What happens if you get a bruise? What are the symptoms and consequences of a bruise? What is the most effective treatment for bruises?

- Post traumatic arthritis
- Causes of post-traumatic arthritis
- Pathogenesis – mechanism of disease development
- What types of hematomas are there?
- causes and symptoms
- Foot bruise
- How can this swelling be relieved?
- How do you tell the difference between a bruise and a fracture?
- First aid
- Clinical manifestations of posttraumatic syndrome
- Stage I
- Stage II
- Stage III
- Diagnosis of post-traumatic syndrome
- Severity of toe bruises
- Emergency treatment for a bruised toe
- When to seek medical attention for a lower limb bruise
- Causes of a leg bruise
- Open fracture
- How do I tell the difference between a bruised foot and a fracture?
- Bruises: symptoms and consequences. What are the risks of a bruise?
- Treating a bruise
- First aid measures for a bruise
- Treatment of bruises in the acute phase
- Treatment of bruising: Reconstructive therapy for bruising
Post traumatic arthritis
Joint injuries are very common. Knees and ankles in particular can be affected. Today we know that post-traumatic arthritis almost always occurs, even with minor joint injuries. Whether the inflammatory process is chronic or acute depends on the severity of the injury, the nature of the body and timely medical care. That's why it's worth visiting a clinic even after a minor injury.
Post-traumatic arthritis is inflammation of the joint immediately or some time after the injury. The inflammation always develops after the injury. In some cases it develops imperceptibly and disappears without consequences, but more often it manifests itself months or even years later with pain and joint dysfunction.
It is more common in young men. ICD-10 code M13.8 – other specified arthritis.
Causes of post-traumatic arthritis
In the development of post-traumatic arthritis, trauma is the main cause. Acute injuries such as bruises, sprains or fractures are always noticed by the victim and can be attributed to subsequent inflammation in the joint. In most cases, this is a reason to see a doctor.
Injuries can also be chronic in nature. This is the case if you constantly lift weights, are overweight and lead a sedentary lifestyle. Sometimes an acute injury seems minor to the injured person, and the appearance of arthritis symptoms cannot be attributed to the injury. These are the most dangerous injuries because the patient almost never seeks medical attention in a timely manner, thereby wasting time and making the condition chronic and destructive.
Athletes, people who perform heavy physical labor (miners, sailors), overweight people and people with a sedentary lifestyle are at risk of developing traumatic arthritis. People suffering from chronic inflammatory diseases of the musculoskeletal system are also at risk: rheumatoid arthritis, gout, etc.
Pathogenesis – mechanism of disease development
In recent years it has been shown that even a small injury triggers the development of an inflammatory process. This takes place at the cellular level. The cells of the intra-articular tissue produce pro-inflammatory (pro-inflammatory) biologically active substances - prostaglandins, cytokines, etc. An inflammatory process that begins with an acute, minor injury (minor bruise) can lead to complete recovery after some time.
However, in the presence of risk factors such as reduced immunity, various chronic diseases and obesity, the inflammation lasts longer and gradually leads to degenerative and dystrophic changes in the joint and impairment of its function.
In severe injuries, in addition to the mechanism described above, a process of necrosis (death) of cartilage cells (chondrocytes) is activated directly by the mechanical impact. The chondrocytes surrounding the area of necrosis have a mechanism of autolysis (self-destruction). The cartilage tissue is destroyed, and this process is promoted by persistent inflammation. In place of the destroyed cartilage, connective tissue (pannus) forms, which limits the mobility of the joint. The subchondral bone tissue begins to grow, which leads to deformation of the joint. Over time, the hip socket is replaced by bone tissue and ankylosis occurs - complete immobilization of the joint.
What types of hematomas are there?
The sooner a hematoma forms after a serious bruise, the more difficult the recovery will be. These injuries can be divided into several categories:
- Lightweight. Develops within 24 hours. The sensation of pain is low.
- Moderate severity. Develops within five to six hours and is accompanied by swelling and pain. If a hematoma forms in the leg or arm after a bruise, the function of the limb may be slightly impaired.
- A severe bruise can occur within a few hours and can be accompanied by significant dysfunction of the leg or arm, swelling, and pain.
- Mild forms of hematomas are the most common. These are usually bruises.
Bruises can also be classified according to other criteria. For example:
- According to the depth of the spot. In this case, the injury can affect subcutaneous tissue (subcutaneous hematoma), mucous membranes, muscle tissue (intermuscular), fascia (subfascial).
- Blood status is also monitored. The hematoma may be fresh (no clotting blood), clotted blood, or lysed (old blood that cannot clot). Lysed lesions are detected after 14-20 days, clotted lesions after a few or three days.
- This depends on the spread of the blood. A hematoma can be diffuse (when the blood penetrates all tissues, it spreads quite quickly), cavernous (accumulation of blood between body cavities), draining (the cavity fills with blood and a connective tissue 'sack' forms around it ).
- Bleeding can be both pulsatile (blood flows freely from the vessels) and non-pulsatile (the ruptured vessel is blocked by a blood clot). They can also be arterial, venous or mixed.
The location of the tear also depends on where the injury occurred.
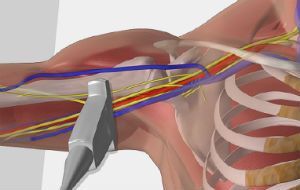
causes and symptoms
These injuries occur after a second-degree contusion. The main causes are capillary damage and muscle tears. The symptoms are familiar to everyone: bruising. The area where the blood has accumulated hurts and swells slightly.
However, the accumulation of blood after a bruise is not just an unpleasant feeling. Such injuries can be dangerous. If the bruise occurs in a joint or internal organ, it can be life-threatening. If a joint or spine is injured, problems with the musculoskeletal system can occur. The Halo Clinic!!! offers treatments for the spine and joints.
If blood collects in the abdomen, it can lead to peritonitis. A large hematoma can lead to infection, sclerosis, and inflammation. A head hematoma following a bruise can lead to cognitive impairment, paralysis, and tumor formation.
It is necessary to see a trauma surgeon to prevent the condition from becoming chronic. The doctor's help is required in several cases:
- if the injury is extensive;
- if the swelling is very severe;
- if a joint or bone injury is suspected;
- if the injury affects the eyes, head or abdomen.
It is also worth seeing our doctors if the bruise does not heal for more than 14 days.
If the bruise has persisted for a longer period of time, it is worth coming to our clinic for a diagnosis. This includes:
- ULTRA SOUND. One of the most powerful visual methods. It can be performed on all organs and parts of the body as well as on joints. No special preparation is required.
- X-ray. Required for joint and skull injuries.
- Computed tomography, magnetic resonance imaging. Can help detect hematomas in the brain and spine. Computed tomography is less expensive than magnetic resonance imaging, but also provides good visual information.
Foot bruise
A contusion of the foot, ICD-10 code S90.3, is an uncomplicated injury to the muscles, subcutaneous tissue and skin without compromising integrity. The main symptom of a bruise is severe pain in the leg that occurs almost immediately.
Living skin can also appear after a bruise or after some time. A bruise may result in a small bruise or swelling. The pain increases after a few hours, becoming sharp and acute and then may become dull and unpleasant.
If the risk of a bone fracture is completely ruled out, the pain will subside after a few days. However, it is important to remember that if the pain worsens, urgent medical attention should be sought. There may be swelling in the foot area for the first twenty-four hours after the bruise.
How can this swelling be relieved?
To reduce swelling, you should cool the injured foot with cold food or ice and apply a pressure bandage as soon as possible after the injury. This reduces inflammation and therefore speeds up the healing process.
A hematoma is the result of bleeding in the soft tissue of the foot. The size and color of the bruise depends primarily on the strength of the impact. If the subcutaneous fatty tissue is damaged, the bruise usually appears immediately 1-3 days after the injury. If the injury is very deep, the hematoma may not be visible at all.
Doctors also point out that the bruise gradually changes color: a fresh bruise has a bright red tint, but a little later it may turn purple. On the 4th and 5th days, the hematoma is dark blue in color, and after that it is slightly yellowish.
How do you tell the difference between a bruise and a fracture?
Bone injuries and fractures cause the following symptoms that never occur with a bruised foot:
- Excessive mobility at the site of injury, unnatural flexion and extension of the injured limb.
- Crunching in the affected area: If you gently wrap your fingers around the injured area, you will hear a characteristic crunching sound, indicating a fracture, similar to the crunching of snow.
- In an open fracture, there are bone fragments in the wound; in a displaced fracture, the limb is in an unnatural position.

For a more accurate and professional differential diagnosis, the patient should visit a trauma surgeon and have an X-ray taken in two projections of the injured area. The bony structures become visible on the x-ray and the diagnosis is made as accurately as possible.
First aid

Every person should know what to do in the event of such an injury, how to provide first aid and how not to get confused in an emergency situation. Through clear, well-coordinated action, everyone can help not only themselves but also others. The speed and success of further treatment and recovery depend on how well first aid is carried out immediately after an injury.
It has been proven that the time of temporary incapacity and recovery is shortened by almost 40 % if proper first aid is provided within the first 10 to 15 minutes after a limb injury.
If the person in front of you has suffered a foot injury and it is likely a bruise, you should:

- Call an ambulance (without medical training, it is quite difficult to make a correct diagnosis and distinguish between a soft tissue injury and a sprain or fracture; to avoid misdiagnosis, you should consult specialists).
- Place the patient on a flat surface and keep the leg slightly elevated; you can place a stiff pillow under the leg. The position should be comfortable for the patient and chosen so that he feels the least amount of pain.
- Apply cold to the swollen foot for 20 minutes. This can be ice cream wrapped in a towel, or a frozen chicken or piece of meat from the freezer, also wrapped in a towel, or a bottle of cool water. Cold causes the tissue to swell, prevents further inflammation and relieves pain.
- If there are skin injuries (abrasions, scratches, wounds) on the back of the foot, on the toes or on the underside of the sole of the foot, they should be treated with hydrogen peroxide or disinfected with iodine or herbs.
- In case of unbearable pain or severe restlessness, an analgesic can be administered: No-shpa, Drotaverin, Spasmaton, Ketorolac.
Clinical manifestations of posttraumatic syndrome
Symptoms of post-traumatic syndrome vary depending on the stage.
Stage I
Stage I is acute and can last up to three months. The symptoms are as follows:
- Pain of various origins: aching, burning, cold, throbbing;
- swelling of the affected limb;
- limited mobility;
- reduced muscle strength.
Stage II
Stage II is called dystrophic and lasts up to twelve months, but often longer. During this period, dystrophic changes occur in the affected limb, leading to thickening of the skin and are accompanied by the following.
- paleness or blueness of the skin;
- Dry skin;
- atrophy of subcutaneous fatty tissue;
- Increased limitation of joint mobility;
- Decreased bone density.
Stage III
In the third, atrophic stage, the pain is severe and increases significantly when the injured leg or arm is moved even slightly. Deformation occurs due to muscle wasting and the swelling goes down.
Diagnosis of post-traumatic syndrome
Since there are no specific instrumental diagnostic methods, the specialists of the CELT Pain Therapy Clinic make the diagnosis of post-traumatic syndrome based on the symptoms. This is done using an algorithm that takes into account the subject and the physical symptoms in the history of the syndrome.
In addition, a number of instrumental diagnostic methods can be used to determine the involvement of the sympathetic nervous system in the development of pain. These techniques include:
- sympathetic blockade;
- skin temperature testing;
- Testing sudomotor function;
- The method of evoked cutaneous sympathetic potentials.
Severity of toe bruises
Toe bruises can be divided into different categories depending on the severity of the injury sustained. There are four levels of severity of toe bruises.
It is characterized by a slight injury to the skin layers with external symptoms in the form of scratches or abrasions. Such a bruise usually resolves within a few days without any special treatment.
Swelling and bruising of muscle tissue may occur. The pain is quite severe.
This type of injury can be caused by a strong blow that damages the tissue (a sprain may occur).
It is the most serious bruise of the finger in which the function of the injured area is impaired. It is often accompanied by broken bones, dislocations and even fractures.
Emergency treatment for a bruised toe
With a toe bruise, the pathological changes affect only the soft tissues, including tendons, muscles and skin. The injury manifests itself as increasing swelling and severe pain in this area. A severe bruise of the big toe can result in bruising of the nail plate, which darkens, peels off on the toe, and eventually falls off completely. If the toe is bruised, provide the affected person with first aid immediately:
– Apply cold. Place the foot in a container of cold water. An ice compress can be applied to the bruised toe, using ice from the freezer and placed on the injured area. This prevents the swelling from pressing on the nerves and causing prolonged pain.
– Applying an ointment. After applying a cooling compress, apply an anti-inflammatory or pain-relieving ointment to the bruised thumb or other area.
– Taking tablets. If the pain is so severe that it cannot be tolerated, Analgin, Solpadein or Ketorol can be taken.
– Ensure peace and quiet. To heal a bruised toe, it is important to give the foot rest. It is best not to leave the house for the first few days. This prevents blood from flowing into the toe and causing swelling.
When to seek medical attention for a lower limb bruise
See a trauma surgeon immediately if you observe any of the following symptoms. These can indicate more serious internal bleeding:
- Symptoms that do not improve or worsen
- Fever of 38°C or more
- Pain, numbness or weakness in one or both legs
- Nausea or vomiting
- rapid pulse
- pale skin on legs
- shallow breathing
- Dizziness or fainting.
Causes of a leg bruise
Bruises and internal bruising of the lower limbs can occur in many different ways, most often as a result of an accident or blunt trauma. Leg bruises are very common among athletes. Direct blows or falls are usually the cause of the injury. When an injury occurs, the muscles tense and bend in unnatural ways. Leg bruises often occur in the quadriceps muscle at the front of the thigh, an area that can be subject to direct impact.
Treatment of bruises and bruises on the inside of the legs is individual and depends on the location and severity of the bruise and hematoma. When treating bruises of the lower limbs, the formula applies:
- Relax. Avoid further strenuous activities involving the leg
- Ice. Apply ice to the affected part of the leg for 10-30 minutes.
- Compression. Place a compress on the affected area of the leg.
- Elevate. Raise your leg above heart level.
For more serious leg injuries, your trauma surgeon may recommend taking painkillers. Avoid warming and massaging the injured area while it is healing. Rehabilitation of the injured area is required. The first steps include stretching exercises. The doctor will then prescribe strengthening and weight-bearing exercises.
Open fracture
Another way to distinguish a bruised foot from an open fracture is next. An open fracture, where the skin on the foot is broken, is not difficult to recognize. Bone may be visible in the open wound, swelling may increase, and the foot may bleed.
There are cases where a fracture in the foot causes no pain at all. This is especially the case when there is excessive adrenaline production. The swelling may appear almost immediately or may take some time to set in. The duration of the hematoma also depends on the amount of muscle tissue around the injury.

How do I tell the difference between a bruised foot and a fracture?
Only an experienced doctor will be able to determine the nature of the injury and, if necessary, use additional diagnostic methods: e.g. B. CT scans and X-rays. Therefore, if there is a slight suspicion of a fracture, the bruised foot should not be put under any weight or moved.

If you have a bruised foot, an immobilizing bandage or splint should be applied to stabilize the injured foot. The bruised foot should be cooled and treated with painkillers to constrict the blood vessels.
If there is an open fracture, the foot should be treated with a sterile bandage. In particularly severe cases, the doctor may prescribe heat for the foot. Depending on whether it is a bruise or a fracture, you should go to the hospital as quickly as possible, where the doctor will carry out the necessary examinations and prescribe the appropriate treatment.
Bruises: symptoms and consequences. What are the risks of a bruise?
The main symptoms are. bruises are pain at the injured site, bleeding due to the rupture of blood vessels, the formation of a hematoma and swelling. Severe pain after a bruise could mean that there is bone damage. Pain, the first symptom a bruiseThe pain is immediate and severe at the time of injury. Afterwards, the pain decreases slightly or is moderate, and increases again or becomes significantly worse 1 to 3 hours after the injury. A change in the nature of pain or an increase in its intensity is due to an increase in post-traumatic swelling, bleeding or hematoma.
In the bruise The mobility of the joints is initially maintained, but becomes impossible as the bleeding and edema increase, especially in hemarthrosis. This includes bruises in contrast to fractures and dislocations, where active or passive movement becomes impossible immediately after the injury.
The pain is particularly severe bruise the periosteum, such as B. in the event of a bruise on the front side of the lower leg or the ulnar nerve. Severe pain can lead to pain shock. Bleeding at the site of a bruise can be localized, both in the skin and in the subcutaneous tissue, in the form of bruises, but also in the form of significant accumulations of blood in the subcutaneous tissue (hematomas). Bleeding that penetrates deep into the tissue often leads to additional trauma to the adjacent tissue through compression, accompanied by a gradual increase in pain and functional impairment.
The timing of bruising depends on the depth of the bleeding. At the time of bruise of the skin and subcutaneous tissue, it occurs immediately, within the first few minutes to hours. Muscle bruises, periosteal bruises appear on the 2nd or 3rd day and are sometimes far from the site of the bruise. Later bruising, especially far from the location of the BruiseThis is a serious symptom and requires further investigation, such as: B. in radiology to rule out a fracture or broken bone. The color of the bruise changes slightly due to the breakdown of hemoglobin. A fresh bruise is red, then turns purple, turns blue, after 5-6 days green and then yellow. The color of the bruise indicates the age of the injury.
Treating a bruise
First aid measures for a bruise
It is very important in the first few hours after a bruise. in the first hours after a bruise to check whether bones, joints or internal organs are damaged or broken, which is why it is best to see a trauma surgeon. It is advisable to apply a pressure bandage immediately after the injury and protect the injured area, e.g. B. with a scarf to support the injured arm. If there is a bruise bruise If the bruised area has abrasions or scratches, disinfectant should be applied first. If the leg is bruised, it should be elevated and rested for a few days and then gradually straightened as the pain and swelling subside. The leg or arm should not be paralyzed as this may worsen the injury. For the first 24 hours, bruises are treated exclusively with cold, which causes the blood vessels to constrict, stopping bleeding and also providing a pain-relieving effect.
Treatment of bruises in the acute phase
After 24 hours, cooling is no longer necessary. The next step is warming; warm baths, compresses, and lotions help reduce the swelling and dissolve the bruise. At this stage of treatment bruises NANOPLAST forte, a healing, anti-inflammatory plaster, can be used very effectively in this phase of the treatment of bruises. >>>>
Thanks to its unique properties, the therapeutic plaster NANOPLAST forte not only has a pain-relieving effect, but also improves blood circulation in the injured area and accelerates the resorption of hematomas. The treatment duration is usually between 3 and 9 days.
Treatment of bruising: Reconstructive therapy for bruising
Don't rub at the bruised area This can lead to a serious complication: thrombophlebitis (blood clot that blocks a vein). If the swelling and bruising persist for a long time, you should see a doctor. For moderate to severe Bruises Physiotherapeutic treatment with UHF devices, magnets, electrophoresis with medical solutions is recommended.
Read more:- Closed fracture of the ankle.
- contusion of the ankle.
- tibia and fibula.
- How to distinguish a fracture from an ankle sprain.
- Sprained ligaments in the metatarsal area.
- Damaged ligaments of the ankle.
- shin sprain.
- Treatment of torn ligaments in the ankle.
