Old60 years diagnosisOsteoporosis, osteoarthritis Result of treatmentNo pain

- pain in the muscles
- Treatment of muscle pain
- Types and causes of muscle cramps
- Types of muscle cramps
- Symptoms and diagnosis of muscle cramps
- Excessive GM impulses
- Excessive exertion
- How can I prevent cramps?
- Why do cramps occur during sleep?
- What should you do if you have leg cramps at night?
- Severe pain in the calf muscle
- causes
- pathogenesis
- Causes of myalgia
- Send request
- Send request
- Methods of diagnosis
- Which venous diseases cause leg pain?
- Diagnosis of pain
pain in the muscles
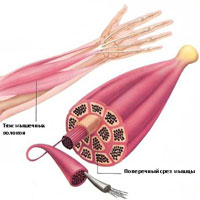
Muscle pain is uncomfortable and sometimes even unbearable. Why do they occur and how can they be treated? When the pain is severe, many people rush to the doctor, but when the pain is mild, not everyone rushes to a specialist. However, persistent, excruciating pain and muscle weakness can be a sign of the progression of chronic, including neurological, diseases.
Without prior diagnosis, it is difficult to determine why muscle pain occurs: the causes can be different. The most common include 1.2:
- intense physical exertion;
- persistent awkward or unnatural physiological postures;
- Poor posture is one of the causes of back pain in everyday life almost all year round, regardless of age and gender;
- Osteochondrosis of the spine, scoliosis, herniated discs;
- Inflammation of the back muscles themselves (myositis);
- radiculitis in the lumbosacral region;
- Bruises, injuries, muscle sprains;
- hypothermia;
- metabolic disorders;
- sustained strain on a muscle group, sustained static tension;
- viral, bacterial and fungal infections;
- systemic diseases (rheumatoid arthritis, lupus erythematosus, gout).
Muscle tension and constant pain are associated with a disease such as osteochondrosis. If the disease is not treated, the pain can occur even at rest and even at night 3 .
However, the most common cause of persistent muscle pain is skeletal muscle inflammation (myositis). It can be traumatic, infectious, caused by rheumatoid arthritis or parasitic infections 4 . The patient cannot distinguish between simple muscle pain and pain associated with a serious illness. Professional advice is therefore essential.
Calf and thigh muscle pain is caused by venous insufficiency and requires consultation with a phlebologist. Painful cramps also occur, signs of venous wall expansion in the legs 5 .
Treatment of muscle pain
The possibilities of modern medicine allow us to provide qualified help to patients with pain of any intensity. The most important thing is to start treatment at the right time.
If the pain occurs suddenly and is accompanied by swelling of the tissue, there may be an injury. To find out what triggered the pain attack, x-rays and MRIs should be done 6 . Only the doctor can determine the cause of the pain and select a therapeutic procedure.
After excessive physical exertion, intense sports training, delayed or delayed pain occurs, which is due to the accumulation of lactic acid in muscle tissue. This process is natural and requires no treatment 7. If pain persists at night or during the day for 3-5 days after exercise, you should get checked out.
Treatment depends on the diagnosis and the clinical picture. If the pain is inflammatory in nature, non-steroidal anti-inflammatory drugs 8 in tablet form and ointments are prescribed. If an infection is detected, antibiotics 9 may be used.
Types and causes of muscle cramps
Skeletal muscle cramps can be divided into four main types. These include 'true' convulsions, tetanic convulsions, spasms and dystonic convulsions. Seizures are differentiated based on the cause of the seizure and the muscle groups affected.
Types of muscle cramps
True 'convulsive' seizures. True cramps affect part or all of a muscle or groups of muscles that normally function together, such as: B. Muscles involved in the flexion of several adjacent fingers. Most researchers agree that true cramps are caused by overstimulation of the nerves that stimulate muscle contractions. They are by far the most common form of skeletal muscle cramps. True cramps can be triggered by a variety of circumstances.
injuries: Persistent muscle spasms can occur as a defense mechanism after an injury, such as a broken bone. In this case, the spasm usually serves to minimize movement and stabilize the injured area. An injury to the muscle itself can also lead to a muscle cramp.
Energetic activity: True cramps are usually associated with active muscle tension and muscle fatigue (during sports or unfamiliar activities). Such cramps can occur both during and after activity, sometimes many hours later. Additionally, muscle fatigue caused by sitting or lying in an uncomfortable position for a long time or by repetitive movements can also cause cramps. Older people are at higher risk of getting cramps when engaging in vigorous or strenuous physical activity.
Cramps at rest: Rest cramps are very common, especially in older people, but can occur at any age, including children. Rest cramps often occur at night. Although not life-threatening, nighttime cramps can be painful, disruptive to sleep, and occur frequently (i.e., many times per night and/or many nights per week). The actual cause of nighttime cramps is not known. Sometimes these cramps are triggered by a movement that causes the muscle to contract. An example of this would be extending the foot in bed, which causes shortening of the calf muscle, where cramps most commonly occur.
Symptoms and diagnosis of muscle cramps
What is characteristic is that the cramps are often very painful. The patient usually has to stop what he is doing and take urgent measures to relieve the spasm; the person cannot use the affected muscle during a cramp. Severe cramps may be accompanied by pain and swelling, sometimes lasting several days after the cramp has subsided. When a cramp occurs, the affected muscles are turgid, feel hard, and are painful to palpation.
Diagnosis of convulsions The diagnosis of muscle spasms is usually not difficult to make, but finding the cause may require a thorough history and instrumental and laboratory studies.
Excessive GM impulses
The 'culprit' of a seizure may be the brain itself, which sends excessive signals to the muscles. Patients with diseases associated with increased GM impulses suffer from persistent cramps:


Under the influence of caffeine and nicotine, excessive impulses emanating from the brain can occur. Night cramps often occur in people who abuse coffee, black tea, cocoa and chocolate, as well as in men and women who smoke cigarettes.
What should you do to eliminate the unpleasant symptoms? First of all, you should give up unhealthy habits and change your diet.

If this is not the cause of your severe leg cramps, you should see a neurologist.
Excessive exertion
Excessive muscle strain during the day can cause cramps both during the day and at night. Prolonged muscle work without rest occurs when:


Wearing even low heels for women results in an unnatural position of the foot, which tenses certain lower leg muscles. The increased stress on the calf muscles causes cramps in each leg at rest - at night or in the morning after sleep.
Important: Excessive strain on the calf muscles leads to a drop in ATP levels in the fiber structure and an accumulation of lactic acid.
Another cause that contributes to the risk of contractures is flat feet.

Abnormal arches result in abnormal load transfer from body weight to the support. The calf muscles are actively involved in the balancing process, becoming overloaded and causing painful cramps.
How can I prevent cramps?
To prevent cramps, the conditions that can cause this unpleasant symptom must be avoided. Women should wear comfortable shoes and men should avoid heavy physical activity, especially if they are genetically prone to varicose veins. If a person has a profession that requires standing for a long time, light exercises or massage of the lower limbs should be performed from time to time.

It is also important that you eat a healthy diet, take vitamin supplements if necessary, watch your weight and stop smoking. If you have cramps, do not rely on conventional medicine or advice from the Internet - it is better to see a doctor as soon as possible.
Why do cramps occur during sleep?

Although there is a widespread belief that mineral and vitamin deficiencies play a role, there is no solid evidence to support this belief. Comprehensive research has shown that treatment with vitamin and mineral supplements (calcium, magnesium, vitamin B12) does not help alleviate symptoms in most patients.
What are the causes of nighttime cramps in the feet, calves and thighs?
According to an investigation into the causes of nighttime cramps, daytime activity is an important factor. Athletes are at higher risk of experiencing cramps at night after being active during the day.
Excessive exertion and increased intensity of exercise can also cause cramps during waking hours.
Muscle fatigue, for example due to a long static posture, can also lead to nighttime cramps.
On the other hand, a predisposition to nocturnal muscle cramps can also result from inactivity. For example, sitting for long periods of time can cause muscle fibers to contract.
Lack of physical activity, that is, a person who does not stretch or actively use their muscles for a long period of time, increases the risk of cramps, which in this case often occur at rest.
Postures that restrict blood flow to the limbs can also trigger cramps: lying cross-legged or pressing on the leg. In such cases, it is worth experimenting with the position of the body in bed.
As you get older, you may experience leg cramps at night. As noted in a review published in BMC Family Practice, up to 33 % of people over 50 suffer from chronic nocturnal leg cramps.
The connection between pregnancy and leg cramps has long been known. It is due to the increased nutrient requirements and hormonal changes in the expectant mother's body.
What should you do if you have leg cramps at night?

For nighttime leg cramps, gentle stretches, self-massage, flexing and straightening the foot, and applying heat to the cramped area can help.
To prevent recurrence, we recommend light exercise (walking, swimming, cycling), drinking plenty of fluids throughout the day and taking care of your shoes. If nothing else works, you should see your doctor. Nighttime foot cramps can be a sign of illness.
Severe pain in the calf muscle
If you translate the Latin name of these muscles (gastrocnemius), it literally means shinbone. Take another look at your calves, because it is the calf muscles that give your legs their elongated shape. The calf muscle begins at the bottom of the thigh, just above the knee on the back. In the middle of the lower leg it connects to the Achilles tendon, which in turn connects to the heel bone. By targeting the fibers in the two heads of these muscles, they can lift body weight. This is important for controlled jumping, climbing and descending stairs and hills. More subtle functions include stabilizing the knee and ankle joints and controlling leg movement to maintain balance. Interestingly, the calf muscles generally have little involvement in the forward movement of the body; they mainly help with sudden movements from the ground. Signs of problems in the calf muscles can first be felt in the feet. The logic behind rebound pain seems to be that you have a sore spot that you need to pay attention to in order to stop the type of activity that is causing muscle fatigue.
Arch pain is the main symptom of calf muscle involvement (Figure 10.23). Pain originating from trigger point 1 can also reach the back of the calf, the knee, and the inside of the ankle (not shown). Trigger points elsewhere in the calf muscle cause pain primarily in the muscle itself (Figure 10.24). However, sometimes the highest trigger point also causes pain on the outside of the heel (not pictured). When trigger points shorten the muscle, it may be difficult to straighten the knee when the heel is on the ground.
These symptoms caused by myofascial trigger points are very common in children. Trigger points closer to the middle of the calf are more prone to nighttime cramps than those above. It is important to remember that nighttime leg cramps can have many other causes, such as: Vitamin deficiency, medication side effects and poor blood circulation. However, the musculo-fascial trigger points are the primary cause. Cramps can occur when walking or running because muscles that have lost elasticity affect blood circulation. Serious medical problems can often be identified by the same symptoms that occur with trigger points in the calf muscles. These include ruptured discs and tendons, posterior compartment syndrome (which prevents normal blood flow to the muscle), phlebitis, and cysts in the pocket behind the knee. However, signs of trigger points in the calf muscles can be misinterpreted as signs of one of these conditions if the doctor is unaware of the myofascial causes.
causes
The calf muscles are overworked by weight lifting, climbing and cycling. They get worn out during work when they bend over while standing for long periods of time, and then trigger points develop. Other causes include swimming with your toes pointed and hitting the water, the habit of wearing high-heeled shoes, and sitting on chairs when they press on the hips from behind and restrict blood flow. The main cause of calf muscle problems are benches and loungers that cause the Put strain on your calves. Lack of exercise due to a leg cast or lack of regular exercise also lead to trigger points. Diseases of the vestibular system lead to muscle stiffness and make them susceptible to overload. Cold weather predisposes them to excessive stress. Stretching your toes at night shortens your calves and contributes to cramps. This danger can be prevented by not wrapping a blanket under your feet.
The location of the calf muscles on the upper half of the shinbone is generally easy to identify by the shape of the calf. You can also feel the belly of the muscle with your fingers as you stretch your toes. For a precise, targeted massage of the calf muscles, use your toes with an Agravations, Noble, or Tera Kane device. When massaging with your toes, it is easiest to place your foot on a bed or chair (Fig. 10.25). A deep massage with the other knee is particularly effective on the back of the shin and is very easy to perform. This method can be performed supine or sitting with bare feet (Figs. 10.26 and 10.27). Simply move the foot down the knee in three or four parallel lines, starting at the ankle and moving toward the back of the knee. If you encounter a trigger point, work the area harder and go over it a few times with short strokes. Massage along and across the muscle. Ideally, you don't move the knee over the skin, but rather move it together with the knee. Poor conditioning is probably the main cause of calf muscle problems. When they are weak and stiff, they have little endurance and become overstretched. Remember that even therapeutic traction can have an adverse effect if the muscle remains tense under the influence of trigger points.
pathogenesis
The pathogenesis of myofascial pain varies greatly depending on the etiological factor and cannot be addressed within the scope of this article.
The classification is based on various criteria by which it is differentiated:
- Due to a pathological change in the musculoskeletal system: Fibromyalgia (primary sekundary), myositis (polymyositis), epidemic myalgia..
- By the nature of the course: acute, chronic.
- According to the location of pain: localized, diffuse.
- According to the level of the enzyme CPK (creatine phosphokinase) in the blood: with and without an increase in CPK activity.
Causes of myalgia
Myalgia can have many causes, the main ones being:
- Injuries (domestic, sporting, industrial) with damage to a muscle group causing acute muscle pain, e.g. B. acute pain in the calf muscle during a high jump.
- Physical overload (overexertion). Typical of athletes, but also common at home if you are not used to hard physical work that uses muscles that are normally little used.
- Long-term static stress (sitting in the same position).
- Overconditioning, especially in drafts.
- Severe stress and emotional breakdowns.
- Prolonged use of certain medications (Penicillins, Diazepam, L-Tryptophan, Calcium gluconate, Clofibrate, Nifedipine, Clonidine, Statins etc.).
- Infectious/parasitic diseases (e.g.Neuroinfections, flu, Trichinosis, Cysticercosis, Toxoplasmosis).
- Vascular diseases (atherosclerosis) are a common cause of calf pain, e.g. B. spastic claudication.
- metabolic disorders (Diabetes mellitus, Amyloidosis, Glycogenosis Etc.).
- Rheumatic diseases, e.g. B, Polyarteritis nodosa, systemic lupus erythematosus, Rheumatoid arthritis, systemic scleroderma, Polymyalgia rheumaticaMyalgias and pain all over the body.
- Poisoning (lead, alcohol, carbon monoxide).
- Potassium/calcium deficiency.
- Dermatomyositis/Polymyositis.
- osteochondrosis.
Send request
Send request
Your message has been sent successfully
Most cases of lower limb pain are caused by varicose veins. This disease is caused by a malfunction of the venous valves. This causes the blood to collect in the blood vessels and causes the following symptoms: tired and heavy legs, capillary network, swelling, cramps and pulsation of the affected veins.
In atherosclerosis The artery becomes clogged, blood supply to the extremity is cut off, and the surrounding tissue suffers from a lack of oxygen and nutrients. Pulsating pain occurs first in the lower leg and then throughout the leg (thighs, feet, toes). As the disease progresses, muscle wasting and gangrene occur.
thrombophlebitis Thrombophlebitis affects the large saphenous vein, but can also lead to inflammation in the deep veins. This causes throbbing pain accompanied by a burning sensation under the skin. These symptoms are persistent, especially in the lower leg. The danger of the disease is that clots form, which can break free and travel to vital organs in the bloodstream.
In venous insufficiency. the affected person feels a constant feeling of heaviness and congestion in the legs. Swelling occurs, the skin turns blue and the venous system protrudes. Subsequently, trophic disorders occur (eczema, trophic ulcers).
Methods of diagnosis

The most effective and accessible method is an examination in which the information is presented in a 3D volume. The MRI shows what is currently happening to the patient's spine, joints or other structures.

A method of quickly assessing the condition of internal structures by taking images using X-rays passing through the patient. Fast, inexpensive and informative.

Examination of the body using ultrasound waves. Ability to assess organs in motion. When passing through structures of different densities, the ultrasound is reflected from them - this creates an image of the condition at the time of the examination.

This is a blood test. Show me your tests and the doctor will tell you who you are. It is the fastest and most accurate way to find out everything about the biochemical processes in your body. Cost-effective, fast and effective.

Electrocardiography is the study of the electrical activity of the heart. Special electrodes are attached to the heart, and a cardiograph records changes in the heart's activity and displays them in the form of a cardiogram.
If vascular diseases are not treated in a timely manner, varicose veins can lead to trophic ulcers, gangrene and amputation of the limb. In the case of thrombophlebitis, this can lead to pulmonary embolism and death.
At the first signs of vascular disease, it is important to consult a doctor and conduct an examination using modern equipment: vascular ultrasound, duplex angioscopy, angiography, CT, MRI.
The first stages of vascular disease are treated conservatively: taking non-steroidal anti-inflammatory drugs, desegregants, anticoagulants, venotonics, enzymes, physical therapy, physiotherapy, special diet, compression garments. For advanced vascular diseases, surgical interventions are used: phlebectomy, sclerotherapy, laser coagulation, radiofrequency current ablation.
Which venous diseases cause leg pain?
There are several common venous diseases that can cause leg pain of varying intensity and location, including
- Varicose veins (varices) are characterized by a local expansion of the walls of the superficial veins. For a long time, these enlarged veins do not cause any discomfort, but when they become inflamed, they cause Pain in the calf muscles when walking.The skin in the area of the dilated veins becomes more porous. The skin in the area of the dilated veins becomes red (hyperemic), swollen, the visible nodules become thick and hot to the touch.
- Phlebitis is an inflammation of the walls of superficial and deep veins caused by various factors (infection, trauma, hereditary predisposition). It is characterized by the following symptoms Severe pain in the calf muscle when walking. The intensity of the pain decreases slightly when the leg is elevated. The skin is also red and swollen, but no nodular changes are visible in the superficial veins.
- Thrombophlebitis or deep vein thrombosis is a serious disease in which an insoluble thrombus forms inside the vessel following an inflammatory reaction. The thrombus leads to an acute outflow of blood. This is accompanied by acute pain in the calf muscle. It is worse when walking and eases somewhat with rest. The main danger of thrombophlebitis or thrombosis is the development of thromboembolism (a condition in which a clot detaches from the vascular wall, enters the bloodstream and clogs the arterial vessels, causing serious damage to the blood supply to various organs and tissues). Thromboembolic disease can lead to a heart attack, stroke, or blockage of a pulmonary artery. It can also be fatal if blood flow is interrupted in a large artery.
Diagnosis of pain
The phlebologist in the 1st surgical department of the SKZD hospital during the initial examination carries out a thorough examination and palpation of the tissue in the area of \u200b\u200bthe pathological process. Based on the results of the clinical examination, he makes an initial assessment and then prescribes additional diagnostics to visualize the venous vessels (phlebography).
Once the cause of pain, location and severity of the venous disease is determined, the phlebologist prescribes appropriate treatment. This may include conservative pharmacotherapy (anti-inflammatory drugs, anticoagulants) and surgical removal of the affected areas.
Read more:- Acute pain in the calf muscle when running.
- Pain in short fibula when walking.
- Why do your calves hurt when you run?.
- The calf is constipated when running.
- Sore muscles in the calf.
- Leg Discomfort – Which Doctor Should I See?.
- Shuffling Feet While Walking Causes.
- Orthopedic knee orthoses for osteoarthritis when walking.
