Traumatic hemarthrosis occurs when the ligaments are severely damaged and the joint capsule is torn. This is called hemorrhage into the joint cavity, which occurs due to a rupture in the vessels that supply blood to the internal structures of the joint. The bleeding can cause destructive and degenerative tissue changes. A puncture is performed and the cavity is protected with antiseptics to remove the accumulated blood.
- Closed ankle injuries
- Short description
- Clinic automation: fast and cheap!
- classification
- Causes of ankle and ankle injuries
- Symptoms of ankle injuries in children
- Pathogenesis of a joint bruise
- Bruised shoulder joint
- Bruise of the angle joint
- How does a sprain of the ankle ligaments manifest itself?
- Medical treatment of injuries
- Medicines used for foot injuries
- signs
- Treatment
- Depending on the severity of the injury and the type of damage, each type of ankle injury is classified into the following grades:
- a – Injury Grade I:
- Main principles of treatment
- Duration of treatment
Closed ankle injuries
ICD categories: Other superficial ankle and foot injuries (S90.8), Multiple superficial ankle and foot injuries (S90.7), Superficial ankle and foot injuries, unspecified (S90.9), Ligament tears of the ankle and foot (S93. 2), strain and strain of the ankle (S93.4), injury to another muscle and tendon of the ankle and foot (S96.8), injury to multiple muscles and tendons of the ankle and foot (S96. 7), injury to unspecified muscles and tendons of the ankle and foot (S96.9), injury to own muscles and tendons of the ankle and foot (S96.2), ankle contusion (S90.0)
Short description
Closed ankle injuries – Injury to structures of the ankle joint without skin injury [1].
Patient category: Adults with closed ankle injuries.
Users of the protocol: Orthopedic traumatologists, surgeons, general practitioners, emergency doctors, paramedics.
Class I – the usefulness and effectiveness of the diagnostic method or treatment measure has been proven and/or generally accepted
Class III - the available evidence or general consensus suggests that the treatment is not useful/effective and may even be harmful in some cases
B - Results from a single randomized clinical trial or large non-randomized trials
C – General expert opinion and/or results from small studies, retrospective studies, registries.

Clinic automation: fast and cheap!
– 800 RUB / 5,500 KZT / 27 BYN – 1 order per month

classification
II. DIAGNOSTIC AND THERAPEUTIC METHODS, APPROACHES AND PROCEDURES
MRI of the ankle joint (indications: torn, dislocated and damaged ankle ligaments).
Minimum list of examinations to be carried out at the time of referral for a planned hospitalization: A planned hospitalization will not be carried out.
1. Magnetic resonance imaging of the ankle joint (indications: torn, dislocated and damaged ankle ligaments)
1 Collection of complaints and anamnesis, physical examination.
Complaints: Pain in the ankle joint, impairment of motor function in the ankle joint.
Medical history: Presence of trauma with a direct (fall on foot) or indirect (acute rotation of the tibia while the foot is standing) mechanism of injury.
– X-ray of the ankle joint in two projections: no bony pathology, but secondary signs of soft tissue damage: widening of the joint space, spreading of the syndesmosis.
– MRI: Signs of damage to the ligamentous apparatus of the capsule and tendons are detected.
Causes of ankle and ankle injuries
Most injuries are caused by falls of all kinds, be it from a height, from a bicycle or from your own height. A child can trip, slip, fall - literally every situation carries the risk of a bruise.
Other possible causes of injury include:
- traffic accidents involving children;
- Accidents involving children (building collapse, fires, floods, etc.).
- physical impacts from other children or adults
- direct external influences on the ankle or ankle joint, e.g. B. by a speeding ball or stone;
- Sports, dancing, extreme sports and contact games.
The ankle joint as well as the heels, knuckles and knuckles in children vary in their susceptibility to bruising. The skin, ligaments and tendons, for example, are more resilient and less susceptible to injury. The loose subcutaneous fatty tissue and muscle structures suffer most from the impacts.
Symptoms of ankle injuries in children
In such an injury, the bones remain intact and only the soft tissues are damaged, while the muscle fibers and cartilage parts are affected by the strong impact. Immediately after the injury, acute pain occurs, which gradually subsides and only starts again when pressure or active movement is attempted.
Symptoms of a bruised ankle, heel and ankle also include.
- Severe swelling, swelling at the site of injury;
- Redness of the skin, bruising of the skin and formation of bruises with red, purple and sometimes bluish discoloration
- Increased body temperature in the joint area;
- Abrasions, abrasions and other skin injuries.
A child with this type of injury cannot move independently and complains of pain, numbness, and decreased feeling in the lower leg when attempting to support the limb.
Pathogenesis of a joint bruise
A contusion is caused by the impact of a moving solid object with low kinetic energy (in a contusion caused by a fall, it is not the object or surface that has the kinetic energy, but the human body). The individual tissues have different levels of resistance to such an impact. Hard skin, fascia, tendons and ligaments remain intact or almost intact. Loose tissue and soft muscle tissue are most affected.
Small tears, bruises and stretches occur in the tissues. Blood from the damaged small vessels flows into the skin, muscle and subcutaneous fatty tissue and bruises (hemorrhages) form. Aseptic inflammation occurs, the amount of fluid in the spaces increases and edema forms. If medium-sized vessels are damaged and bleeding is more severe, hematomas – limited spaces filled with blood – can form.
Even if there is no major damage, joint bruises often affect not only the superficial soft tissues, but also intra-articular structures such as the synovial membrane, cartilage, ligaments and the joint capsule. Microdamage to the synovial membrane is the most common. Bleeding occurs in the synovial membrane, blood flows from the damaged blood vessels into the joint cavity and hemarthrosis develops. The blood cells begin to decompose, fibrin fibers form in the joint cavity and the breakdown products are absorbed into the surrounding tissue.
The cartilage and soft tissues of the joint become less supple and partially lose their elasticity, which can lead to recurrent synovitis and arthritic changes in the long term. Microdamage to hyaline cartilage is another cause of the long-term consequences of a joint contusion. When a bruise occurs, small fragments of cartilage detach from the surface and form intra-articular bodies, and the cartilage itself loses its suppleness in the areas of the crack.
Bruised shoulder joint
Usually caused by an impact or collision with an immovable object (e.g. a door frame), less commonly by a fall. The pain is intense at the time of injury, subsides, and then returns with increasing swelling. The size of the swelling can vary greatly. With minor injuries, the swelling is barely visible, with severe joint contusions there may be a significant enlargement of the affected area due to bleeding from the deltoid muscle, swelling of the deltoid muscle, and accumulation of blood in the joint.
A bruise of the joint is distinguished from a dislocation of the shoulder, a tear of the large hump and a fracture of the neck of the humerus. Indications of a bruise include preservation of the joint configuration, the absence of pain in the shoulder when tapping the elbow, and a slight limitation of movement (the patient can pull the arm back and raise it forward quite freely). No changes can be seen on the x-ray images of the shoulder joint. Treatment includes NSAIDs in the form of tablets and topicals, rest (a splint in severe cases), cold followed by UHF and dry heat. A puncture of the shoulder joint is usually not necessary.
Bruise of the angle joint
symptoms bruises, sprains, contortion i fractures are very similar, which is why many people waste valuable time trying to treat ligament strains and tears at home. However, self-treatment by applying a bandage or cold compress to the painful area can only be carried out if you are sure that the injured person has not suffered a fracture, tear or sprain.
bruises – The most common type of injury, which can occur in isolation or be associated with other, more serious injuries such as fractures, dislocations, damage to internal organs, etc. A bruise is usually the result of hitting a heavy object or falling from a height. The most common type of injury is damage to the skin and subcutaneous tissue, but internal organ bruising can also occur. These include, for example, the brain, heart, kidneys, liver and lungs.
Main Symptoms of a bruise – Pain, swelling, tissue bleeding, bruising and functional limitations. The pain occurs immediately after the injury and can be quite severe; after a few hours the pain subsides. How long it takes for a bruise to appear depends on its depth. Subcutaneous and cutaneous bruises bleed immediately and the bruise is visible within a few minutes, while for deeper bleeding the bruise may not become visible for two or three days.
damage of a bruise They usually occur as the swelling and hematoma progress. The ability to move the injured part of the body is gradually lost. For example, a person cannot bend an injured leg or arm on their own because of the acute pain, but if another person helps them, the limb can be bent, although this is also painful. This is in contrast to fractures and sprains, where the injured limb cannot be moved immediately, either alone or with the help of another person.
Self-treatment of bruises is also possible Bruises can also be treated yourself. To reduce swelling and bruising, apply a cold compress to the injured area immediately after the injury and allow it to rest. You can hold the bruised area under cold running water, bandage it with a wet towel, or apply ice or a cold water bottle. Apply a pressure bandage to limit movement around the joint and place the limb in an elevated position.
How does a sprain of the ankle ligaments manifest itself?
Individual ligament fibers in the ankle joint can cause mild symptoms, as opposed to completely torn ligaments in the ankle joint.
The main clinical symptom is pain when walking or trying to move the foot. The severity of the pain syndrome can vary from patient to patient. Palpating the injured area is also painful. With an ankle sprain, the patient is usually able to walk despite the pain.
Examination of the injured area reveals local swelling. In some cases, slight bruising may be noted. A sprain can be distinguished from a complete ligament tear by the extent of the bruise, which in a complete tear extends to the sole and back of the foot. In addition, with a complete rupture, the swelling is much more severe and also affects the foot.
Medical treatment of injuries

Immediately after the injury, a cold compress should be applied to the injured area. It is advisable to immobilize the ankle joint with a tight eight-point bandage. The more correctly the bandage is applied, the more effective it is. In addition, the load on the leg should be limited.
To relieve inflammation, pain and swelling, non-steroidal anti-inflammatory drugs are prescribed in the form of ointments, gels and creams.
In addition, a bioregulatory ointment containing a number of herbal and mineral ingredients - arnica, monkshood, belladonna, echinacea, etc. - can be used. In 2016, researchers at the University Hospital of the Technical University of Munich published a paper in which they demonstrated the effectiveness of this drug in diseases and injuries of the musculoskeletal system.
It is important to remember that the use of any medication is possible only after prior consultation with a doctor.
Physiotherapeutic treatment can be started around the second or third day after the injury. These can include magnet therapy, thermal applications with ozokerite or medicinal paraffin, and others.
On average, with an ankle sprain, functionality in the injured area is restored after one to two weeks.
Medicines used for foot injuries

Available in ointment and gel form. One of the main non-steroidal anti-inflammatory drugs. Has a pain-relieving, decongestant and fever-reducing effect. Can be used for sprains and bruises from the first day of the injury.

It has an anesthetic and anti-inflammatory effect. The ointment is used for bruises and sprains, as well as complications of injuries. For example, dimethoxide can help with infiltrates, abscesses, etc. However, the antiseptic effect is only moderate, so it is not suitable for primary wound care.

The ointment is applied on the 2nd or 3rd day after the injury. It helps dissolve infiltrates, relieve swelling and reduce hematomas. It is particularly useful if there is an injury to the toenail and blood is collecting underneath.

Refers to non-steroidal anti-inflammatory drugs. In ointment form, it helps relieve swelling and pain. It can be used immediately after an injury, which is why ibuprofen along with diclofenac is very popular among athletes.
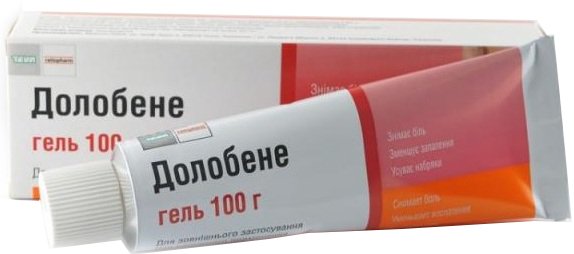
The ointment contains dimethyl sulfoxide, heparin and dexpanthenol. So it works in several directions at the same time. Dimethyl sulfoxide has an analgesic and anti-inflammatory effect, heparin helps to reduce hematomas, and dexpanthenol improves metabolic processes and promotes rapid regeneration of the foot.

It relieves pain and reduces swelling. It is most commonly used for bruises and sprains of muscles and tendons. It also has an anti-inflammatory effect, so can help with synovitis and other joint injuries. Used immediately after injury and until full recovery.
signs
Symptoms of an ankle injury depend on the type and extent of the injury.
An ankle sprain causes a sudden increase in swelling and severe pain when turning the foot and palpating it.
- The lateral malleolus is painful to feel below and at the ankle;
- In both ankles, any attempt to move the ankle is painful, and the pain is audible along with the crunching of the ankle joint with movement;
- In the heel bone: The injured person cannot stand up due to pain in the heel;
- the metatarsals; Acute pain when putting pressure on the forefoot and when palpating the foot.
An ankle sprain is characterized by visible deformity, pain, and swelling, and the foot is displaced inward, outward, or backward.
Depending on the severity of the injury, three degrees can be distinguished:
- I (mild) – the dislocation is slightly swollen and tender, without fracture, without joint instability and noticeable impairment of foot function;
- II (moderate) – partial tear of the ligament, characterized by moderate pain, swelling, mild impairment of foot function and joint instability (intra-articular bleeding is also possible and pain increases with loading);
- III (severe) - complete rupture of the ligament with extensive swelling, subcutaneous hemorrhage, severe pain, loss of function of the foot and significant instability of the joint (bleeding, inability to support the limb).
A chronic ankle ligament injury is associated with swelling of the ankle, pain when walking and running, swelling, and instability of the joint.
Treatment
At First Medical Clinic we offer conservative treatment of ankle injuries using the most effective and safe methods:
- drug blockages – Injection of anesthetics directly into the area of most pain
- local injection therapy – Injection of painkillers, anti-inflammatory agents and other medications into the joint cavity;
- intra-articular injections Hyaluronic acid (relieves pain and accelerates recovery of function in ankle fractures);
- Bio Osteo Bio Implant – Injection of multipotent mesenchymal stromal cells from the patient's adipose tissue into the damaged area, which promotes tissue regeneration and injury healing;
- Injection of platelet-derived autoplasma into the damaged joint or surrounding tissue (auto plasma therapy), etc.
The use of autoplasmin not only helps tissue heal after an injury, but also prevents the development of complications such as post-traumatic ankle arthritis. It is also effective in treating an already developed degenerative and dystrophic process.
The necessary scope of therapy can only be determined by a specialist after the diagnosis. We recommend that you visit First Medical Clinic early for treatment of your ankle injury.
You can arrange a consultation and an appointment at the following number
Depending on the severity of the injury and the type of damage, each type of ankle injury is classified into the following grades:
- Acute ankle injuries
- I. Injuries to the ankle joint due to indirect traumatic impact:
- (a) abduction variant (pronation) (grades I, II, III);
- (b) Adduction variant (supination) (grades I, II, III).
Acute ankle injuries can be open or closed.
Injuries to the ankle include acute for the duration of the injury up to 10-20 days i chronicIf the time that has passed since the injury more than 20 days.
The diagnosis of ankle injuries is made based on the nature and mechanism of the injury, the clinical picture and mandatory X-ray examination in two projections.
In some cases, a special radiological examination (with 'loading') is carried out in which the foot is placed in a position that places stress on the ligaments required for the examination (intercondylar syndesmosis, external or internal collateral ligaments) in order to strengthen the ligaments of the ankle joint which is clearly visible on the x-rays.
Fractures of the ankle joint are intra-articular in nature.
Therefore, the precise reduction of the fracture fragments must be carried out with great care in order to restore the entire articular surface and all ligamentous parts of the joint, hold the fracture until complete healing and enable comprehensive rehabilitation.
a – injury Grade I:
- Tear (microscopic tears) of the ligament causing local pain and minimal swelling, with little mobility and stability of the joint. However, the joint can be put under strain and the x-rays show no abnormalities.

Main principles of treatment
Only conservative methods are used to treat Grade 1 and 2 ankle ligament tears. Patients are not recommended to wear bandages throughout the treatment period. After cold compresses, ointments containing anti-inflammatory nonsteroidal drugs such as Voltaren, Fastum, Indomethacin are prescribed. These relieve swelling and inflammation and make pain disappear quickly. The therapy regimen should also include means to improve blood circulation:
The dosage regimen depends on the severity of the ligament injury. As a rule, it is enough to apply an external agent 2-4 times a day to dissolve the hematoma or swelling. After 3-4 days, patients are recommended to use ointments with a warming effect: Finalgon, Viprosal, Capsicam. Their action improves microcirculation and nutrients begin to reach the damaged ligaments, accelerating their healing.
Immediately after the diagnosis of a grade 3 ligament tear or complete separation of the ligament from the bone, a surgical operation is performed. During the rehabilitation period, the patient is prescribed a course of venotonics (Phlebodia, Detralex) to restore blood circulation in the damaged ankle joint.
Main symptoms of a torn ankle ligament Pharmacological treatment to eliminate them Pain syndrome Nonsteroidal anti-inflammatory drugs in the form of ointments, tablets, capsules – Ibuprofen, Diclofenac, Meloxicam, Ketorolac, Nimesulide, Piroxicam swelling Products for restoring blood circulation and microcirculation – Indovazin, Heparin ointment, Phlebodia, Detralex hematoma Drugs to normalize blood vessel permeability – Troxerutin gel, Troxevasin, Lyoton Duration of treatment
Trauma patients are primarily interested in how long it takes for a torn ankle ligament to heal. Even an experienced doctor can only give approximate treatment and rehabilitation times. The patient's age is of great importance. Children have an accelerated metabolism and therefore recover 1.5-2 times faster than adults. Older patients have a slower metabolism, which affects the rate of regeneration of damaged tissue. When predicting the prognosis, the traumatologist takes into account, among other things
- the extent of injuries to ligaments and tendons;
- the state of the injured person's immune system;
- the history of acute or chronic illnesses.
A diabetic, for example, has a very slow metabolism. Therefore, even a minor injury may require him to be hospitalized. The injured person is being treated in the hospital under the supervision of medical staff.
The symptoms of a grade 1 ligament tear subside completely after 2-5 days. Sometimes a small bruise or swelling remains, but there is little pain when walking. The speed of recovery depends on the quality of treatment and monitoring of the patient's recovery dynamics. After 3-4 weeks of treatment, people with Grade II or II ligament tears can return to normal activities of daily living. In rare cases, the rehabilitation period lasts longer than 2-3 months.
How long it takes to heal an ankle sprain also depends on the discipline of the patient. If he strictly follows the doctor's instructions, full recovery will occur much faster.
- Closed Foot Injury.
- dislocation of the ankle.
- Injury to the ligaments of the ankle.
- ligaments of the ankle.
- Damaged ligaments of the ankle.
- Ankle ligament strain, ICD.
- Structure of the human ankle.
- The ankle bruise is where the picture is taken.
