Studies have shown that MRI or CT scanning is more effective for indeterminate PLA. Both techniques can detect fractures, but MRI, in addition to PLC, showed significant changes in the carpal ligament (Bäcker, 2020; Parvizi, 1998; Clementson, 2020).

- Fractures of the foot bones
- species
- Causes of heel bone fractures
- Symptoms of a metacarpal fracture
- Diagnosis of a heel bone fracture
- Treatment of a fractured heel bone
- surgical treatment
- Modern minimally invasive surgical procedures
- How can I recognize this?
- Treatment of a fracture of the navicular bone of the foot
- Result indicators.
- Subjective evaluation
- Treatment
- surgical treatment
- Conservative treatment
- Causes of navicular fractures:
- GRIGORENKO Andrei Alexeyevich
- Tereshkin Vitaly Tereshkin
- Diagnosis of navicular fractures:
- causes
- signs
- prophylaxis
- rehabilitation
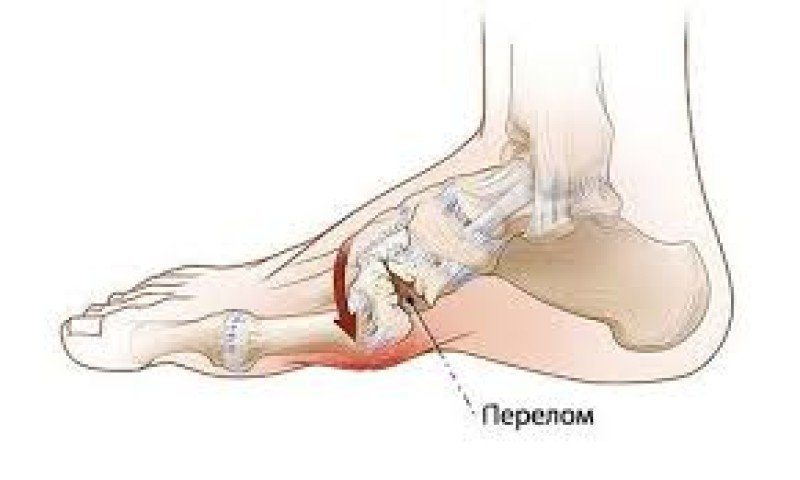
Fractures of the foot bones
A foot bone fracture is a condition characterized by a disruption in the integrity of one or more of the bones that make up the human foot. This injury is common and accounts for one tenth of all fractures.
The causes of disruption of the foot anatomy can be divided into two groups - direct and indirect forces, where the following factors may also be added
- foot compression from tight footwear;
- crushing the foot with a heavy object or a sharp blow to the foot;
- rolling up the foot;
- Improper landing after a fall or jump;
- injuries at home;
- crushing of the toes (e.g. if someone steps on your foot with full force);
- disasters (fall from a bicycle, car accident, unsuccessful parachute jump, etc.);
- Bone diseases that cause the breakdown of bone structure and reduce bone strength;
- bone tumors.
species
The following types of this disease are distinguished:
- open;
- closed;
- solitary;
- multiple;
- with or without displacement of bone fragments;
- dislocations of fractures.
Depending on the localization, fractures of these bones are distinguished:
Regardless of the type of lesion, the consequences should not be underestimated, since the foot is the support for the whole body and any anomaly can lead to disorders - the development of flat feet or secondary arthritis.
Causes of heel bone fractures
Fractures of the ankle jointAnkle fractures are most commonly caused by a fall with an outstretched hand. A fall from the same position often results in a fracture of the distal radius bone. Fractures of the scaphoid occur in people of all ages, including children. The injury often occurs in sports or traffic accidents. Men between the ages of 20 and 30 are at higher risk of breaking the heel bone of the hand for one reason or another.
Some studies have shown that wearing protective devices while inline skating, snowboarding, skiing, and skating reduces the likelihood of wrist and radius fractures.
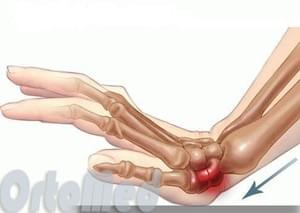
Symptoms of a metacarpal fracture
- Pain and swelling in the 'anatomical snuffbox' area at the base of the thumb. The pain can be very severe when moving, feeling or trying to grasp something;
- Restricted movement of the hand, but this can be masked by the pain and it is very difficult to determine on examination how much movement there is;
- Crepitus of fragments (crunching of broken bone fragments);
- Bleeding in the wrist area.
If the wrist is not deformed (as in displaced fractures of the radius), this does not mean that the smaller bones of the wrist are not broken. In some cases, the pain is not very severe and can be confused with a bruise, an injury to the ligaments.
Wrist pain that does not go away within 24 hours of the injury may be a sign of a fracture.
Diagnosis of a heel bone fracture
The anamnestic examination indicates a corresponding injury.
Examination reveals swelling on the radial side of the joint in the area of the anatomical snuffbox. Pain on palpation and dorsiflexion of the hand is also noted here. Axial loading of the first finger causes pain in the scaphoid area. Movement of the wrist is restricted and painful, particularly during radial and dorsiflexion of the hand.
Laboratory and instrumental studies
If a fracture of the navicular bone is suspected, x-rays should be taken in two, or better, three projections: straight, lateral and in semi-profile. In some cases with a clear clinical picture, the fracture is not visible on the radiographs, even with the help of a magnifying glass. In these cases, the same procedure should be used as for a fracture of the navicular bone. A plaster cast should be applied for 10-14 days, after which the plaster should be removed and the x-ray repeated. During this time, the bone becomes overheated and the gap between the fractures increases and becomes visible on x-rays.
[1], [2], [3]
Treatment of a fractured heel bone
Conservative treatment of heel bone fractures
Treatment is usually conservative. After injecting 10-15 ml of 1%iger procaine solution into the fracture area, the fractures are approximated by palmar traction, palmar flexion and ulnar retraction. Pressure on the bony fragments in the area of the 'anatomical snuffbox' completes the reduction. A circular plaster cast is applied from the elbow joint to the metatarsophalangeal joints of the toes in a functionally favorable hand position (wrist position with tennis ball).
After 3-5 days, UHF, static muscle contraction under the cast, LFC and stimulating physiotherapy on symmetrical parts of the healthy limb are recommended. After 2.5-3 months the cast is removed and an X-ray examination is carried out. If consolidation does not occur, immobilization continues for up to 4-6 months. Once immobilization is completed, rehabilitation treatment is prescribed.
Surgical treatment of heel bone fracture
If closed reduction is not possible in the hospital and the joint fractures are not displaced or false, surgical treatment is indicated. The operation consists of open reduction and fusion of the fracture. An autologous bone nail is considered optimal fixation, even better when placed on a supplying vascular nail. Another microsurgical procedure is connecting the supply vessels to the damaged bone, which also achieves good results. In some cases with nonunion or even aseptic necrosis of the scaphoid with deforming osteoarthritis, the function of the wrist is preserved and there is little or no pain. Surgical treatment should be avoided in these patients. However, if impaired joint function and severe pain are noted, scaphoid arthroplasty is performed. Arthrodesis of the wrist is rarely indicated.
surgical treatment
If the scaphoid is fractured at the ligament or proximal pole, or if the fragments are displaced, the doctor may recommend surgical treatment. The aim of the operation is to restore the correct position and stabilize the fracture in order to create optimal conditions for the fracture to heal.
Repositioning. During the operation under anesthesia, the doctor tries to put the fragments back into the correct position. In some cases, a small incision or special instruments are used. In other cases, full access is created and the fragments are reduced under eye control. The fragments can also be repositioned using a small video camera, the arthroscope.
Internal fixation. Metal structures such as screws and/or spokes are used to fix the fragments in the correct position until they are completely healed.

(From the left) The x-ray shows a fracture of the scaphoid fixed with a screw. (From the right) This x-ray was taken 4 months after surgery. The fracture is completely consolidated.
The location and size of the access depends on the location of the navicular fracture. Sometimes a small incision is enough to insert a screw or needle. In other cases, full access is required to ensure adequate reduction of the fracture. The incision can be made on the dorsal or palmar aspect of the wrist.
Modern minimally invasive surgical procedures
For certain types of fractures, we use very small incisions (less than 1.0 cm) to reduce the fracture and fix it in the correct position with a screw. This procedure is carried out under constant radiological control.
In addition, the doctor can insert a small camera, called an arthroscope, into the joint and visualize the fracture on a monitor. This method helps to control the repositioning and fixation of the fracture and reduce surgical trauma.
Various variants of bone grafts and bone replacement materials that stimulate bone regeneration are currently being researched. Bone morphogenetic proteins that are involved in normal bone remodeling processes are also being researched.
Bone grafting. In some cases, bone grafting may be indicated in combination with or without internal fixation. Bone grafting involves inserting healthy bone tissue into the fracture site. This stimulates bone regeneration and fracture healing. A radial bone from the same forearm or thigh can be used to harvest the bone material.
Regardless of which treatment you choose, you may be advised to wear a splint or cast for up to six months or until the fracture heals. Unlike most other fractures, navicular bone fractures heal slowly. The following activities should be avoided throughout the treatment period (unless approved by your doctor):
- Lifting, carrying and other manipulations with weights over 0.5 kg
- Throwing/throwing objects with this hand
- Practicing contact sports
- Climbing trees
- Activities that involve the risk of falling on the wrist, e.g. B. Ice skating or diving
- Working with heavy or vibrating tools
- Smoking (can delay or prevent healing of the fracture)
How can I recognize this?

When a patient complains of pain and the first signs of injury are detected, the doctor takes a medical history, conducts an examination and orders an X-ray. In complicated cases, further examinations are carried out:
It is difficult to diagnose a fracture without displacement because the symptoms are mild. Comparative projections and dynamic scans are required. The accessory bone resembles a burst fracture and the dorsal separation is identical to a surface injury to the ankle joint. To diagnose Keller's disease, a medical history and x-rays are examined.
Treatment of a fracture of the navicular bone of the foot
The choice of treatment depends on the severity of the injury. If there is a closed fracture without displacement, a circular cast is applied and the arch of the foot is simulated. A supination splint is used prophylactically to flatten the foot. In the case of a fracture with displacement, an initial repositioning is carried out after anesthesia.

If a displaced fracture is present, a Cherkes-Zade design, which resembles metal spokes, is used. In this case, one spoke is pulled through the heel bone and the other through the metatarsal head. The operation is performed under general anesthesia. The foot is covered with a plaster cast for 6-10 weeks. After this time, the cast should be checked regularly with x-rays.
The scaphoid bone is rarely removed because such an operation leads to deformity of the foot.
Doctors recommend the following measures to restore foot function:
- Physical therapy;
- massage treatments;
- sea salt baths;
- regular swimming;
- Use of orthopedic shoes.
Treatment of Keller's disease includes wearing a plaster cast for 1.5 months, after which the patient should limit physical activities and active movements. The patient should be provided with appropriate orthopedic footwear. In parallel, physiotherapeutic treatments such as vascular electrophoresis, ultrasound and others are carried out.
Result indicators.
- DASH or QuickDASH (hand, shoulder or arm disability).
- A 15-item PRWE questionnaire (Mc Dermid, 1998) was developed to assess wrist pain and disability.
- The PEM (Patient Evaluation Questionnaire) has a simple layout with questions asked in a visual analog form. Patients are asked to read and understand only the question, and not the description of each interval response (Scott, 2019).
Subjective evaluation
When examining a patient with suspected SPS, it is important to compare the injured wrist with a healthy wrist.
- The pain of the navicular tuberosity on examination is 90 % a highly sensitive symptom of PPC, but only 40 % is nonspecific (Gutierrez, 1996).
- Navicular tuberosity: The clinician extends the patient's wrist with one hand and applies pressure to the tuberosity in the proximal wrist crease with the other hand. This provides better diagnostic information; Sensitivity 87 %, specificity 57 % (Gutierrez, 1996).
- Pain on the scaphoid compression test (ie, axial/longitudinal compression of the patient's thumb along the first metacarpal line) has been shown to help identify PPC (Greene, 2001; T. Grant Phillips, 2004).
- Runny nose pain with wrist pronation followed by ulnar deviation (52 % positive predictive value, 100 % negative predictive value) (T. Grant Phillips, 2004).
Treatment
If a fracture is suspected with an adequate clinical picture on examination but negative radiographs, a follow-up examination with repeat radiographs should be performed after 7-14 days. If pain persists and x-rays are normal, further imaging with MRI or CT should be performed. Pain management with medication should be considered.
surgical treatment
Indications for surgical treatment include:
- Displacement of more than 1 mm.
- Intraradial angle greater than 35 degrees (humpback deformity).
- Angle between the radius bone and the half bone greater than 15 degrees.
- Translateal-perilunate dislocation.
- Fractures of the proximal pole.
- Fragmentary fractures.
- Hip fractures without dislocation in people who need to return to work/sports quickly.
- Fractures without dislocation or avascular necrosis.
Surgical fixation involves the insertion of one or more screws and can be performed percutaneously or openly. The latter method is preferred for non-fused and highly displaced fractures, while the former is preferable for acute fractures with minimal displacement (Hayat, 2020).
Conservative treatment
Fractures without displacement and within the distal third of the bone can be treated non-surgically with immobilization in plaster. There is debate as to whether a long or short shoulder cast is preferable and whether a thumb splint should be applied. There is currently no evidence that one option is better than the other.
Immobilization for 6 weeks with repeat radiographs to evaluate the anastomosis is usually required.
The healing time depends on the location of the fracture.
- In approximately 90 % of fractures with no or minimal displacement (≤0.5 mm) of the navicular talus, the distal third heals within 6-8 weeks, the middle third within 8-12 weeks, and the proximal third within a few weeks.
- Hip fractures of the navicular bone with moderate displacement (0.5-1.5 mm) can be treated conservatively but require long-term immobilization in plaster for 8-10 weeks (Clementson, 2020).
Causes of navicular fractures:
- Pain and swelling in the 'anatomical snuffbox' area.
- increased pain on movement or palpation
- Restriction of movement in the wrist
- Crunch of broken bone fragments
- Bleeding in the wrist area
- Wrist pain that lasts up to 24 hours
GRIGORENKO
Andrei Alexeyevich
25 years of experience Founder and head of the clinic.
Neurologist, Doctor of Osteopathy Europe (DOE), rehabilitator, orthopedist. Schedule an appointment
Tereshkin
Vitaly Tereshkin
Over 20 years of experience as an osteopath, chiropractor and rehabilitation therapist.
Specialist in restorative medicine, negative pressure gradient therapy, medical stretching and therapeutic exercises. Schedule an appointment
Diagnosis of navicular fractures:
- X-rays of the injured limb help identify the type of fracture of the navicular bone.
- CT scans help to visualize the displacement of the fragment in complex injuries to the articular surface.
- MRI is used to visualize possible damage to the capsule and ligaments of the foot.
- Fractures near the distal pole. Both fractures have sufficient blood supply and heal reliably and quickly, regardless of whether the wrist is immobilized. However, a plaster cast for 2-3 weeks is still recommended.
- Fractures of the calcaneal shaft. As a rule, both fragments have sufficient blood supply. Fracture healing is only possible if the joint is completely immobilized in a plaster cast. In a recent fracture, fusion usually occurs after 8-10 weeks, but immobilization must be continued until radiological confirmation of complete fusion.
- Proximal pole fractures. Every fracture has sufficient blood supply, and if the carpal joint is completely immobilized, regrowth usually occurs after 6-8 weeks. In 1/3 of proximal pole fractures, the blood supply to the small fracture is impaired. Recovery is then very slow and sometimes immobilization must be continued for up to 12 months or even longer.
- With conservative methods, treatment requires immobilization (casting) of the wrist and first finger for 2 weeks or longer while the fracture heals.
- Surgical methods are used when the fracture cannot be healed with conservative treatment. Elimination of displacement of bone fragments and their fixation with an implant (screw) for stabilization.
- Relief of pain in the area of the fracture
- Improving blood circulation in the wrist and carpus
- Restoration of metabolism in the damaged tissues of the hand
- Restoration of the physiological function of the damaged upper extremity
- Work on the damaged wrist
- Restoration of active movement of the hand
causes
- Direct trauma. A fall with a heavy object on the foot. This type of injury rarely only results in a fracture of the navicular bone; as a rule, the cuboid and sphenoid bones are affected;
- Indirect trauma. This type of fracture occurs when the foot is forcibly and violently flexed in the area of the instep, resulting in severe entrapment of the scaphoid bone between the talar head and parts of the sphenoid bone. There are two types of fractures that occur with such mechanical pressure: in one case, a small bone rim on the dorsal surface is detached from the navicular bone, in the other case, the bone in the tuberosum on the mandibular surface is detached;
- FRACTURE. The fracture is the result of compression of the foot bone;
- stress fractures. This type of bone injury occurs in competitive athletes, most commonly gymnasts and ballet dancers. With intense physical activity over a long period of time, a pathological process of restructuring of the bone structure occurs, which can last 1-1.5 years. In recent years, an increase in this bone pathology has been observed in athletes participating in competitive sports such as football and basketball. Stress fractures can also be caused by early loading of the foot after treatment.
If the navicular bone fractures, the fragments often shift in the plane and in the axis, e.g. B. to a displacement of the fragment backwards or backwards and inwards.
In competitive athletes who participate in athletics, a fragment may be torn near the navicular tuberosity, where the tibialis muscle attaches. This injury occurs in conjunction with an uncoordinated, violent contraction of the tibia.
signs
- When examining the foot, the injured person notices swelling and pain in the area of the injured bone;
- Limited soft tissue swelling may be observed over the segment of injured bone;
- In some cases, the swelling may extend to the ankle;
- If a segment of the scaphoid has been displaced into the back of the foot due to the fracture, a bone protrusion can be felt in the area of the swelling;
- The injured person is unable to walk fully or support himself on the injured leg. In this case, the patient can only step on the heel;
- The patient is unable to make active movements of the foot up and down or to the right and left at the doctor's request;
- Any axial load in the area of metatarsals I, II and III causes severe pain in the foot, which spreads to the heel bone;
- If the injured person has an isolated fragment in the navicular tuberosity, the pain is referred to the lower medial surface of the navicular bone. Soft tissue swelling is also localized in this area.
prophylaxis
To prevent meniscal necrosis, stress on the wrist should be reduced and trauma to the hand should be avoided. If severe or unreasonable pain occurs, a doctor should be consulted. Timely treatment of a fracture of the navicular bone can restore full trophism and avoid complications.
Kinbeck disease is very rare. Doctors are more likely to diagnose a scaphoid fracture after a hand injury if it is not treated in a timely manner. It is important to know that the bones of the wrist are very small and fragile and can be easily injured when the hand is moved in a certain way or when the hand is thrown and dropped.
It is better not to hesitate and seek help immediately after an injury. An examination will show whether there is a fracture and allow treatment to begin in a timely manner. Delay is dangerous for the patient, who experiences significant impairment of wrist function, which inevitably affects the ability to work and overall quality of life. Ankle necrosis can be treated surgically if the pathology is detected in a timely manner.
rehabilitation
Surgical treatment requires the patient to be hospitalized for 3 days. After the operation, the wrist is immobilized with a plaster cast for 5 weeks. A control x-ray is then taken in two projections. When the bones have successfully solidified (healed), the cast is removed and the patient receives physical therapy to restore joint function.
The complaints are referred to an orthopedist/traumatologist, who orders further examinations and makes an objective diagnosis as a basis for treatment. A rheumatologist can also be consulted during the diagnosis.
In advanced cases, surgical treatment may not be advisable. The possibility of surgical intervention is examined in each individual case.
An unsatisfactory treatment result is possible if the rehabilitation recommendations are not followed. For example, the patient may re-injure the wrist or strain the joint. It is important that the doctor's recommendations are strictly followed.
Korshunov VF, Vidasova EV Peculiarities of treatment and rehabilitation of patients with aseptic necrosis of the scaphoid and hemilateral bones // Materials of the seventh city scientific conference 'Medical rehabilitation of patients with pathology of the musculoskeletal and nervous systems'. ¬ Moscow, 2006. ¬ С.203.
Korshunov VF, Vidasova EV. Surgical treatment of aseptic bone necrosis of the scaphoid and semilunar hand // Kremlin Medicine. ¬ №2. ¬ Moscow, 2007. 18¬20.
Andrushko NS, Solodko VI Results of conservative treatment of Kinbeck's disease. – In book: The conservative treatment of traumatological and orthopedic diseases of the upper limbs. – Bitter, 1971 С.251-253.
Read more:- Fracture of the calcaneus of the foot.
- tibia and fibula.
- Bones of the tarsal bone of the hand.
- fracture of the elbow in the foot.
- Fracture of the lateral condyle.
- Injury to the navicular semilunar ligament.
- scaphoid in the foot.
- Cracked metatarsal.
