Water stimulates the excretion of salts and toxins and regenerates the tissue after intensive exercise. Dehydration is noticeable through spastic pain after exercise. You should increase your water intake to three liters per day. You can also take a few sips during training.
- hamstring tear
- clinical signs
- causes
- Fibrillation and muscle fasciculations
- Diagnosis and examination
- Free advice and diagnosis from the doctor
- Diseases of muscle tissue
- Lesions of nerve fibers
- treatment of pain
- prophylaxis
- preventive measures
- diagnostic procedures
- What treatment is possible?
- The most common causes
- Blood congestion in the veins
- Micronutrient deficiencies
- Why cramps in older women and men?
- surgical intervention
- rehabilitation period
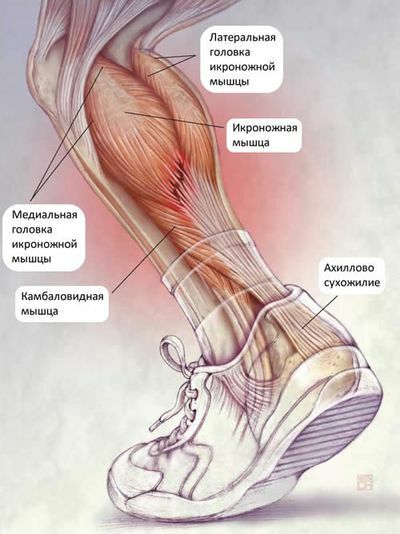
hamstring tear
A muscle tear is an injury that occurs when a muscle near the belly of the muscle or where the muscle meets the tendon suddenly contracts (falling) or is overused (lifting weights).
The thigh muscle is usually the most susceptible to rupture. The tear of the rectus abdominis muscle is not uncommon. It is caused by a fall backwards. A careless jump when running up can cause a torn calf muscle. There are also situations in which a rupture of muscle tissue leads to a bone fracture with significant displacement of bone fragments.
You can receive treatment for a torn calf muscle at the multidisciplinary CELT clinic. We have experienced specialists who will help you recover quickly from your injury.
clinical signs
Competitive athletes such as gymnasts, wrestlers, volleyball players, weight lifters, rowers, etc. are most likely to suffer muscle tears in the lower leg and other areas of the body. The symptoms of a muscle tear are primarily severe pain that is limited to the injured muscle.
- interruption of the muscle;
- A defect in the muscle that can be detected by examination and palpation;
- bulging of the muscle on the side opposite the tear in the form of a roll (in the case of a complete tear);
- Hematoma and swelling at the site of injury.
causes
- oncology of the brain and spinal cord;
- neuroinfections;
- Peripheral nerve damage;
- poisoning;
- Motor neuron disease.
In most cases, however, the muscle fasciculations are benign and not life-threatening. A muscle fascicle is an uncontrolled, visible, short contraction of a muscle. They are usually the result of heavy physical exertion, fatigue or stress. Fasciculations can occur in various parts of the body, e.g. B. on the eyelids, cheeks, lips and tongue.
Fibrillation and muscle fasciculations
A fibrillation is a spontaneous contraction of a specific muscle fiber that does not result in the contraction of the entire muscle. Fibrillations (unlike fasciculations) are not visible through the skin. At Yusupov Hospital, neurologists use very sensitive equipment to make a differential diagnosis between fibrillations and fasciculations.
In electromyography, fibrillation is detected as asynchronous, irregular, short (1-5 ms), low voltage (20-300 µV) discharges in the muscle (usually up to 30 discharges per 1 s).
- Traumatization of the body or axon of the motor neuron;
- Primary muscle diseases (myopathies).
- Muscle fasciculations can be seen on electromyography as longer discharges (8 to 20 ms) and higher voltages (2-6 mV). Fasciculations occur at irregular intervals (frequency 1-50/min).
In a healthy person, fasciculations occur during muscle relaxation: during, before or after sleep, at rest. These twitches disappear during active movement, but are recoverable when at rest. In contrast to fibrillations, they are not accompanied by muscle weakness, loss of sensitivity or atrophy of muscle tissue.
- Motor neuron diseases (ALS – amyotrophic lateral sclerosis, progressive spinal amyotrophy and others);
- Benign fascial syndromes;
- Painful muscular fasciitis syndrome;
- Traumatic root and peripheral nerve injuries or compressions;
- facial myokymia (brain tumor, multiple sclerosis);
- Isaacs syndrome (Isaacs syndrome);
- Some forms of facial hemispasm;
- Postparalytic contractures of facial muscles;
- Iatrogenic fasciculations.

Diagnosis and examination
Pain that doesn't go away on its own after exercise requires a visit to the doctor. After the diagnosis, the specialist will tell you how to treat the calf pain. The following examinations will be carried out:
- Laboratory tests of blood and urine:
- Ultrasound examination of the vessels of the lower extremities;
- MRI of the legs and spine;
- Electroneuromyography, an instrumental diagnostic to assess muscle contractility;
- Joint puncture.

The success of the treatment depends to 90 % on the doctor's experience and qualifications.
Free advice and diagnosis from the doctor
During the consultation, we carry out a thorough diagnosis of the entire spine and each of its segments. We determine exactly which segments and nerve roots are affected and cause the pain symptoms. As a result of the consultation, we make detailed treatment recommendations and, if necessary, prescribe additional diagnostics.
We carry out functional diagnostics of the spine
We carry out manipulations to significantly reduce the pain.
We put together an individual treatment program
Diseases of muscle tissue
Diseases of muscle tissue of various etiologies can also cause calf pain:
- Inflammatory processes of the calf muscles (myositis) – characterized by a pulling, aching pain that does not stop or occurs in spurts and increases with movement;
- Parasitic diseases (especially trichomoniasis) – characterized by muscle pain accompanied by facial swelling, fever, nausea, vomiting and diarrhea.
Lesions of nerve fibers
One of the symptoms of nerve inflammation and polyneuritis is a strong aching pain that occurs in attacks and begins to spread along the affected nerve. It can be caused by compression of the nerve roots. Its side effects are often:
- Trophic abnormalities in the innervated area (i.e., in the organs and tissues supplied by the nerves);
- numbness, tingling, or tingling;
- motor disorders in the innervated area;
- Loss of sensation.
treatment of pain
Our center has the most modern diagnostic equipment available for the treatment and diagnosis of calf pain. Qualified specialists apply individual treatment regimens for patients, using both standard and cutting-edge techniques, which produce excellent results and avoid side effects and relapses.
Types of treatment for calf pain depend on the diagnosed cause of the condition. In some cases, conservative treatment methods are used; Surgical intervention is very rarely required for this pathology. They help reduce inflammation, eliminate toxins, strengthen the ligamentous system, improve blood circulation and eliminate pain and swelling.
Key treatments for calf pain include:

acupuncture – This method relaxes muscle tension, reduces inflammation, relieves pain, reduces swelling and improves muscle and joint function.

massage – This is a very effective method of treating pain in the lower limbs. It helps to eliminate muscle spasms, relieves pain, increases mobility and muscle tension, and normalizes metabolic processes. As a rule, the doctor prescribes a massage treatment.

physical therapy (Ultrasound therapy, phonophoresis, electrophoresis, cryotherapy, shock wave therapy, magnet therapy, cold therapy, quantum therapy).
Depending on the individual indication, calf pain can be treated with the most effective combination of treatments, which may also include exercise therapy, phytotherapy, magnetic vacuum therapy, UWT, etc.
prophylaxis
Before deciding whether to immediately see a doctor for calf pain or whether rehabilitation at home is possible, you should try to determine the cause of the problem.
First of all, it is important to determine whether there has been a trauma, a bruise, hypothermia of the lower limbs recently, whether the body has been stressed by long walks, whether insomnia has occurred, whether there has been a lack of fluid in the body?
When such factors are present, dehydration, overexertion and stress can usually be reduced in calf pain:




If inflammation is suspected and the symptoms resemble trauma or vascular disease, foot baths and massages are contraindicated.
If you have acute, severe pain in your calf muscles, you should take painkillers. Gels and ointments for local pain relief have a good effect.
If acute pain in the calf muscles occurs frequently and for no reason, you should immediately consult a doctor. In some cases, self-treatment without medical supervision can lead to thrombosis, sepsis and other serious consequences.
So how can you get rid of calf pain preventively?
Doctors recommend the following preventive measures to protect the lower limbs from unwanted diseases:

preventive measures
To prevent muscle cramps, which are accompanied by pain, experts recommend muscle stretching exercises. Such an exercise is very simple.
To perform it, you have to stand about one meter away from a wall. Then the person has to bend forward to touch the wall. The feet should not be lifted off the ground for even a second. One should stay in this position for five seconds and then return to the starting position. The exercises should be performed three to four times a day for five minutes.
Training on a stationary bike is another effective preventive measure. This is especially advisable for people who are sedentary and lead a sedentary lifestyle.
Doctors also recommend wrapping your legs in a blanket when sleeping and drinking enough water every day to prevent it.
To avoid croup, you should also avoid alcohol, coffee and tea (or limit their consumption to a minimum) and, if possible, avoid taking medications that can trigger the syndrome.
diagnostic procedures
If the muscles contract regularly and severe pain occurs at the same time, a doctor must be consulted. It is also concerning if there is no obvious cause for this symptom (it is not related to exercise or prolonged sitting in an uncomfortable position).
A common reason people put off going to the doctor is because they don't know who can help them with their problem. The best thing to do is to contact your family doctor, who will refer you to a specialist:
After the initial examination, complaints and test results, your doctor will tell you which additional diagnostic methods are required. If you have abdominal cramps, you will be referred for an ultrasound scan, your back for an X-ray, your neck muscles or calves for a vascular Doppler scan.
What treatment is possible?
If diseases of internal organs that cause muscle spasms are identified, treatment of the underlying disease also treats the accompanying symptoms. Depending on the location, this may include medication, massage and physical therapy.
The uncontrolled use of antispasmodic medications (e.g., Neurontin) must not be taken uncontrolled. They are prescribed for patients with epilepsy. A person who has occasional cramps in the gluteus medius or neck area should not abuse these medications.
First aid also depends on the location of the cramp. With pain in the legs (from the buttocks to the feet), it is necessary to stretch the muscles, restore blood circulation and warm them up. The back should be rested. If the abdomen is affected, it is better not to take risks and consult the doctor immediately, especially for women who are aware of their pregnancy.
The most common causes
Leg cramps are caused by various peculiarities and abnormalities in the body:
- congestion of blood in the veins of the legs;
- micronutrient deficiencies;
- endocrine disorders;
- Long-term treatment with anti-inflammatory non-steroidal drugs;
- kidney disease;
- dehydration;
- extreme temperature fluctuations;
- taking diuretics;
- tight shoes, clothing;
- Physical and emotional overload.
Blood congestion in the veins
Cramps in the calf muscles can be a symptom of the development of varicose veins. If you experience swelling or heaviness in your legs, you should see a doctor. These are caused by venous blood congestion. The body tries to activate blood flow in the veins through muscle contractions. At this stage there are no visible symptoms of the disease. There are no balloon-like veins protruding from the skin, no spider veins. If treatment is started early, these will not occur and the cramps will not bother you at night.
Micronutrient deficiencies
Blood contains positively and negatively charged electrolytes, which conduct electrical charges necessary for transporting nutrients and oxygen to cells. If too little calcium, potassium, sodium or magnesium enters the body, the water-salt balance and the interaction of positive and negative molecules are disturbed. Uncontrolled reactions occur, causing muscle spasms. Cramps often occur in the calves, hips, feet, and hands.
Even if you eat a lot of vegetables and fruits and drink the vitamin and mineral complex prescribed by your doctor, you should take a test to check the biochemical and electrolytic composition of your blood. Minerals can enter the body, but are poorly absorbed if there is a lack of vitamins and fatty acids or if the diet is rich in protein, the breakdown of which accelerates the excretion of calcium from the body.
Why cramps in older women and men?
The body's ability to absorb micronutrients decreases with age. And even if the menu is based on the recommendations of nutritionists and contains a lot of vegetables, fruits and dairy products, older people may experience cramps in the hands, calves, feet and fingers due to a lack of calcium and other micronutrients.
Many people suffer from varicose veins as they age, and this disease causes cramps in the calves and thighs even in its early stages.
Another reason why cramps disrupt the sleep of older people is due to the use of medication. Doctors often prescribe diuretics and other medications that cause muscle spasms in older patients.
With a sedentary lifestyle, even light exercise, a long walk or gardening can cause fatigue, and sleep is interrupted by cramps several times a night.
surgical intervention
Treatment for a calf muscle strain, which is characterized by a tear of most of the fibers, is exclusively surgical. If the injured person is taken to a hospital in a timely manner (within 1 to 3 days), the surgeon stitches up the torn muscle and immobilizes the leg with a plaster cast for 2 to 3 weeks. After the rehabilitation measures, the functionality of the foot is completely restored after 1-3 months.
If the injured person underestimates the severity of his condition and does not report to the trauma center, this leads to shortening of the calf muscle, a reduction in its volume and degenerative processes in the adjacent connective tissue structures. Due to the inability to move properly, the patient eventually needs to seek medical attention. Since the muscle has already degenerated, it must be restored through plastic reconstruction using arthroscopy. The surgeon rebuilds the muscle tissue with a transplant.
rehabilitation period
Your doctor will develop a rehabilitation program to help you regain active muscle function. If you follow all the recommendations, recovery will speed up significantly. After a mild sprain, rehabilitation begins after 2 to 3 days using warming ointments. If the injury is severe, rehabilitation begins as soon as the cast is removed. What rehab specialists recommend
- Massage, classic or acupressure, to improve blood circulation and microcirculation;
- 5-10 sessions of physiotherapy: laser therapy, magnetic therapy, UHF therapy to increase the recovery rate of muscle fibers;
- therapeutic exercises and physical training to restore all functions of the torn muscle.
At the beginning of treatment, electroresection with analgesics, NSAIDs and calcium solutions is indicated to reduce the intensity of pain. If the sprain is associated with a joint or bone injury, cartilage-protecting agents are used during physical therapy.
Traumatologists recommend going to the hospital even if the ankle pain is only mild. The injured person is unable to assess the severity of the sprain himself or to determine the accompanying damage to the bone or the ligament-tendon apparatus. If the injury is not treated, it will worsen and lead to serious complications.
An informative video about recovering from an injury:
Read more:- Calf muscle cramps when walking.
- Acute pain in the calf muscle when running.
- How muscles and bones are related.
- The calf is constipated when running.
- abdominal muscle.
- The long fibula muscle hurts.
- Marfan syndrome in newborns.
- Treatment of short leg syndrome.
