metal screws remain in the bone until it has completely healed. In this way, misalignments in various parts of the foot can be corrected and the patient is relieved of pain while walking.
After surgery, patients usually wear special shoes for a while to relieve pressure on the forefoot. The stitches are usually removed 12-14 days after surgery.
In our clinic we extensively use minimally invasive methods to treat foot pathologies. The operations are carried out using the most modern medical equipment and high-quality and proven consumables, fixators and implants from the world's largest manufacturers.
However, the result of the operation depends not only on the equipment and quality of the implants, but also on the skills and experience of the surgeon. The specialists at our clinic have many years of experience in the treatment of foot pathologies.
Causes and symptoms of a fracture
A metatarsal fracture can be caused by primary trauma due to direct impact or secondary trauma due to osteoporosis or excessive exercise (pathological metatarsal fractures). This pathology includes a wide range of injuries, from isolated fractures of a single metatarsal bone without displacement to complex comminuted fractures of the metatarsal bone with damage to the soft tissues of the foot.
These fractures are usually divided into two main groups:
This type of fracture can occur in a single bone or in multiple bones at the same time. Stress fractures of the metatarsal bones are common in athletes, particularly runners, ballet dancers, and gymnasts.
- Fractures with and without fragment displacement.
- Open and closed fractures.
- Transverse fracture of the fifth metatarsal (Jones fracture).
- Fractures of the metatarsal neck.
- Fractures of the metatarsal base (with and without Lisfranc fractures).
- Transverse, burst, fragment, oblique and spiral fractures.
- Intra- and extra-articular fractures.
The 2-4 metatarsals are most commonly injured.
Symptoms of a metatarsal fracture
The severity of symptoms varies depending on how severe the injury was. Often there are no visible signs of a fracture, and a person mistakes a fracture for a simple bruise. However, there are some indirect signs that indicate a closed fracture:
- Pain in foot after exercise.
- Spontaneous swelling of the metatarsal region.
- Reducing pain at rest.
- Occurrence of abnormal grinding and stabbing pain.
- Abnormal position of the toes.
- Swelling with hematoma and pain.
- An open fracture is characterized by more pronounced symptoms:
- The occurrence of bleeding.
- Tearing of the soft tissues.
- Expansion of the bone through the torn wound.
- Significant pain.
Principles of Diagnosis
All patients are first visually examined by a specialist. The doctor assesses the extent of the damage and orders additional diagnostic procedures. These include MRI, CT or X-rays. After the examination is completed, a preliminary diagnosis is made. A normal x-ray (anteroposterior, lateral and oblique) is usually sufficient to diagnose a fracture. CT or MRI scans are used to rule out other injuries and, if necessary, to determine the type of fracture more precisely. In some cases, comparison with the opposite lower extremity may also be necessary.
Treatment
A metatarsal fracture requires special treatment. The treatment method is selected and adapted individually by the doctor. Conservative treatment is only used if the fracture is not dislocated. Treatment procedures generally depend on the type and complexity of the injury and include.
- Symptomatic treatment Taking painkillers and antipyretics and wearing a soft protective bandage.
- Repositioning of the fracture under anesthesia
- Applying a short plaster cast to the injured limb.
- Therapeutic measures Wear immobilization shoes.
- Physiotherapeutic treatment
symptoms of the disease
A metatarsal fracture may initially be difficult to detect, even on an X-ray. The difficulty is that it is a 'green branch': the internal bone tissue is damaged first, while the surface remains intact. It takes 4-5 weeks for the injury to become clearly visible. The presence of an injury can be recognized by the accompanying symptoms, which include stabbing pain when palpating the foot. Other symptoms include:
The symptoms of an injury may not be very pronounced, especially in the early stages. However, without treatment, the signs of a fracture become increasingly obvious. However, it is important to seek help at the right time, when therapy is most effective and does not last long. Therefore, a diagnosis should be made at the first suspicion of a metatarsal fracture in order to avoid serious consequences. This includes:
Such complications lead to increased stress on other parts of the musculoskeletal system, especially the spine. This situation leads to rapid wear and tear, resulting in pathologies of varying degrees of severity. Diseases caused by trauma to the metatarsal require longer and more complex treatment, which is not always successful.
Causes of a marsupial bone fracture
This injury occurs as a result of excessive stress on the forefoot. In this case, the arch of the foot is disturbed and the metatarsal bone is damaged. Risk groups include military personnel, athletes and people with an active lifestyle. In most cases, a stress fracture of the marching foot is caused by the following factors.
- unfamiliar footwear;
- Excessive use of the feet;
- Prolonged standing on feet;
- Carrying heavy loads;
- the presence of flat feet.
Injuries are not uncommon among physically fit people. This is the case, for example, with athletes, both men and women, who train intensively for competitions. The disease can be triggered by a professional activity that requires the affected person to stand for long periods of time: hairdressers, salespeople, lecturers. These people need to rest their legs and, if possible, sit down between jobs. Newly hired employees are at risk. In them, a fatigue march fracture may be due to the type of military service:
In 5 % of the recruits, a combination of these causes leads to a march fracture. In more cases, namely in 50 %, the second metatarsal bone is injured. The third and fourth metatarsals each account for 25 %.
Which doctor should I see?
A broken foot is difficult to detect in the early stages, but its consequences lead to more serious injuries. Despite the mild symptoms, diagnosis is important even if pathology is suspected. The diagnosis and treatment of the disease are controlled:
Fractures of the anterior row of the hyoid bone.
Fractures of the scaphoid, cuboid and sphenoid bones usually occur as a result of direct trauma - a fall on the foot with a load. Fractures of the navicular bone can also be caused by indirect trauma - with excessive flexion of the foot, the foot is compressed and breaks in the horizontal plane, displacing the bone fragment forward. A sudden contraction of the tibialis posterior muscle results in a rupture of its tuberosity at the tendon insertion site. As a rule, fractures of these bones do not cause significant displacement, but they do cause weakness in the longitudinal arch of the foot.
symptoms. Examination reveals swelling of the foot and subcutaneous hemorrhage at the site of impact. Local pain on palpation. A subluxated fragment of the meniscus bone may be palpable. The pain increases with movement of the distal part of the foot (when the fifth foot is standing) or with axial loading of the metatarsal bone. The location of the fracture is clarified radiographically in two or three projections (if the tubercle is detached). Sometimes a separation of the sesamoid bone in this area of the foot is seen as a tuberosity fracture. Therefore, a comparative radiograph of the other foot should be taken to differentiate the two cases. There are cases when a fracture of the ischium is not found, so sometimes it is necessary to repeat the x-ray in a different projection.
Treatment. If there is no displacement of the bone fragments of the splint, a plaster cast with a well-modeled longitudinal arch of the foot is applied for 3 weeks. This is followed by physiotherapy and balneotherapy treatment. The duration of the inability to work is 4-5 weeks. Supinator shoes must be worn for one year.
In case of. Subluxation and dislocation fractures of the navicular bone over the head of the carpal bone is reduced under local anesthesia. Axial traction and flexion of the distal part of the foot is performed, and the protruding fragment is compressed and reduced with two toes. After repositioning, the foot is brought into the central physiological position. However, since the subluxation has a tendency to recur, it is preferable to fix the fracture immediately after reduction with two or one K-wire through the skin at the carpal head and to apply a plaster shoe. The pins are removed after 3-4 weeks and the plaster cast after 2.5-3 months. The patient then undergoes reconstructive treatment. Again, you can return to work 3-4 months after the injury.
Fractures of the metatarsal bone
Metatarsal bones most often break when the body is exposed to direct trauma - pressure or impact with a heavy object. Fractures of one or more bones can occur at the same time. Fractures most often occur in the area of the diaphyses and neck of the metatarsal bone, less often in the base and head of the metatarsal bone. Fractures of the cusp of the fifth metatarsal can also separate. When one or two bones break, there is no significant displacement of the fragments because they are supported by the neighboring intact bones. It is very disadvantageous if the fractures are at an angle, towards the sole or to the opposite side, as normal footwear puts pressure on the representation of the malformed bone and causes pain. This is particularly common with fractures of the metatarsal neck.
symptoms and diagnosis. The diagnosis of a metatarsal fracture is made based on the medical history and clinical symptoms, which in turn depend on the severity of the injury and the number of bones broken. The foot is swollen, there is bleeding on the surface, and sometimes the skin is damaged. Extension of the foot is impossible due to pain. On palpation, acute local pain occurs, which increases with axial compression of the bone. The type and location of the fracture is clarified radiographically in two projections.
Treatment. For fractures with little or no displacement of the fracture width, a plaster cast is applied under local anesthesia, which well simulates both the longitudinal and transverse arches of the foot. A radiological follow-up check is carried out.
After 5-6 weeks, the cast is removed, restorative treatment is recommended, and the foot is supported with supinator shoes. Duration of incapacity for work
2-3 months, depending on the number of fractures.
fractures the diaphysis and neck of the metatarsal bone Displaced fractures are repaired under local anesthesia. Traction along the bone axis and lateral correction with the hand is effective in most cases. The 1st and 5th metatarsals must be reduced with particular care. However, a plaster shoe does not provide a secure hold for the reduced fragments, especially in the case of oblique fractures of the diaphysis and the necks of the metatarsal bones. Therefore, they are fixed with Kirschner nails (one in each bone), which are passed from the sole or interdigital side through the skin and head to the diaphyseal bone. A plaster cast is applied and the procedure is the same as for fractures without displacement.
Rehabilitation after a foot fracture
A plaster cast or immobilizing bandage is applied for 3-4 weeks to several months for complex injuries. Rehabilitation begins after immobilization and lasts up to a year.
Removal of the cast should be prepared in advance. After 2-3 weeks after an uncomplicated injury, it is advisable to remove the splint and move the ankle without putting any strain on the limb. Exercises to improve blood circulation that do not affect the injured leg but improve its blood supply are also recommended.
After the bandage is removed, rehabilitation takes place.
- Massage;
- Physical therapy;
- PHYSICAL THERAPY;
- diet that begins during treatment;
- Wearing special shoes, insoles and cushions for the feet.
A holistic approach to recovery allows you to regain full mobility more quickly.
massage
Before removing the bandages on the free part of the limb, massages are performed. Once the leg is free, the basic techniques should be learned by the nursing staff and the foot massage should be performed alone or with the help of a loved one. A professional massage performed by a professional is best.
The massage improves blood and lymph circulation, tones blood vessels and muscles, and helps reduce swelling.
physical therapy
Physical treatments can be started during immobilization and continued after the cast is removed. The following treatments are indicated:
Hardware treatments improve microcirculation, promote the resorption of edema and hematomas, and accelerate the formation of bone callus.
For example, after a double ankle fracture with foot subluxation, rehabilitation includes:
The doctor determines the order of treatments. Due to the long immobilization after such a fracture, it takes a long time for the foot to recover.
PHYSICAL THERAPY
Depending on the location and type of injury, a set of physiotherapeutic exercises is selected individually for each case. Standardized exercises help restore muscle memory, improve tissue trophics, and prepare the foot for full participation in movement with simple activities.
Stages of rehabilitation
During the cast, hip and knee joint exercises should be performed to maintain muscle tone and improve blood circulation.
Rehabilitation must be carried out consistently so as not to put excessive weight on the limbs. The main stages of correct rehabilitation:
- First phase.. Rehabilitation should begin with warming up the foot with massage. Simple kneading movements without any effort are suitable for this. The movements are light, kneading and stroking. Do not attempt to walk immediately, especially without crutches. This mistake is often made during the rehabilitation of patients with metatarsal fractures.
- Second phase.. In the second phase, a specially selected set of physical exercises should be performed, periodically increasing the load. Walking is of utmost importance. It is important to walk properly from the start without limping, which can lead to mental paralysis. The arch of the foot, whose muscles have atrophied due to immobility, should be trained.
- Third stage.. In the final phase, exercise should not be stopped, the diet should be continued and physiotherapy should be attended. In this phase, exercises to develop the spring function - small jumps - are carried out.
The rehabilitation period should result in full joint mobility and a steady gait without limping. Shoe insoles should continue to be worn to make movement easier. This is a mandatory part of rehabilitation for patients with all local injuries, except for a fracture of the fifth metatarsal, which is the most common.
symptoms of the disease
The formation of a false joint takes a lot of time. They attribute the discomfort and pain that patients feel at the fracture site during this period to the healing process of the bone or to various external factors (up to the body's reaction to weather changes). Therefore, they are not even aware that they are suffering from nonunion and healed fractures. However, even one characteristic feature can indicate a pathology - increased mobility of the limbs, which is anatomically impossible. In later stages, other symptoms appear:
- the ability to twist unnaturally;
- increasing the range of motion of the joints;
- shortening of the limbs;
- decrease in muscle strength;
- Impairment of motor function of the injured limb;
- pain during physical activity.
Dropping of the foot and the use of crutches may occur when walking. Real joints can become dysfunctional due to reduced pressure on the real joints. In the area of the false joint there is often significant swelling due to active connective tissue growth.
Causes of nonunions and healed fractures
A false joint is a complication of an unhealed bone fracture. It arises directly from the abnormal fusion of the remaining bone, which can be caused by the following factors, among others
- soft tissue surrounding the bone fragments;
- wide spread of broken bone elements;
- insufficient immobilization of the injured limb;
- problems with the blood supply to the bone;
- Hardening at the fracture site.
There is a high risk of pathology in multiple fractures, wound infections and improper application of a plaster cast to the injured limb. Those affected are particularly vulnerable:
The space between the individual bone fragments gradually fills with connective tissue. Their edges fuse with the cartilage, which increases the mobility of the injured limb. At the same time, a pseudojoint cavity forms in the gap. It is filled with liquid and enveloped.
Which doctor should I see?
If an unnatural dislocation occurs at the fracture site and overall mobility of the limb is impaired, the injured bone may not have had time to heal. If this is the case, you should consult a doctor immediately. False joints and unhealed fractures are treated:
The diagnosis
The diagnosis is made on the basis of an examination, examination and x-ray data. The image that is created during the radiological examination is crucial. In Deichlener's disease, a change in the structural pattern is noted in the diaphysis of the affected metatarsal bone (sometimes closer to the head, sometimes closer to the base, depending on the location of the most functionally overloaded area). An oblique or transverse luminous band (Looser's lucency zone), an area of bone remodeling, is noted. This looks like the metatarsal bone is divided into two fragments. However, in contrast to the radiological picture of a fracture, in this case there is no displacement.
Next, periosteal growths appear around the damaged bone. At first they are thin and sinewy, then they become dense and resemble spindle-shaped bone marrow. Later the luminal zone disappears and sclerosis occurs. Over time, the periosteal layers dissolve. The bone is permanently thickened and compacted. It is characterized by the absence of acute trauma, the typical location of the injury and the presence of a realignment zone in which there is no displacement of the fragments and the bone maintains its regular shape. It is important to note that no radiological signs may appear in the first few days or weeks. Therefore, when characteristic symptoms are present, it is sometimes necessary to take several x-rays at a certain distance.
Treatment of marching foot
The treatment is carried out by trauma surgeons. Treatment is strictly conservative; surgical intervention is contraindicated. In acute cases, a plaster splint is applied and bed rest is recommended for 7-10 days. After the acute symptoms of the disease have subsided, as well as in the primarily chronic form of the disease, massages and heat treatments (paraffin packs, baths) as well as other physiotherapeutic treatments are recommended. Patients are then advised to wear orthoses and avoid long walking.
The prognosis is favorable: if the stress is eliminated and appropriate conservative treatment, all symptoms subside within 3-4 months. Prevention consists of choosing comfortable footwear, reasonable physical activity and careful medical monitoring of soldiers.
2. Anthology on stress fractures / AV Yankin, GA Krasnojarov, PS Markevich // Bulletin of the All-Russian Scientific Center of the Russian Academy of Medical Sciences - 2012 - №2
3 Clinical and radiological manifestations of stress pareolomas (stress fractures) / Zholdybay JJ, Tuleutaeva ZK, Akhmetbaeva AB, Nurumbetov KM, Dalieva GA, Kassymbekova GD // KazNMU bulletin – 2014 – №2
Read more:- metatarsal bones.
- The tarsal and metatarsal bones.
- metatarsal and metacarpal bones.
- tibia and fibula.
- Fracture of the 5th metatarsal.
- metatarsal bones.
- bones of the foot.
- tarsal bones of the foot.
