As part of rehabilitation after a leg injury, it is important to work on restoring walking. One of the most effective options is training on an exercise bike, which the doctor must allow the patient to do if there are no contraindications.
- Exercise therapy after an ankle fracture
- Physiotherapeutic recommendations after a foot fracture
- Characteristics of the injury
- Clinical implications
- symptoms
- First symptoms
- Obvious symptoms
- Dangerous Symptoms
- What are the risks of post-traumatic arthritis?
- Characteristics
- complications
- Ankle fracture: symptoms and first aid
- First-class care: what modern diapers can do
- First aid and treatment for broken ankles
- diagnosis and treatment
- First aid
- diagnosis
- Treatment
- Rehabilitation period.
- Specific symptoms
- Rehabilitation after a displaced ankle fracture (after cast removal)
- How is the foot rebuilt after an ankle fracture?
- Types of Ankle Injuries
- Consequences and complications of ankle injuries
- Nourishment
- massage
Exercise therapy after an ankle fracture
A fracture of the ankle requires a relatively long rehabilitation period. More than 10 % of all skeletal injuries are believed to occur in this area. In order to restore function to the injured foot more quickly, a number of measures must be taken.
Rehabilitation after a broken foot bone depends on the type and complexity of the injury itself. A fracture can be open or closed, with or without displacement. Depending on the fault line, they are divided into these types:
If the bone is exposed to strong external influences, e.g. For example, if the foot hits a hard surface or a heavy object falls, it is called a traumatic fracture. Some diseases or complications of diseases reduce calcium levels and bone strength, leading to a fracture. Such fractures are called pathological fractures.
The main symptoms that accompany a fracture include severe pain, swelling, and bruising in the injured area. The pain increases every time you put pressure on the injured leg.
Physiotherapeutic recommendations after a foot fracture
Rehabilitation after a foot fracture has the following goals for the patient
- restoring mobility of the foot;
- Activation of ligament and muscle tone in the injured area;
- strengthening the base of the ankle joint;
- elimination of puffiness and activation of metabolic processes;
- Return to normal gait.
- Therapeutic physiotherapy – a set of physical and gymnastic exercises;
- massages;
- orthopedic shoes, splints;
- a drinking regime (at least two liters per day).
Therapeutic exercises are recommended from the first day of the injury and continued for several months until full recovery.
Characteristics of the injury
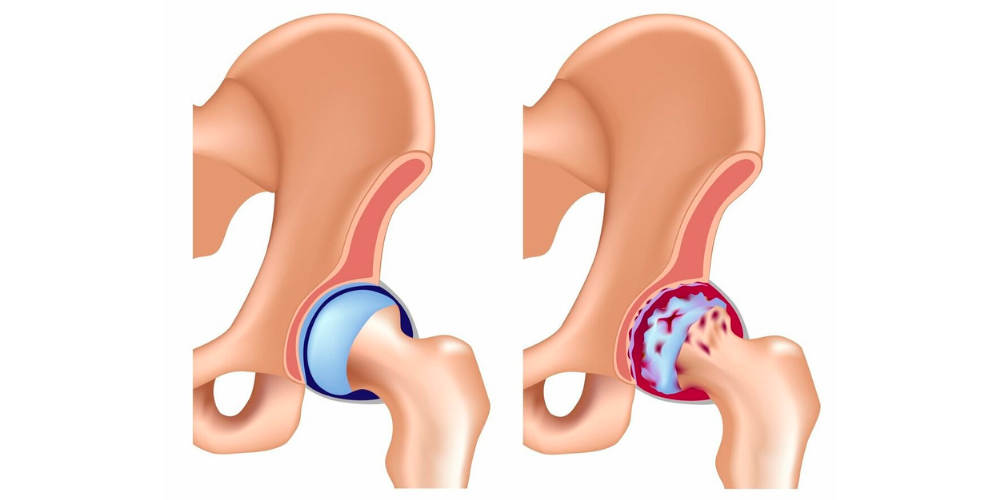
If there is a small ankle fracture, there is a risk that the limb will be completely immobilized. Any attempt to move this limb causes pain along the entire length of the leg as the numerous nerves in the injured area respond to the injury. Anatomically, the ankle joint consists of two pairs of bones, the outer (lateral) and the inner (medial) ankle. Immediately below is the talus, which is connected to the fibula by the fibula-foot ligament. As with a fracture, it is not uncommon for bone fragments to form and become displaced and for important connective structures of the foot and lower leg (ankle, ligaments, tendons) to be damaged. There are few blood vessels in this area, but injury to them is extremely dangerous.
The special thing about this injury is that it is very easy to sustain. All it takes is one careless twisting of the leg and you can not only sprain but also break your ankle. The proximity to the skin means that an open injury is likely if a large splinter breaks off and breaks the skin.
Clinical implications
Diagnosing the injury is not difficult as it has fairly clear clinical signs. For example, a fracture often occurs in people who regularly put a lot of strain on the musculoskeletal system. These include professional athletes, athletes, people in professions that require good physical preparation and high activity. In this case, fatigue damage can occur. This means that the bones are worn down by regular stress and can no longer regenerate with repeated stress. Any careless action can cause a fracture or even a fracture.
Weakness in the ankle joint caused by the body can lead to injuries even with the slightest mechanical impact. A trip during a walk, a careless step and a twisted foot – these possibilities are diverse. Sharp blows, bruises, etc. can also be a source of injury. However, it is not uncommon for a fracture to be accompanied by other related injuries:
- stretching of neighboring ligaments;
- Damage to the joint structure (fracture, loss of joint or even partial tear);
- Permanent fractures, etc.
symptoms
Post-traumatic arthritis develops gradually, and in most cases the patient does not pay attention to the first mild symptoms.
First symptoms
The first symptoms appear some time after the injury. This period is shorter for larger injuries and longer for smaller and micro injuries. In the morning, the affected person notices mild pain and stiffness. They pass very quickly after the start of movement and do not return during the day, so most patients do not pay attention to them and do not associate them in any way with a once forgotten injury. However, if you pay attention to your health, these symptoms may be noticed and a consultation with an orthopedist/traumatologist becomes necessary.

Obvious symptoms
The pain occurs with prolonged exertion, such as when standing or walking. Initially, this pain goes away quickly with rest, but over time it lasts longer and longer. The pain is sensitive to changes in the weather and can also cause joint pain and insomnia. The next stage is movement - then the characteristic cracking of the joint occurs, which indicates changes in the cartilage.
Periodically the joint swells, the skin over the joint becomes slightly red and the pain increases. This is a symptom of aseptic arthritis or synovitis - inflammation of the synovial membrane as a result of prolonged trauma. The exacerbations can resolve spontaneously when the stress is reduced. After some time, the patient notices that the shape of the joint has changed and he has difficulty bending and stretching.
Dangerous Symptoms
Don't hesitate to see a specialist if
- increasing pain in the joint;
- Pain and discomfort when flexing and extending the joint in the morning;
- Redness and swelling of the soft tissues over an already injured joint;
- Changes in the shape of the joint.
What are the risks of post-traumatic arthritis?
The main risks are the slow, imperceptible progression of the disease and the high risk of disability.
Characteristics
Every location and every form of osteoarthritis brings with it serious complications, so treatment must not be delayed.
There are several classifications of post-traumatic osteoarthritis, depending on the degree or stage of progression. The classification of prof. Kosinka, introduced 60 years ago, is most commonly used by professionals:
- Level I (Grade) – Initial. Complaints of pain and morning stiffness in the affected joint. The pain occurs even when there is significant strain on the joint, but subsides quickly with rest. X-rays show no change or a slight narrowing of the joint stroma.
- II – obvious. The pain increases and lasts longer after exertion. There is a crunch in the joint and some limitation of movement. The x-rays show narrowing of the joint space, sclerosis of the bony joint surface and isolated osteophytes.
- III – final. The pain syndrome is constant and increases with exertion. The joint is periodically swollen, the skin over the joint reddens, and pain increases (exacerbation as aseptic arthritis). Exacerbations can be left untreated, but the pain increases and becomes constant. The shape of the joint is changed, function is impaired and movement is severely restricted. At the end of this stage, the joint is no longer functional. On the X-ray, the joint space is almost absent, the bony surfaces are fused (very often abnormal), large osteophytes on the edges of the joint change its shape.
complications
Osteoarthritis of the joint after trauma progresses faster than other similar lesions and is more likely to lead to complications. This includes:
- instability of the joint;
- Persistent and pronounced pain syndrome;
- Recurrent exacerbations – synovitis and arthritis – which promote disease progression;
- Changes in joint configuration, joint valgus and fusion, with abnormal load distribution, loss of function and disability.
Ankle fracture: symptoms and first aid

Ankle fractures are one of the most common injuries to all bones and joints, especially in winter. Severe pain, inability to step on the foot, and numbness of the limb are symptoms that may prompt you to see a trauma surgeon.
Older people and people with ankle problems belong to the risk group.
The ankle joint is a complex anatomical structure that allows foot movement and walking. The ankle is the part of the leg that connects the lower leg and foot. The ankle joint is considered the most injury-prone area for the simple reason that it bears the greatest load, which is several times the body weight.

First-class care: what modern diapers can do
First aid and treatment for broken ankles
The first medical treatment for a broken ankle is to immobilize the limb with a splint. If the victim has an open wound, the bleeding must first be stopped. For minor bleeding, the wound should be disinfected and a sterile dressing applied, while for severe bleeding, a tourniquet should be applied.
Depending on the clinical picture and the complexity of the ankle fracture, appropriate therapy is carried out. For complex fractures with displacement, surgical reduction of the bone is performed. After repositioning, the wound is stitched and a plaster cast is applied to the fracture site. The duration of the plaster cast is on average 2 months. For fractures with displacement, the plaster cast can remain on the injured leg for up to 4-5 months.
The rehabilitation period after a broken ankle is as important as the treatment itself. Massages, exercise therapy and physiotherapy are prescribed so that the injured person can regain function as quickly as possible.
diagnosis and treatment
First aid
The first measure is to immobilize the injured limb and, if possible, immobilize the foot and lower leg. If the pain is severe, the patient can be treated with painkillers and taken to the hospital.
diagnosis
To make an accurate diagnosis, x-rays are taken in two projections (anterior and lateral). Additionally, a CT or MRI examination can be carried out.
Treatment
To close the fracture site, the surgeon puts it under local anesthesia. A plaster cast is then placed on the fracture site. If the dislocation cannot be reduced and the fused bones cannot be fixed with a plaster cast, an operation is performed.
During the operation, the individual bone fragments resulting from the fracture are fused together using special plates and fixation implants. The limb must then be completely immobilized (immobilized) to ensure effective bone fusion and prevent re-dislocation. Immobilization in a cast or bandage takes 1-3 months, depending on the complexity of the fracture. In parallel with surgical treatment, comprehensive rehabilitation is carried out until complete recovery.
Rehabilitation period.

Rehabilitation therapy includes:
Massages help to relieve muscle and ligament tension, eliminate congestion, and stimulate lymphatic flow and blood circulation. Physiotherapy treatments include magnetic therapy, electrophoresis and acupuncture. Therapy includes exercises to restore muscle tone and normalize the flexion and extension functions of the foot: circular rotations of the foot, right-left abduction, up-down abduction, etc.
Only the doctor can prescribe and combine different treatment methods, as the effect may vary depending on the type of fracture.
Specific symptoms
With an ankle fracture, the first symptoms appear immediately after the injury. The clinical picture is as follows:

- Intense pain in the area of injury that does not subside even when the leg is at rest.
- Inability to kick or move the injured leg and severe, increasing pain during these activities.
- Swelling and swelling around the lower leg joint.
- Deformation of the limb (with strong displacement), unnatural posture.
- Vitality of the skin at the fracture site, hematomas (consequence of bleeding due to the damaged ligaments).
- Crunching noises when palpating and moving the leg.
- Bleeding, painful shock, open wound with visible bone fragments in an open ankle fracture.
To assess a closed fracture, bilateral x-rays and, if necessary, computer tomography are carried out. If there is suspicion of vascular damage, angiography is indicated. This diagnosis makes it possible to obtain the most accurate picture in order to prescribe the correct treatment and not to confuse the fracture with an ordinary sprain or twist.
Rehabilitation after a displaced ankle fracture (after cast removal)
An ankle fracture is an injury to the tibia, fibula, or talus that compromises their integrity. In the event of a sprain, the ankle bone is usually affected. A posterior tear is the most serious form of ankle fracture.
It is often associated with fracture of the condyles of the tibia and fibula. This injury can also be accompanied by deep fractures of the tibia and fibula. If the ankle bone is also affected, this fracture often results in severe deformation of the bone heads, contributing to deforming osteoarthritis at a young age. Failure to perform rehabilitation after an ankle fracture can result in limping and severely limit physical activity.
Official medicine often does not begin full rehabilitation after an ankle fracture until the cast is removed, and this often has negative consequences. For severe combined fractures, the joint is immobilized for 4-6 weeks. During this time, the muscle fibers partially atrophy and the length of the ligaments and tendons shrinks dramatically. This eventually leads to the formation of a contracture. As a result, the affected person can no longer move their foot fully after the cast is removed because the ligaments are deformed.
Complete rehabilitation after a fractured ankle with dislocation must take place in several stages:
- After 10-12 days, you should start working on the muscles without involving the tendon apparatus;
- after 21 to 24 days, start working on the tendon apparatus;
- After 30 days, when the cast is removed, rehabilitation begins with physiotherapy, kinesitherapy, massage and osteopathy.
Rehabilitation can only be carried out under the supervision of an experienced doctor. It is important to note that the repaired break is a very delicate area. Various callus deformities can form, which can cause plantar fasciitis and heel spurs in the future.
How is the foot rebuilt after an ankle fracture?
Before the ankle is rebuilt after a fracture, an x-ray should be taken. If the examination shows that there are no fractures or permanently fused areas in the bone, a functional rehabilitation specialist should be consulted. This can be an orthopedist or a chiropractor.
Before breaking an ankle, the doctors in our chiropractic clinic carry out various functional tests and get a comprehensive picture of the condition of the muscles, fascia, ligaments, tendons and articular cartilage.
Comprehensive treatment of the ankle joint after a fracture includes the following areas of work for the practitioner
- Restoration of impaired blood and lymphatic circulation and microcirculation (when wearing a plaster cast or bandage, these processes are impaired);
- Restoration of normal innervation of all tissues of the foot, lower leg and ankle;
- If large nerves are trapped or compressed, the doctor will remove them using osteopathy;
- Activation of the regeneration process of all damaged tissues;
- Increasing the flexibility of the tendon and ligament apparatus (patients who neglect rehabilitation after an ankle fracture may incur a severe dislocation within the first three months if they accidentally twist their leg);
- Restoring the strength of trophic and muscle fibers;
- Prevention of deformation of all structural parts of the joint.
During the course of treatment, the doctor uses various rehabilitation techniques. Some patients also need dietary measures and reflexology to strengthen the general immune system, improve well-being and reduce excess weight. An ankle fracture or misalignment of the foot may be detected during the initial examination.
Types of Ankle Injuries
Below we will discuss the main types of ankle injuries that can occur in patients of different age groups. Each injury requires a specific first aid approach. Therefore, you should not attempt to diagnose and treat the injury yourself. If you have suffered a traumatic injury, you should see a trauma surgeon immediately. Only this specialist is able to make an accurate diagnosis, provide high-quality first aid and recommend initial treatment.
The following are the main types of ankle injuries:
- Fracture or breakage of the condyles of the tibia, femur;
- fracture or break of the talus or heel bone;
- Sprain and tear of the ligaments and tendons;
- Sprain, strain and tear of the joint capsule;
- Hematomas in the surrounding soft tissues;
- Subluxations and dislocations.
Each of these injuries has its own specific characteristics. Fractures and fractures almost always do not heal properly without professional help. A thickened bony callus forms, which puts pressure on the surrounding soft tissues. In this way, post-traumatic angiopathy and neuropathy can develop. In most cases, a cast is required to immobilize the injured limb for up to 40 days. Once the cast is removed, full rehabilitation at a chiropractic clinic is required.
Sprains and microscopic tears in ligaments and tendons are just as dangerous. It usually starts with a mild sprain of the foot. For example, you tripped or sprained your foot. A small tear occurs in a single fiber.
At this point, the exact same ligament or tendon tissue will not form again during the healing process without expert help. This is because tendons and ligaments do not have their own blood supply. They receive fluid and nutrients only through diffusion exchange with the surrounding muscles. But the muscles have to work constantly to achieve this.
Consequences and complications of ankle injuries
Without proper treatment, various complications arise after an ankle injury. Some of these lead to disability or severe mobility restrictions.
For example, an ankle contracture following an injury means a complete loss of mobility, making walking very difficult. But that is not all. When ankle contracture develops, the distribution of cushioning forces is disrupted. The knee and hip joints quickly deteriorate. Deforming gonarthroses and coxarthroses occur. Within 2-3 years, the lumbosacral spine also deteriorates.
Other likely consequences of an ankle injury include:
- Destruction of the small joints of the foot bones;
- Development of flat or club feet, which negatively affects the entire musculoskeletal system;
- Ankylosis of the joint with subsequent progression to complete or partial contracture;
- Deformative arthrosis of the ankle joint – thickened bony outgrowths form on the bone surfaces, making movement difficult and causing severe pain;
- Tear or complete disintegration of the ligaments and tendons;
- Hemarthrosis due to infiltration of blood into the joint capsule;
- Aseptic inflammatory necrosis of bone and cartilage.
All consequences of a traumatic impact can be easily avoided. First of all, all possible risk factors should be eliminated from your life. People who have one or more of the following risk factors are most likely to suffer ankle injuries
- Excessive body weight - the higher the weight, the more stress is placed on the tissues of this joint and the more likely a serious injury is if the foot slips or twists;
- sedentary lifestyle - due to the lack of regular exercise, the body's muscular skeleton becomes weak, undergoes dystrophic and atrophic degenerative processes and loses its ability to withstand increased mechanical stress;
- poor diet and inadequate intake of clean drinking water throughout the day;
- smoking and drinking alcoholic beverages;
- Hard physical work;
- inappropriate footwear for everyday life and sports;
- poor foot position in the form of a club foot or flat foot.
Nourishment
The recovery period should always be accompanied by adequate nutrition. During this time, the body needs more vitamins and nutrients, which should not only be supplied through food, but also through additional vitamin supplements.
During the period of active convalescence, it is necessary to saturate the diet:
- Protein (found in poultry, fish, meat);
- Calcium and silicon (can be obtained from cottage cheese, oatmeal, beetroot, cheese, parsley, sesame)
- Vitamins B, C and D (the largest amounts are found in fish oil, liver, bananas, beans and citrus fruits).
Alcohol, carbonated drinks, coffee, chocolate, fatty and salty foods should be avoided during recovery from a fracture.
massage
Therapeutic massage after a fracture includes specific techniques:
- Rubbing – active movements improve blood circulation and relieve pain;
- Kneading – restores muscle tone and improves tendon mobility;
- Stroking – light stroking movements relax muscles and improve microcirculation;
- Tapping – improves blood circulation and increases muscle contractility.
The therapist selects the course of treatment taking into account the specifics of the injury and the exact location of the fracture. Therapeutic massage can help prevent muscle loss and weakness, improve mobility, and relieve swelling and pain.
Read more:- Boots for a broken leg.
- The lateral ankle is.
- The hock in which the person is located.
- roll the dice.
- Photo: Outer malleolus fracture.
- The hock is the place where.
- Bones of the human ankle.
- The ankle bruise is where the picture is taken.
