If the child has a hemolytic disease, he or she should not be breastfed for several weeks. If there is no hemolytic disease, the mother can breastfeed after an injection of immunoglobulin. The drug is administered once and prevents the development of Rh-conflict in a subsequent pregnancy.

- What is a mosaic embryo?
- What is the incidence of mosaic embryos? PGT—A?
- Experience reports from the clinics
- Secret #2 The baby is developing evenly, but not necessarily 'perfectly' according to the manual.
- About development stages and new formation
- Secret #3 Mom's emotions are 'contagious
- Clubfoot in children
- How is clubfoot treated in children?
- Physical therapy for clubfoot
- Soft bandages
- Prevention of Rhesus intolerance
- Possible consequences of an immune conflict
- First pregnancy after turning 40
- Having a second child after 40.
- Fetal bradycardia: causes and symptoms
- Types of fetal bradycardia
- Two horror stories about motherhood. Marina Tsvetaeva and her mother Maria Main
- Komarovsky's advice
- prevention
What is a mosaic embryo?
Preimplantation genetic diagnosis of embryos for aneuploidy (PGT-A) is a genetic test designed to increase the success of IVF by obtaining information about the chromosomal health of the embryo.
Embryos with a normal set of 46 chromosomes (euploidy) have a better chance of implanting and developing a successful pregnancy than embryos with an abnormal set of chromosomes (aneuploidy). A healthy person has 46 chromosomes in their cells. We even have two pairs of each chromosome, one from our biological mother and one from our biological father.
PGT-A is performed because aneuploid embryos have a very high risk of implantation failure or abortion.
The likelihood of having an aneuploid embryo increases with age.
There are variants in which only one chromosome of a pair of chromosomes is present - the so-called 'monosomy'. Monosomy. Or vice versa, instead of 2 chromosomes there are 3, which is called Trisomy. During preimplantation genetic diagnosis, an embryo with chromosomal variants such as: aneuploid..
However, recent advances in PGT-A technology have revealed a third variant of PGT-A results that lies somewhere in the middle. This variant is called a mosaic embryo (it contains a combination of aneuploid and euploid cells). This is because DNA sequencing for PGT testing has become more advanced and sensitive. This improved technology is known as NGS (Next Generation Sequencing).
We are now able to see finer details, something that was previously impossible.
We can now hear '40% mosaicism', meaning 40% of cells are aneuploid and 60% are euploid (according to the biopsy).
- 20-40 % are low-grade mosaicism;
- 40-80% is high-grade mosaicism;
- > If there are more than 80 % aneuploid cells, the embryo is considered aneuploid.
What is the incidence of mosaic embryos? PGT—A?
Mosaicism occurs in approximately 15-90 % of embryos at the fetal stage and in 30-40 % of blastocysts (5-day embryonic stage) (Spinella et al. 2018), with the same frequency regardless of age (Munne et al. , 2017), namely in all embryos tested with PGT-A.
Apparently, euploid embryos have a greater chance of a successful pregnancy. The most common question patients ask after receiving their PGT-A result is 'How does this mosaic result affect the pregnancy or baby?'.
The answer is complicated. Although mosaic has always existed, it has only been detectable for a few years, so screening is not yet complete.
However, there are some guidelines and recommendations from the medical community.
Experience reports from the clinics

Our family is very grateful to Olga Loseva, a doctor at Embrylife Clinic. She is a very competent, knowledgeable and experienced specialist with a big and kind heart. Olga helped me and my husband have a child, even after two unsuccessful IVF attempts in another clinic. The doctor was inseparable from us throughout the entire procedure - she always gave us detailed advice and did her job well, supporting us with a kind word when we had difficulties. I sincerely believe this is the best possible treatment.

I recently underwent laser intimate rejuvenation at the Art-Eko clinic. I am very satisfied with the result! After giving birth, I had cracks, bulging walls, intimacy has not changed for the better, and incontinence, for example when coughing or sneezing. At 32 years old, I didn't want to put up with any of this anymore, especially if it could be fixed. It is a painless procedure and I have had it done three times so far. The results are fantastic! I have the sensitivity back and then some.

'But they have a very old and poor ultrasound machine.' I agree with you. While they look good, they can't do anything with their device, and if I have an urgent question I send them elsewhere. If they don't replace the device, they will lose customers.

The clinic is great. I'm a demanding patient (especially when you pay for it), but Ava Peter made everything convenient and easy for me. Like many others, I applied for IVF. I believe they did everything they could to achieve my pregnancy. Thank you for our long-awaited baby!
Secret #2 The baby is developing evenly, but not necessarily 'perfectly' according to the manual.
After a month, I learned to live with the new rhythm and began to read carefully about the baby's developmental stages. I studied it in psychology, but the theory required repetition and practice. For me, also as a psychologist, it was important that the baby corresponded to the 'norm'.
I read the chapters 'Baby development at N months - the norm' and read forums for mothers. There I received a lot of scattered information. One child started making sounds at the age of one, another was already playing chess. This scared me at first, but then I came to the most important conclusion: all children are different!
- Don't stick to the first table you find, find several and calculate the 'average temperature in the hospital';
- Read quality literature on child development - written by psychologists, published by faculty and academic institutions;
- be critical of the source 'the aunt said';
- Assume that all children are different.
Yes, we must not forget: There are no exact criteria.
The theory with which I began to follow child development was that of LS Vygotsky. He described the development of the child in terms of neoplasms, the zone of immediate development, crises and the leading type of activity. The periodization of child development according to DB Elkonin also helped me. It gave me a good starting point to track my child's developmental stages. After reviewing the proposed stages of development, it is important to review the most important thing - the formation of the new age.
If you want to know more about Vygotsky and Elkonin's theories, click on the hidden section below.
About development stages and new formation
Click on the title to read the text
A new formation is a new way in which a person interacts with reality that occurs at each successive stage of development.
Example. Yesterday your child reacted the same way to you and to the presence of another person in the room, but this morning he woke up and smiled only at you.
Secret #3 Mom's emotions are 'contagious
Every emotion I had quickly transferred to the baby. I had to control myself: the more upset I was (and I was, because sleepless nights and perfectionism kept me awake), the more upset the baby became. As a result he was grumpy and I was even more upset, it was a vicious cycle.
I needed to improve my relaxation skills. Meditation techniques are a great solution. The silent meditation from MR Ginzburg's book Ericksonian Hypnosis: A Systematic Course, for example, would be a good solution:
I have become calmer and so has the baby. The child calmed down more quickly, fell asleep more calmly and cried less. Learning to relax was difficult, but it was all a matter of willingness and practice.
- Make friends with your feelings instead of suppressing them: if it's bad, go into another room for five minutes and breathe; if it is very bad, leave your husband alone with the baby and go for a walk;
- Learn meditation techniques: Simply lie down and imagine yourself in a pleasant place - by the sea, in a forest by a babbling river;
- rest, rest and rest.
Clubfoot in children
Treatment of the condition depends on the severity of the clubfoot. Only then will the professionals select the best treatment method. Treatment is carried out by a doctor, and parents must strictly adhere to all recommendations. There are cases where treatment can last up to several years.
There are three degrees of clubfoot in children.
- Minor – the feet are slightly deformed. The ankles are movable.
- Moderate – there is foot deformity and limited ankle mobility.
- Severe – there is severe foot deformity and complete lack of ankle mobility.

If clubfoot is detected in an infant, parents immediately contact an orthopedist and begin treatment. However, sometimes the abnormality is discovered later because adults do not know how serious the condition is and believe it will go away. If clubfoot is not treated in children up to a year old, it will only become more complicated later. After all, some muscles are over-tightened and others are under-tightened. That can have consequences.
- X-shaped curvature of the legs.
- curvature of the spine.
- Sleep disorders.
- Headache.
- Habit of placing feet poorly.
- Physical and mental development is delayed.
How is clubfoot treated in children?
In the case of congenital defects, the orthopedist begins treatment immediately. Parents take an active part in the treatment. Your task is to observe how the child walks, prevent clubfoot, control the alignment process of the feet and legs and choose special orthopedic shoes for the child. For a mild form, massages and gymnastics are recommended. In addition, diseases that promote clubfoot are corrected. These include adduction (movement of the foot towards the center of the torso), supination (movement of the foot outwards), equinus (walking on tiptoes like a ballerina, with the foot held in place by soft bandages).
If the degree is moderate, the clubfoot is also corrected. The gait is then corrected with plaster casts. Here too, the process of turning the toes downward is emphasized.
If all methods fail to eliminate the clubfoot, the child will have severe clubfoot. In this case, surgery is recommended. In small children the ligaments and tendons are operated on, in older children the joints and bones are operated on. A very severe degree is almost rare. It is treated by a combination of all methods. In addition, orthopedic shoes are prescribed. This also applies to the prevention of the disease. According to statistics, children who wear special shoes can avoid clubfoot even if many factors are present.

Physical therapy for clubfoot
Exercise is very effective, but should be done with a child who is only a few months old. During this time, the muscles and ligaments are still developing well. Therefore, exercises should be performed that include raising the legs, bending the legs around the feet, simultaneous and alternating flexion of the legs, circular foot movements, and walking with support.
Soft bandages
If a mild degree is observed, the use of soft bandages is effective. The doctor first performs corrective exercises and then places a soft bandage around the entire limb. The bandage should be applied consistently and in a specific position.
Prevention of Rhesus intolerance
All Rhesus-negative pregnant women without antibodies are recommended to undergo pregnancy in the 28th to 30th week. This drug is able to bind D-antigens that have entered the woman's bloodstream, thereby preventing an immune reaction.
Women who have undergone immunoglobulin therapy no longer need to be tested for antibodies in the following months of pregnancy: after the injection, a small amount of antibodies will be present in the blood, which is completely normal.
The immunoglobulin injection is not only given in the 28th to 30th week of pregnancy. It must also be given within three days of:
After the baby is born, umbilical cord blood is collected for analysis and sent to a diagnostic laboratory to determine the baby's Rh value. The test results are usually available after 24 hours. If the baby has Rhesus, there is no risk and the woman does not need to be injected. If the baby is Rh+, the woman must receive an injection of immunoglobulin to rule out an immune reaction in future pregnancies.
Immunoglobulin is only made available to hospitals in limited quantities and may not be available to all women who have recently given birth.
Another indication for immunoglobulin is bleeding during pregnancy. A pregnant woman with Rhesus factor must be very careful with her body. If even minor bleeding or vaginal discharge occurs, you should receive an immunoglobulin shot as soon as possible to prevent antibodies from forming against the fetus. Remember, you only have 72 hours to give the injection! During this time you will need to be tested for antibodies as the immunoglobulin injection is only given if there are no antibodies present.
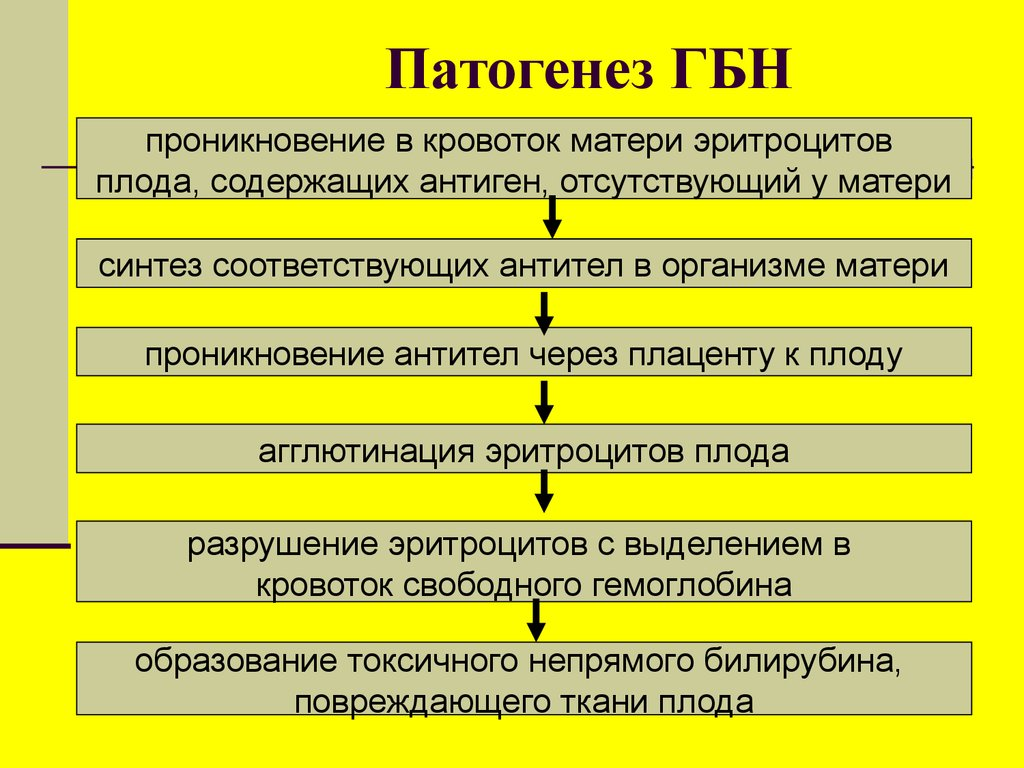
Possible consequences of an immune conflict
The maternal antibodies in the fetus' bloodstream destroy its red blood cells. As a result, a hemolytic disease develops in the fetus and newborn, leading to anemia, poisoning and various organ disorders.
The edematous variant of hemolytic disease can be diagnosed during pregnancy by ultrasound examination of the fetus. During the ultrasound examination, the following is determined
- a swelling of the placenta;
- Traumatic hemoptysis;
- Accumulation of effusions in the abdominal cavity, pleural cavity;
- Hypertrophy of the liver, spleen, heart muscle, thickening of the intestinal walls;
- 'Buddha position' - The fetus' abdomen is enlarged and the legs are spread.
The jaundice variant of hemolytic disease shows clinical signs at birth:
- A blood test reveals a high level of intermediate bilirubin;
- The baby's skin becomes yellowish;
- The newborn may have an enlarged spleen, liver, heart and lymph nodes.
First pregnancy after turning 40
In fact, the first pregnancy at 40 is not much different from the first pregnancy at 20: the same risks, the same characteristics, the same consumption of maternal resources.
But the resources of women in their 20s and 40s will be different.
Although every body is different, there are a number of problems that most women encounter in late pregnancy.
The main problem of late pregnancy – is the lower probability of fathering a child. Between the ages of 40 and 45, the ovarian follicular reserve begins to deplete, and the ovaries themselves begin to respond less to hormones. Studies show that changes in the reproductive system can begin long before menopause, as early as age 35. Blood supply to the reproductive organs decreases and the lining of the uterus deteriorates. The illnesses she has suffered from throughout her life and the medications she has taken also affect her fertility. Of course, the list at twenty is much shorter than at forty.
However, it should be borne in mind that the statistics show the average situation, so many women still have high fertility even in their forties. In addition, modern medicine is able to solve many of the above-mentioned problems and increase the likelihood of conception.
The second problem. – The risk of developing genetic diseases in the future child. The older a woman is, the more likely she is to give birth to a child with Down syndrome and other genetic abnormalities.
The third problem – are chronic and latent diseases, exhaustion of resources. Pregnancy at any age is torture for the body, it consumes a significant amount of energy, is associated with physical exertion and involves a restructuring of the entire body. The worse a woman's health, the more difficult it will be for her to bear a child. Bone and joint diseases, circulatory disorders (e.g. high blood pressure), hormonal disorders, hidden diseases, untreated inflammation - all of this makes pregnancy and birth more difficult. However, not all women can boast of perfect health at the age of forty. In order to afford to give birth to a healthy child after 40, a woman needs to take care of her health and get herself in good shape.
Having a second child after 40.
Many women make the decision to have a second child after the age of 40. This is usually a psychologically conscious decision so that tests can be ordered earlier, illnesses can be treated if they are discovered, risks can be discussed with the doctor, and preparations for pregnancy can begin earlier. It is assumed that if there were no complications in the first birth, the second birth can also be easier. However, the truth is that everything depends on the condition of the woman's body and her genetic characteristics.
The risk of losing a child exists with every pregnancy, but the number of negative factors increases with age. And acquired chronic diseases influence this to a large extent. Diabetes, hypertension, endocrine disorders and undetected chronic diseases of the reproductive system can lead to miscarriage, premature birth or frozen pregnancies.
Another risk that is directly related to age is hereditary diseases in children. The older a woman is, the greater the likelihood. A not insignificant part of the problem of hereditary diseases are 'hidden risks' - constant electromagnetic radiation, polluted air, smoking (including passive smoking), inhalation of exhaust gases, contact with pesticides. All of these factors lead to an excess of free radicals (oxidative stress), which can damage the genetic makeup of men and women. But while the genetic material in the man's sperm is completely renewed after three months, the woman's egg cell reserve is deposited at birth. However, free radicals are especially dangerous for the maturing egg, since it is she who will give birth to a new life. According to experts, the greatest risk of pregnancy after the age of 40 is the possibility of genetic diseases in the child. Therefore, pregnant women over 40 are strongly recommended to undergo all necessary preventive examinations to detect fetal anomalies in advance.
Fetal bradycardia: causes and symptoms

Not every drop in a person's heart rate is an abnormality or pathology. For example, it occurs during sleep or when the ambient temperature drops - at such times the body saves energy and slows down the metabolism. It also occurs in athletes or is present from birth in some people, but is not pathological. In such cases one speaks of physiological bradycardia. The main difference from abnormal bradycardia is that it does not have pathological symptoms.
Abnormal bradycardia is a drop in heart rate that causes various painful symptoms such as dizziness, cold sweats, fainting, etc. These usually occur when the heart rate decreases significantly. If it is not significant, the person may not feel it.
To assess whether fetal cardiac bradycardia is present, it is necessary to know the physiological heart rate norm. In an adult it is 60-80 beats per minute, but in an embryo it changes during development:
- In 3-5 weeks – 75-80;
- In week 5-6 – 80-100;
- In the 6-7th week – 100-120;
- In weeks 7-9 – 140-190;
- In weeks 10-12 – 160-180;
- In the 4th month – 140-160;
- In the 9th month there are already 130-140.
The values given are not exact, since the physiological norm for each baby may vary slightly. Until about the 21st day of pregnancy, the embryo's heartbeat is not audible at all - at this point, its own heart has not yet formed and the metabolism is completely supplied by the mother's bloodstream.
Abnormal bradycardia in the mother and fetus can only be clearly diagnosed in the second trimester (after the 20th week of pregnancy), as at this point the body's own circulatory system has essentially already developed and the heart rate should therefore stabilize. The doctor will make the diagnosis if the heart rate is below 110-120 beats per minute during this period.
Types of fetal bradycardia

Depending on the nature and intensity of the decrease in the fetal heart rate, the following types of pathology are distinguished:
- basal – diagnosed when the fetal heart rate falls below 120 beats per minute; if the fetus is treated quickly, harm to the baby and the mother herself can be avoided;
- Slowed down. - Bradycardia, when the fetal heart rate is less than 72 beats per minute; the woman should be hospitalized and remain in bed;
- Sine - Sine. If the fetal heart rate drops to 70-90 beats per minute, this is the most dangerous condition and the woman needs urgent hospitalization and intensive care until delivery.
It is important to determine the exact nature and cause of bradycardia because this determines how high the risk is to the baby and mother and what therapeutic strategy should be chosen to treat the condition or at least reduce the risk.
Two horror stories about motherhood. Marina Tsvetaeva and her mother Maria Main

Marina Tsvetaeva's eldest daughter, Ariadne Ephron, survived only because her mother carried her out of the orphanage wrapped in a fur coat. The younger Irina was left in an orphanage - and soon starved to death. Her youngest son George Efron, or Mura as Tsvetaeva called him, tried to love her almost hysterically after her daughter's terrible death. Tsvetaeva indeed had a very difficult character. She was heavily influenced by her mother, Maria Main. At the age of 23, My Tsvetaeva's father, who was 44 years old, married. He had two daughters from a previous marriage. His wife died, but he loved her madly - her portrait hung in the living room of the Tsvetaeva family, and the girls did not accept their new stepmother. Maria Maine was in love with another man, but her father came between them - and she chose her father. She was an extremely principled and tough woman. – Because my mother, a musician, wanted me to be like her. Because people thought (for six years!) that I wrote badly - 'even Pushkin wrote in free verse, but she has no greatness!'
. Round table. A family circle. Sunday cookies from Bartels are on the blue serving plate. One for each.
- Children! Take her! – I want a meringue and I want an eclair. Embarrassed by my mother's clear gaze, I lower my gaze and drop it completely:
'Fly, my swift horse!
Over seas and meadows,
And shake your mane,
Take me there!
- Where to? – They laugh: my mother (triumphantly: I'm not going to be a poet!), my father (good-natured), my brother's tutor, a student from the Urals (go-go-go!), my older brother (following the tutor) and my younger sister (following my mother) have been laughing for two years; only my older sister, Valeria, a seventeen-year-old student, doesn't laugh, despite my stepmother (my mother).
And I, red as a peony, dazed and blinded by the blood that has flowed to my temples, by the tears that boil and have not yet overflowed, I am at first silent, then I scream: - There - far away! There, there!!! And I'm very ashamed to steal a notebook and then laugh!' (story about the dedication), This is how Tsvetaeva described a scene from her childhood. It seemed to Marina that her mother should hate her because she was her father's daughter, and not the beloved husband of Maria Maine. Marina Tsvetaeva grew up self-centered and self-absorbed precisely because of the atmosphere in her house. She was ridiculed in front of strangers and given no paper to write her poems on. Her mother was uncompromising and did not respond to her children's wishes.
 In a letter to Vera Bunina, Tsvetaeva writes about things that make even the most blind suspect the narcissistic nature of the great poet. She talks about longing for freedom but not being able to leave her husband and daughter at the same time. – I, Vera, have had a reputation for being tough all my life, but all my life I haven't left her [husband and daughter - MT], even though sometimes HOW much I wanted to! A different life, myself, the freedom, the fullness of myself, myself out there, just a blissful morning with no obligations. The year 1924, no, I'm lying - 1923! Crazy love, the strongest in my entire life - ringing, tearing, but remaining CONVENTIONAL: for - S. - and Alya, her, the family - as without me! – 'You can't be happy on someone else's bones'. – was my last word. Vera, I'm not sorry. It was me. I couldn't have it any other way. (I read Anna Karenina for 14 years because I knew I would never leave Seryozha. I fell in love with Vronsky and stayed with Seryozha. Because not loving is impossible, and I HAD to know that, especially about myself myself. But the family in my life was such a certainty that I simply and never put it at risk. And taking Alicia and living with someone else - that was also such a scandal for me that I couldn't shake hands with anyone who suggested this to me.
In a letter to Vera Bunina, Tsvetaeva writes about things that make even the most blind suspect the narcissistic nature of the great poet. She talks about longing for freedom but not being able to leave her husband and daughter at the same time. – I, Vera, have had a reputation for being tough all my life, but all my life I haven't left her [husband and daughter - MT], even though sometimes HOW much I wanted to! A different life, myself, the freedom, the fullness of myself, myself out there, just a blissful morning with no obligations. The year 1924, no, I'm lying - 1923! Crazy love, the strongest in my entire life - ringing, tearing, but remaining CONVENTIONAL: for - S. - and Alya, her, the family - as without me! – 'You can't be happy on someone else's bones'. – was my last word. Vera, I'm not sorry. It was me. I couldn't have it any other way. (I read Anna Karenina for 14 years because I knew I would never leave Seryozha. I fell in love with Vronsky and stayed with Seryozha. Because not loving is impossible, and I HAD to know that, especially about myself myself. But the family in my life was such a certainty that I simply and never put it at risk. And taking Alicia and living with someone else - that was also such a scandal for me that I couldn't shake hands with anyone who suggested this to me.
I'm telling you this so you can see how kind Alia was to me – wrote Tsvetaeva. Tsvetaeva viewed her adult daughter Asia as sleazy and incapable of living independently and apart from her parents. However, there were no clear reasons for this. At the age of 20, Ariadne was already a complex, intelligent and bright girl. This rigid upbringing, rule-following and uncompromising attitude certainly left its mark on Tsvetaeva's psyche, who eventually took her own life. However, the situation she found herself in at the time was truly horrific. No one in exile wanted to hire her, and she herself had nothing to eat. Irina's death was a terrible tragedy, but even then the poet lived in poverty. There was no money and hunger forced her to give her children to an orphanage because she was told they would get food there. Her husband was at the front. Maybe from today's perspective and worldview we simply have no moral right to condemn them.
This rigid upbringing, rule-following and uncompromising attitude certainly left its mark on Tsvetaeva's psyche, who eventually took her own life. However, the situation she found herself in at the time was truly horrific. No one in exile wanted to hire her, and she herself had nothing to eat. Irina's death was a terrible tragedy, but even then the poet lived in poverty. There was no money and hunger forced her to give her children to an orphanage because she was told they would get food there. Her husband was at the front. Maybe from today's perspective and worldview we simply have no moral right to condemn them.
Komarovsky's advice

Dr. Komarovsky draws the attention of parents to the fact that clubfoot cannot be eliminated without special treatment measures.
Curing the neglected form of this disease is much more difficult than pathology detected at an early stage.
In addition to the treatments carried out in medical institutions, it is necessary that Additional home therapy for your child. Even those who have never used these techniques will have no difficulty learning basic massage or remedial gymnastics.
From the statement of Dr. Komarovsky, the following conclusions can be drawn:
- Clubfoot always needs to be treated;
- The disease can lead to disability of the child and significantly affect his quality of life;
- Children diagnosed with clubfoot should only wear orthopedic shoes;
- It is recommended that the child be barefoot at home;
- Massage is only an effective treatment in mild to moderate stages of clubfoot;
- If clubfoot is caused by a bone disease, self-medication should be avoided.
prevention
Preventive measures to prevent the appearance of clubfoot in a child should be carried out During the prenatal period.
Women are advised to completely give up unhealthy habits, eat a healthy diet and have their fetus examined regularly by the health service.
If no clubfoot symptoms are detected in the newborn, the acquired disease should be prevented in the first few years of life.
preventive measures. These include the following recommendations:
- Observe the child's gait and, if any abnormalities are suspected, seek medical attention early;
- The child's footwear should be of good quality and comfortable;
- The child's diet should contain foods containing calcium;
- Prevent your child from becoming overweight;
- Ensuring the child gets enough exercise;
- Massage the feet with special mats, walk on sand or pebbles.
It is possible to confirm the diagnosis of acquired clubfoot in a child before seeing a doctor. The child should take a few steps on wet sand.
The foot pathology will be clearly visible in the footprints. If a child is diagnosed with congenital clubfoot almost immediately after birth, the treatment process should be started as early as possible.
Can club foot nevus in newborns be treated? Find out in our article.
How to correct clubfoot in a child? About the treatment of congenital clubfoot for children, see this video:
Please do not self-medicate. Make an appointment with your doctor!
Read more:- How do you know which leg is pushing?.
- Causes of tiptoe walking in babies.
- A child begins to have clubfoot between the ages of 1 and 5.
- Insoles for pregnant women.
- How a child's feet grow at the age of one.
- Why does a child develop clubfoot?.
- Child with Komarovsky clubfoot.
- Clubfoot in children therapeutic exercises 7 years old.
