Anterolateral instability of the knee joint Occurs when the lateral condyle of the tibia moves forward; Anterolateral instability occurs when the medial condyle of the tibia moves forward. These types of rotational instability of the knee joint severely limit physical activity.

- instability of the knee
- causes
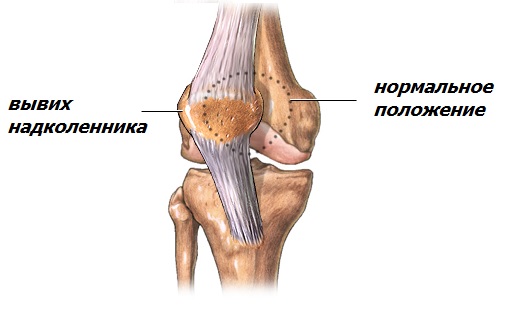
- Dislocation of the kneecap.
- Cartilage damage of traumatic origin.
- What diagnostics are required to perform an osteotomy?
- How is the operation performed?
- Contraindications to MRI scanning of the knee
- Preparation for the MRI scan of the knee
- Knee joint
- Detecting anatomical landmarks [edit edit source]
- Knee joint: anatomy and physiology of muscles
- The innervation of the tissues adjacent to the knee joint
- Physiology and pathology of the knee: the chain reaction to injury
- Causes of patellar luxation
- Symptoms of a dislocated kneecap
- prevention
- Nourishment
- ARTHROSCOPIC CRUCIAL LIGAMENT SURGERY
- Statistics on Autograft Use in Primary Anterior Cruciate Ligament (ACL) Pplication in Athletes
instability of the knee
The stability of the joint is a prerequisite for good function. It can move with a certain amplitude and in certain directions, and all loads will be correctly distributed. This stability is ensured by the joint capsule, the ligaments and the normal condition of the joint cavity. Unstable knee joints lead to a redistribution of loads. Not only does the joint itself suffer, but also the adjacent structures.
The main cause of knee joint instability is damage to the cruciate ligaments. They are located in the joint cavity and connect the articular surfaces of the shinbone and femur. A cruciate ligament injury often occurs due to trauma, combined with meniscal damage and hemarthrosis (accumulation of blood in the joint cavity).
causes
The disease often occurs as a result of serious accidents and also as a result of competitive sports such as football, ice hockey, running or cross-country skiing. The following activities can lead to the development of the disease:

People with a genetic predisposition (underdeveloped ligaments) are most susceptible.
Dislocation of the kneecap.
When the knee joint flexes and extends, the kneecap moves on the femoral block like a train on a rail. However, there are reasons for abnormal movement and the train derails - dislocation of the kneecap occurs.
Causes: abnormal development of the femoral block and condyles, anatomical anomalies, tear of the medial retention of the patella, patella alta (elevation of the knee cap due to an excessively long patellar ligament), weakness of the quadriceps muscle, abnormal position of the tibial tuberosity.
Many conservative treatments are used to correct anatomical abnormalities with good treatment results. However, if no effect is achieved or there are a large number of dislocations, surgical treatment is indicated.
There are open and arthroscopic techniques for stabilizing the kneecap, depending on the examination and the cause of the instability. X-rays of the knee joint in 2 standard projections and axial (oblique) views as well as magnetic resonance imaging are important for the diagnosis, and computed tomography (CT) may also be required.
After the operation, a special orthosis that restricts movement in the knee joint, walking on crutches, exercises with a physiotherapist and physical therapy are recommended.
Restoration of joint function can be expected within 2 months after surgery, and return to sport after approximately 4 months.
Cartilage damage of traumatic origin.
Injuries to the knee joint Injuries to the knee joint Ligaments and meniscus can remain intact due to their elasticity. In contrast, solid structures such as cartilage can be destroyed. Cartilage tissue is very difficult to heal, which is why plastic surgery is necessary if there are defects. Cartilage defects of up to 1-1.5 cm2 in non-loaded articular surfaces and with good cartilage plates around them are usually tunneled or microfractured. Loose fragments are removed, the defect is scraped down to the bone (refreshed), and channels are created throughout the defect to allow blood flow from the bone marrow. This technique provides a regenerative vascular response by promoting filling of the defect with fibrous scar.
Defects in the accentuated areas can be considered an indication for mosaic chondroplasty. Cylindrical columns about 2 cm high and 6-8 mm in diameter, consisting of healthy cartilage and underlying bone, are harvested from donor sites using special instruments. After appropriate preparation, these columns are placed on the defect site and fill the required space like a mosaic. The possibilities of this technique are limited by the size of the defect itself and the amount of donor material. The best results are achieved when the size of the cavity does not exceed 3 cm2.
An alternative technique that can be used to close larger cavities is the implantation of a collagen matrix. The cavity is also refreshed and channels are introduced into the cavity through which blood and bone marrow elements can flow to the surface. This matrix, which can be glued with a special medical adhesive or sewn to the edge of healthy cartilage, is needed to hold it to the surface of the defect. The matrix impregnated with bone marrow elements forms the basis for filling the space with a fibrocartilage scar.
Chondroplasty techniques are mainly open surgical treatment, that is, with an incision. Tunneling of small defects, on the other hand, is carried out arthroscopically.
What diagnostics are required to perform an osteotomy?

Analysis of the axis of the lower extremity before surgery when the patient is standing. It is a varus deformity of the lower leg with overloading of the medial side of the inner joint. © Joint Clinic
First, a clinical examination is carried out during which the orthopedist collects all information about the existing knee joint defect. He then examines the patient's leg and approaches the axis of the limb. An X-ray from the hip to the foot will determine the exact extent of the problem. Based on the images, the doctor can plan the operation.
The patient is also referred for an MRI scan. This examination can detect damage to the meniscus and differentiate local damage to the articular cartilage from larger lesions.
How is the operation performed?
The tibial osteotomy is usually performed under general anesthesia. An incision on the inside or front of the knee creates access to the knee joint and shinbone. The joint is then examined. To align the axis of the tibia, it is cut at an angle and a wedge-shaped hole is created. This hole is filled with a bone graft that is secured with a metal plate and screws. This helps keep the wedge in place. The incision is closed and the knee and leg are placed in a splint.
As a rule, the patient stays in the clinic for three days after a knee osteotomy. On the day of the operation, the leg can be loaded with around half of your body weight. Full strain is usually possible after about four to six weeks.
Physiotherapy speeds up the healing process significantly.
After a knee osteotomy, sporting activities such as swimming or cycling can be resumed after four weeks. For other sports, consultation with a doctor is required.
Contraindications to MRI scanning of the knee
The main limitations relate to the presence of solid metallic structures and foreign bodies in the body.
- Ferromagnets. These have intrinsic magnetization and can behave unpredictably when exposed to a strong external magnetic field. These include iron, nickel, cobalt and some alloys. MRI should not be performed if these are present in the body.
- Paramagnets. In the absence of an external magnetic field they have no magnetic properties. For example titanium, platinum. They are not dangerous, but can be disruptive if they are in the study area.
The doctor makes the final decision after studying the documents describing the composition of the product.
Absolute contraindications for an MRI scan are:
- Presence of electronic devices – pacemaker, cochlear implant, insulin pump and others;
- The first trimester of pregnancy;
- Severe claustrophobia.
Our medical center does not examine children under 5 years old; For an MRI scan of the knee under anesthesia, parents should visit a specialized pediatric facility. If you weigh more than 150 kg, an MRI scan of the knee joint is also difficult to perform due to the design of the scanner.
Preparation for the MRI scan of the knee
No special preparation is required and you can have your MRI scan done at our medical center on the day of your appointment.
Before the examination, you will be asked to remove all accessories and clothing containing metal and to remove all bank cards and other magnetic cards.
Be sure to tell your doctor your medical history and the results of previous examinations. This allows him to specifically address any concerns and choose the best protocol for the procedure.
Knee joint
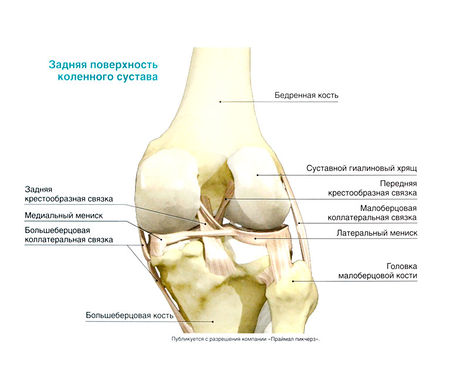
The knee joint is formed by the distal end of the thigh and the proximal end of the tibia. The proximal end of the tibia also forms an intercondylar joint with the fibula, allowing both bones to slide together during pronation and supination of the foot. At the front, the kneecap attaches to the distal end of the femur and forms the patella-thigh joint, which is important for the function of the knee joint.
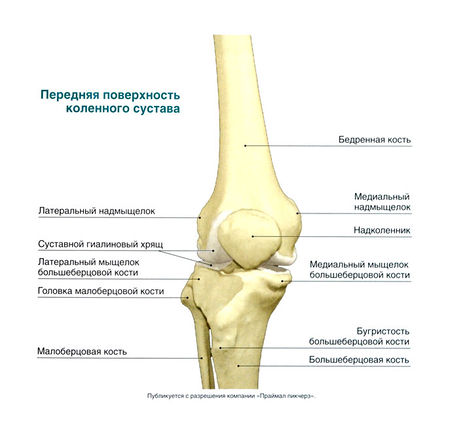
Biomechanics of the knee joint on the x-ray
The knee joint belongs to the group of Joint capsulesIt moves in two axes. The most important movements are: Flexion and extension - these are carried out about the anterior axis (Fig. 3.1), but in addition the tibia rotates inwards during flexion and outwards during extension.
The relatively flat knee joint is reinforced by several ligaments. The tibial collateral ligament (medial) strengthens it on the medial side and prevents excessive valgus movement of the tibia, and that Collateral ligament of the humerus (lateral) strengthens it on the lateral side and prevents excessive varus movement of the tibia.
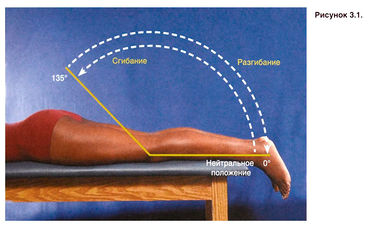
Figure 3.1. Volume of movement in the knee joint.
- Valgus alignment of the lower limbs – Lateral displacement of the distal part of the lower limbs (as in an X-shaped curvature).
- Varus of the lower limbs – Medial displacement of the distal part of the tibia (as in an O-shaped curvature of the leg).
Anterior cruciate ligament (ventral ligament) – Ligament that runs within the knee joint from the anterior edge of the tibia to the posterior edge of the femur; restricts the anterior displacement of the tibia relative to the femur and its rotation.
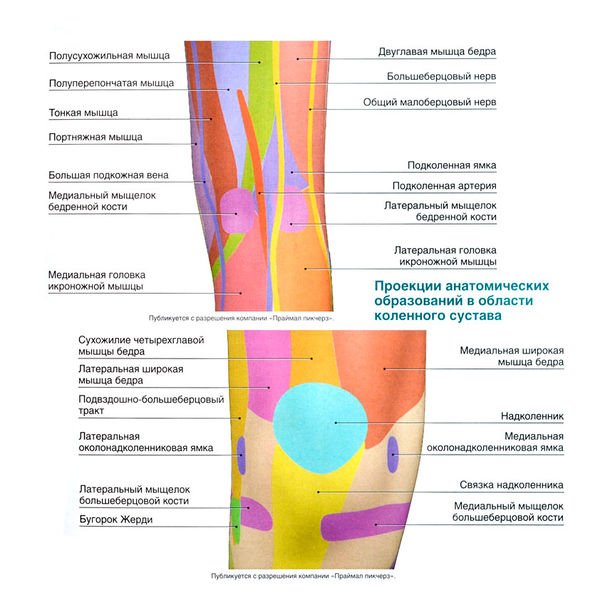
Detecting anatomical landmarks [edit edit source]
- knee braces
- Hyperextension of the knee joint
- Hamstring syndrome
- Hamstring strain (treatment)
- Meniscus tear: symptoms and treatment
- Cracked osteochondritis
- Injuries and damage to the quadriceps muscle
- Torn quadriceps tendon
- Tear of the patellar ligament
- Tear of the tibial tuberosity (tuberositas tibiae)
- Ligaments of the knee joint
- Tear of the collateral ligament (collateral ligament)
- Tear of the anterior cruciate ligament
- Tear of the anterior cruciate ligament
- Chondromalacia of the knee: symptoms and treatment
- Subluxation and dislocation of the kneecap
- Tenosynovitis of the patellar ligament
Knee joint: anatomy and physiology of muscles
The alternating contraction and diastole of the muscles causes the knee to move in three planes, allowing flexibility and stability of the lower limbs. Therefore, the basic classification of muscles is not based on the anatomy or the location of the individual muscle groups, but on their function:
- The flexion of the knee. This movement is achieved through the balanced and complete work of the most developed muscle group of the knee joint. These include the biceps, semitendinosus, semitendinosus, hamstring, calf, soleus, tailor and lean muscles.
- Extension of the joint. Only one muscle is responsible for this function - the quadriceps, the largest muscle in the leg. It consists of straight, lateral, medial and middle broad muscle fibers.
- Pronation is the inward movement of the leg. The limited 'rolling' of the lower limb towards the internal axis is facilitated by the popliteal tendon, semitendinosus, hamstring, coccyx, semitendinosus and the medial head of the calf muscle.
- Supination is an outward movement. The outward rotation of the tibia is made possible by the contraction of the heads of the biceps and lateral calf muscles.
The innervation of the tissues adjacent to the knee joint
The nerve fibers of the knee joint form a vast interconnected network that allows the lower limbs to do their best work. Although the knee's neural network is not very extensive, each component plays a key role, meaning that the slightest disruption 'paralyzes' the entire joint mobility system.
The local nervous system in the knee area consists of the following nerves:

- The meniscal nerve bundles penetrate the tissue along the periphery of the cartilage body itself and follow the course of the blood vessels of the knee. These nerves contribute to the parenchymatous and non-muscular fibers and support the proper innervation of the joint tissue.
- The tibial nerve with its articular branches provides sensitization of the posterior surface of the knee.
- The fibular nerve innervates the anterior portion of the knee, including the calyx.
Physiology and pathology of the knee: the chain reaction to injury
Knee injuries are among the most complex in orthopedics - and for good reason: every muscle or ligament fiber, every cartilage or bone influences the function and mobility of the joint. Even a minor deviation, such as a slight inflammation of the ligaments or a bruise, can set in motion destructive processes, the healing of which requires lengthy and serious therapy.
It is known that the bone surfaces do not fit together like a puzzle to ensure full mobility. So when the ligaments, muscles or meniscus that hold the joint in its physiological position are affected, the cartilage tissue gradually begins to wear away. This degeneration usually only becomes clearly visible in the final stages: At first, the sensation of a pathological process can be dismissed as the result of a sprain or overexertion. Pain, abnormal noises during flexion/extension or discomfort during strain therefore require an accurate diagnosis of the knee joint and timely qualified help.
Causes of patellar luxation
A dislocation of the kneecap is very often the result of trauma. Anatomically, this part of the kneecap is covered by the femoral and tibial heads, which are separated by the lateral and medial meniscus. The kneecap is firmly connected by the anterior cruciate ligament and allows the joint to be mobile in flexion and extension of the leg.
The most common injury that causes a dislocation of the knee joint is a dislocation and sprain of the joint capsule. The second most common injury is a sprain and tear of the anterior cruciate ligament with subsequent severe scarring. These injuries do not provide stability to the kneecap. Therefore, if the leg is tilted slightly, a sprain occurs. This condition is accompanied by severe pain, swelling and hypersensitivity of the surrounding soft tissues.
Other causes of kneecap dislocation include:
- Excessive body weight, which significantly increases the potential physical and mechanical stress on all major joints of the lower limbs;
- a misalignment of the foot that changes the position of the femoral and tibial heads in the joint capsule, creating a risk of overloading the ligaments and dislocating the structural components;
- Valgus and labral deformities of the tibia or femoral neck
- wearing uncomfortable footwear;
- sports injuries;
- Excessive physical exertion;
- Meniscopathy and deformation of the cartilaginous synovium at the bone heads;
- deforming osteoarthritis;
- Ankylosing spondylitis;
- systemic connective tissue and cartilage diseases;
- muscular fiber dystrophy, etc.
It is very important to determine the possible cause of the knee sprain before starting treatment. Only when this has been eliminated can full treatment begin. Otherwise, the disease may come back immediately after treatment.
Symptoms of a dislocated kneecap
The clinical symptoms of a dislocated knee joint occur when the integrity of the joint is compromised. This causes severe pain, comparable in intensity to that of a broken bone. Therefore, it is necessary to consult a trauma surgeon immediately after such an injury in order to exclude the possibility of damage to the integrity of the bone using X-rays.
In most cases, symptoms of a dislocated knee include instability and wobbling, causing fear of taking steps with the affected limb and a feeling that the leg may bend in unintentionally in unpredictable directions. The surrounding muscle tissue is weakened.
With a patellar luxation, the symptoms are even more varied and include:
- Visually recognizable deformation of the knee joint;
- When attempting to move the kneecap, it gives way easily and without effort, but considerable pain occurs;
- Instability of the leg when standing, with a feeling of instability;
- Pain localized in the middle of the knee and radiating to the back of the knee;
- If the anterior cruciate ligament is ruptured, a crunching sound can be heard on palpation, which gradually turns into a clicking sound;
- The knee can no longer be bent and extended freely;
- When trying to forcibly bend or straighten the leg, pain and a cracking sound occur;
- Rapidly progressive contracture of the joint;
- Dense areolar edema of the peripheral soft tissues around the joint (when pressed with a finger, the characteristic depression is not preserved);
- The skin may be congested (in the inflammatory phase) or covered with hemorrhages (formation of hematomas in bruises due to tearing of the soft tissues of the ligamentous apparatus);
- Nausea in the lower leg (the swelling causes compression of the sciatic nerve near its foramen to the tibial and ankle branches).
prevention
Prevention and adherence to medical advice play an important role in the development of gonarthrosis. To slow down the degeneration of the joint it is necessary
- perform exercises that do not put too much strain on the joint, such as therapeutic exercises and gymnastics;
- avoid strenuous exercise;
- choose comfortable orthopedic shoes;
- Pay attention to your body weight and your daily lifestyle - alternate between special exercises and rest periods.
Nourishment
The condition of the affected cartilage largely depends on diet. If you have osteoarthritis, you should avoid the following:
- carbonated drinks;
- alcoholic drinks;
- fatty and overly spicy foods;
- canned and semi-finished foods;
- Foods with colors, preservatives and artificial flavors.
The diet should contain the following: protein, fatty acids, e.g. B. Omega-3, collagen, which is contained in gelatin. It is necessary to eat without increasing body weight.
ARTHROSCOPIC CRUCIAL LIGAMENT SURGERY


2. Positioning the patient on the operating table

3. Installation of arthroscopic optics and manipulators


5. Transplantation of the cruciate ligament onto the suture

6. Tunneling under optical control
Statistics on the use of autografts
In primary plication of the anterior cruciate ligament (ACL) in athletes
1.1 % – tendon autograft 4
Male, 28 years old, 1 year after anterior cruciate ligament (ACL) surgery.
The graft was made from the tendons of the triple compound semitendinosus and double tendon muscles.
In this MRI image, the new anterior cruciate ligament transplant is indistinguishable from the ligament that was torn during the injury.
- Pronation and supination of the knee joint.
- How much does knee surgery cost?.
- The lateral dislocation is.
- tibial ligaments.
- Dislocation of a bone in a joint.
- Femoral collateral ligament.
- Rupture of the medial collateral ligament.
- The sit bones.
