Torsion of the ligaments of the foot is a relatively common occurrence. It occurs when the foot is suddenly turned inward. Clinically, a sprain is manifested by pain on movement and touch, especially in the front part of the ankle, restriction of movement and swelling. The diagnosis is made on the basis of the clinical and radiological picture. The most important treatment measures are to protect the limb and control the edema (use of ice, compression bandage, elevation of the limb). In more severe cases, surgical treatment is required.

- Pain in the toes
- Conservative treatment
- Possible diagnoses – causes of thickening on the foot
- What is a valgus deformity?
- risk factors
- Old
- Cosmetic surgery on the feet
- Paul
- Occupational Injuries
- pregnancy
- sports and dancing
- Causes of foot pain.
- Prevention against swollen feet
- Conclusions
- forecast
- How do you treat bed sores?
- Treatment of stage 1 pressure ulcers
- Foot paralysis. Types, causes and risk factors
- Causes that can lead to foot paralysis include:
- Depending on the weakness of the contraction of the foot muscles, a distinction is made:
- Symptoms of foot paresis
- Symptoms of foot paresis
- Complications associated with foot paralysis
- Traditional medicine
- prevention
Pain in the toes
Morton's neuroma (also called interdigital or interdigital neuroma) is a common cause of forefoot pain. It manifests itself as a sharp, burning sensation in the spaces between the toes. The pain and burning often radiate up the foot towards the ankle or into the neighboring toes.
Most often, the neuroma is located in the third or second space between the toes and therefore manifests itself as pain, burning and/or numbness between the third and fourth or second and third toes.
In terms of pathological anatomy, it is not a true neuroma. In other words, Morton's neuroma is not a benign tumor of the nerve called a neuroma, but an inflammatory lesion of the nerve and a thickening of the tissue surrounding it.
Wearing shoes with narrow legs or high heels usually worsens the symptoms of the condition.
The medial soleus nerve and the lateral soleus nerve are branches of the tibial nerve, into which it splits at the level of the ankle joint. These nerves provide sensory and motor innervation to the surface of the sole of the foot.
- The median nerve is larger and innervates the skin and muscles of the first, second, and third toes, as well as the inner half of the fourth toe (similar to the median nerve in the hand).
- The lateral cutaneous nerve innervates the outer half of the 4th finger and the entire sole surface of the 5th finger (similar to the ulnar nerve in the hand).
Fingers (similar to the ular nerve in the hand). As they progress, these nerves divide into the common digital nerves, from which the medial and lateral branches of the neighboring fingers arise in front of each interdigital space at the level of the heads of the metatarsal bones. Unlike in the hand, where the branches of the median nerve and the ulnar nerve rarely converge, the third interdigital nerve in the foot is formed by fibers from the median nerve and the lateral popliteal nerve.
In approximately 50-85 % of cases, the third interphalangeal nerve is affected by Morton's nerve, probably because it is larger and lies between the two most mobile bony structures. In other cases, the second interphalangeal nerve is affected. Very rarely, the first and fourth intercostal nerves are affected, and the reasons why the latter two are affected are unclear.
Conservative treatment
Initially, all cases of Morton's neuromas are treated conservatively. Patients are recommended to wear shoes with a roomy toe and a low heel. Soft insoles or a custom orthotic insert may be used to relieve pressure on the painful area.
Non-steroidal anti-inflammatory drugs may be prescribed to relieve pain. In some cases, physical therapy in the form of ultrasound or electrical stimulation may be effective. Injecting a corticosteroid into the space between the toes together with a local anesthetic for diagnostic purposes allows for a fairly long-lasting effect in some cases.
If conservative treatment remains unsuccessful over a long period of time and other possible causes of foot pain have been ruled out, surgical treatment may be indicated.
Possible diagnoses – causes of thickening on the foot

There are many causes of nodules, blisters, cones, and other deformities. When making a diagnosis, the doctor is guided by:
- the location of the formation – a nodule on the outside or bottom of the foot, on the big toe or on the little toe;
- structural features – bony or soft nodules under the skin of the foot, small, large, mobile
- Patient sensations – pain, discomfort, numbness;
- Results of complex diagnostics – CT, MRI, ultrasound of soft tissues, biopsy data.
The doctor is also interested in the causes of the growth and any accompanying diagnosis.
Possible causes of a nodule on the foot:
- A hyproma is often a bump on the back of the foot (on a tendon) or on the crook of the foot, soft-elastic or hard. It does not hurt, but causes discomfort when in contact with shoes. It is a benign cystic tumor on the superficial lining of the joint.
- Plantar fibromatosis – small to large dense thickenings on the sole of the foot, subcutaneous nodules. They arise as a result of a proliferative plantar aponeurosis. Treatment depends on the size and location of the growth as well as the patient's level of discomfort.
- Calloused nails and canker sores are thickened, hardened areas of skin on the sole of the foot that are harmless and usually painless. They look like patches of callused skin with no clear boundaries.
- Taylor foot deformity is a mass at the base of the little toe caused by varus deviation of the fifth toe and valgus deviation of the fifth metatarsal.
- Podagra is a systemic disease caused by impaired purine metabolism. If a man has a painless, dense nodule on his foot, it is most likely tophus or a gout nodule. The nodule may be on the back and arch of the foot, on the toes, or on the heels.
- Osteoarthritis is a degenerative disease in which the articular cartilage becomes damaged. It often occurs as a mass in the area of the big toe joint. It looks like a bump on the top of the outside of the foot.
What is a valgus deformity?
The valgus deformity is described by patients as a bump on the inside of the foot. However, medically, the pathology is defined as a progressive, complex condition associated with deviation of the first toe and loss of stability of the bony structures of the forefoot.
- The abnormal load on the foot leads to a weakening of the musculoskeletal system.
- The bases for walking and standing for long periods have changed.
- The forefoot bones fan out.
- An imbalance occurs in the strength of the muscles responsible for the correct positioning of the big toe.
- The first toe deviates outwards and the metatarsophalangeal joint is deformed.
The patient describes these changes as 'a bump that popped out of the foot and started to grow'. In reality, that is exactly the case. Without treatment and preventive measures, the bunion in the big toe will grow larger, causing pain, discomfort and further joint deformity in the foot.
risk factors
Risk factors for foot pain include the following:
Old
Older people are more prone to foot pain. As we age, the foot becomes wider and flatter. The skin on the feet becomes thin and dry. Foot pain as you age can be a sign of age-related degenerative diseases such as arthritis, diabetes and heart disease. In addition, problems in the feet themselves can affect musculoskeletal balance as we age.
Cosmetic surgery on the feet
Some women have fashion surgery to improve the shape of their feet so they can wear high-heeled shoes. Surgical techniques include shortening the toes, shrinking the foot, or injecting silicone into the soles of the feet. Over time, these procedures cause pain in the foot, and surgeons discourage foot surgery unless indicated.
Paul
Women are more prone to severe foot pain, which is likely due to wearing high-heeled shoes. In the older age group, severe foot pain is a common cause of disability.
Occupational Injuries
Approximately 120,000 work-related injuries occur in the United States each year. About a third of these are foot injuries. Most foot injuries, such as Some diseases, such as arthritis, tunnel syndrome and plantar fasciitis, are caused by excessive stress on the foot (standing for long periods of time and walking long distances).
pregnancy
Pregnant women are at increased risk of foot problems due to weight gain and the release of hormones that make the ligaments more flexible. These hormones help with birth but weaken the foot.
sports and dancing
People who exercise regularly are at higher risk of plantar fasciitis, heel spurs, osteoarthritis, Achilles tendonitis, and bone fractures. Women are more prone to fractures.
Causes of foot pain.
Foot pain can affect different parts of the foot. Bones, ligaments, tendons, muscles, fascia, nerves, blood vessels and the skin can be the source of the pain. The most common causes of foot pain are the following conditions:
- plantar fasciitis.
- osteoarthritis
- Podagra
- athlete's foot
- Rheumatoid arthritis
- Condylar deformity of the foot (hallus valgus)
- Achilles tendon injury
- Diabetic foot
- calluses on the foot
- heel spur
- clubfoot
- metatarsalgia
- fractures
- Morton neuroma
Prevention against swollen feet
If you don't have any medical problems, but your feet are constantly swollen, it's worth changing your lifestyle.
Start by limiting the consumption of hot spices, especially salt, as they can inhibit the excretion of fluid from the body.
You should also control the amount of water you drink throughout the day - an average person should consume no more than 2.5 liters per day.
If you work while standing or sitting, take short breaks to stretch tired legs. You should avoid wearing high-heeled shoes for the duration of the problem. You should also pay attention to your sitting position: until the swelling subsides, you should give up the leg-to-foot position; If you sit on a chair, make sure that the edges of the chair do not press on your thighs.
If swelling occurs without any obvious health problems, it is worth seeing a specialist.
The doctor will prescribe the necessary tests and determine the true cause of the problem.
Conclusions
Even if you do not have any health problems, you should not treat yourself on your own. Swelling in the feet can be a sign of serious illnesses that are not obvious.
If the swelling in your lower limbs does not go away within a few days, you should definitely see a qualified doctor.
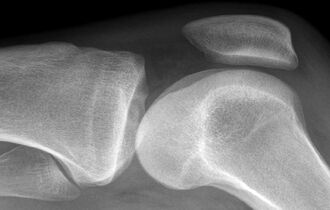
What an MRI scan of the knee joints shows, how the procedure is carried out: decoding and contraindications
Since the structural elements of the examined area are visible from all sides during the examination,…
Sciatic nerve entrapment: causes, symptoms, treatment, prevention
The sciatic nerve is the longest nerve in the human nervous system. It originates in…

Intercostal neuralgia: symptoms and diagnosis
Intercostal neuralgia is one of the most common causes of severe chest pain….
forecast
The prognosis for sprains is favorable. Grade 1 sprains usually heal without any side effects. With sprains of the 2nd and 3rd degrees, there may be tingling and pain in the joint for a long period of time, which may be due to the involvement of nerve endings in the pathological process. The ligaments are repaired by scar tissue, causing weakness. The connective tissue is no longer sufficiently elastic, so the risk of another injury increases. It is recommended that the patient wear a special splint.
Conclusions
A sprained ankle can be effectively repaired with RICE (rest, cold, compression and elevation) treatment. If pain is severe, analgesics are indicated.
How do you treat bed sores?
During long-term inpatient treatment, it is not always possible to be completely free of pressure sores. Older patients with very weak immune systems and vascular diseases are particularly at risk.
The treatment patterns and methods depend on the different stages of the pressure ulcer, of which there are four:
1. First stage. – Large purple spots form on the skin that do not disappear even with pressure or a change in posture. The integrity of the skin is not affected.
2. Second stage. – Bubbles with watery contents form within the red spots. They burst when they rub against clothing, exposing a shallow wound.
3rd stage – The wound enlarges and penetrates deep into the subcutaneous fatty tissue and muscle layer. Fluid and pus may leak from the thickness of the wound. The decubitus ulcer appears as a deep depression with jagged edges.
Stage 4. – The wound penetrates through the muscle into the tendons and bone. A black mass of dead tissue (necrosis) forms on their surface. Purulent discharge and an unpleasant odor may occur.
Treatment of stage 1 pressure ulcers
Before any manipulation of the skin, the nurse washes and treats the patient's hands with the antiseptic Softa-Man Iso Viscorab. The patient's body position is then changed to relieve pressure from the area where the pressure ulcer formed.
Treat the red area and the skin around it with Eplan solution, Seni Care cream with arginine or similar products. These products relieve pain, soften and protect the skin, accelerate the regeneration of damaged tissue and stimulate blood circulation. Massages in the form of gentle strokes in a clockwise direction increase the effect of the products on pressure sores.

At the end of the hygiene treatment, a breathable bandage such as Askin Hill or Askin Derm is placed on the stain. It protects the wound from maceration and mechanical damage. During the entire treatment period, care should be taken to ensure that the patient does not lie on the injured area.
Foot paralysis. Types, causes and risk factors
Foot paralysis is a pronounced weakness of the lower leg and foot muscles. It is a defect in which the foot does not straighten completely and can drag to the ground or sink when walking. It is also referred to as: 'horse foot', 'hanging foot' or 'toe paralysis'.
Paralysis of the foot is not a disease in itself, but simply a symptom of abnormalities in nerves, muscles or bones.
A distinction is made between unilateral and bilateral foot paralysis.
Another classification divides foot paralysis according to the cause and the degree of severity.
Causes that can lead to foot paralysis include:
- Herniated disc (more common in the lumbar spine, which is associated with compression of the spinal cord or nerve roots).
- Damage to the fibular nerve.
- Trauma or illness that damages the sciatic nerve.
- Pathology of the lumbosacral nerve plexus.
- Cauda equina syndrome (damage to the nerve roots in the spinal canal).
- Spinal cord and brain injuries.
- Diseases of the spinal cord and brain (poliomyelitis, tumors, acute cerebral circulatory disorders).
- Genetic abnormalities of the nervous system (neural amyotrophy and hereditary neuropathy).
Depending on the weakness of the contraction of the foot muscles, a distinction is made:
- Grade 0 – Contraction with weight bearing on the foot (normal).
- Grade 1 – contraction with low load on the foot.
- Grade 2 – Contraction to overcome gravity.
- Grade 3 – slight contraction (without overcoming gravity).
- Grade 4 – Twitching of the muscle ('trembling' contraction).
- Grade 5 – complete absence of contraction (paralysis).
Because the nerve that controls foot elevation passes close to the surface of the skin on the outside of the foot, any compression of this nerve can be considered a risk factor for developing foot palsy.
Symptoms of foot paresis
As already mentioned, the main symptom of foot paresis is a fluttering, slouching or 'cramped' gait. The person affected by this pathology has to lift the foot up or pull it up on the ground. Due to the paresis of the extensor muscles, the foot does not move up and reaches a flexion of more than 80 %.
The symptoms that accompany foot paralysis include:
- Pain in the foot with tingling or numbness
- Impairment of flexion of the foot
- Sensory disturbances on the dorsal and sole sides of the foot
- Muscle wasting in the lower extremity (caused by a herniated disc and central nervous system dysfunction)
Symptoms of foot paresis
When walking with a foot paralysis problem, a wobbly gait is evident: the person walks with their leg raised or dragging it on the ground. Another characteristic movement of the foot is walking on tiptoes with a strong swing of the hips or excessive sideways movement of the hips. Due to extensor palsy, the foot does not lift, folds over when walking and twists more than 90 degrees.
- Moderate pain in the foot
- Tingling and numbness in the foot
- Impairment of flexion of the foot and toes
- Difficulty climbing stairs
- Sensory disturbances on the sole of the foot and on the outer edge of the foot
- Muscle loss in the feet (often caused by a herniated disc or spinal cord injury)
Complications associated with foot paralysis
If patients with foot paralysis seek medical attention early, the foot can be completely healed and the patient can walk normally again. Without timely treatment, foot paralysis can progress and lead to serious complications.
One of the consequences of the disease is foot deformity. In the early stages of the disease, it is easy to return the foot to the correct position using muscle strength, but over time this becomes more and more difficult without fixation. In order to avoid irreversible deformations, the cause of the disease must be determined as quickly as possible: it can be a spinal disease or a consequence of muscle injuries.
Sometimes foot paralysis leads to paralysis of the lower limbs and the patient is unable to move independently. In such cases, it is important to fix the foot in the correct position in a timely manner so that the shape of the leg is not changed in a degenerative manner. For this purpose, the doctor prescribes special orthopedic shoes and other aids to the patient.
Traditional medicine
If you are sick with parotitis, you can resort to folk remedies after consulting a proctologist.
- Baths with salts. An effective means of eliminating unpleasant and painful sensations is a bath based on salt and soda. Boil 5 liters of water, let it cool until warm, then dissolve 1 teaspoon each of salt and baking soda in it. Strain the liquid through cheesecloth and then take a seated bath for 10 minutes. A series of 15 such treatments.
- Shilajit bath. Another bath for chronic paraproctitis is based on Shilajit. Dissolve 10 tablets in a glass of water, stir well and strain. The resulting solution, add 5 liters of warm boiled water, infuse for a few minutes and then take a bath.
- Rinse with calendula infusion.. The preparation is very simple: soak 20 grams of fresh or dried flowers, pour a glass of boiling water over them, let it brew for two hours and then do an enema. It is recommended to apply oil or cream to the edge of the syringe.
- Rowanberries. They have a mild laxative effect. From them you need to squeeze the juice - about half a cup and drink a little each 3 times a day before meals. Use the rest of the pulp to make a compress around the anus.
prevention
There are no specific measures to prevent this disease. General advice to prevent the development of paraproctitis:
- All anal diseases must be treated timely and correctly.
- Chronic infections of other body systems cannot be ignored.
- Proper intimate hygiene is very important.
- Visit the proctologist regularly for preventive examinations, and do not hesitate to consult a specialist if your body gives the first warning signs: pain, discomfort in the anus, weakness.
- Morton shoe inserts.
- Morton's Neuroma Ointment.
- tendons of the foot.
- metatarsal bones.
- Treatment of metatarsalgia of the foot.
- metatarsalgia.
- The tarsal bone hurts from above - what to do?.
- Syndrome of the tibial nerve.
