X-ray of the cervical spine in lateral projection does not show displacement of the vertebral body after trauma because the patient's shoulders obstruct the view.
- Anomalies and malformations of the spine
- Asymmetrical position of the articular plates
- Hypoplasia
- Symptoms of an ulnar fracture
- Diagnosis of fractures of the ulnar process with and without dislocation
- Causes of mandibular fractures
- First aid for lower jaw fractures
- triggering factors
- How osteophytes are treated today
- Treatment of sprains and subluxations
- The cervical plexus is a superficial part of the
- Stellate ganglion
- X-ray
- Surgical treatment options.
- Symptoms, diagnosis
- Hand extension test
- Surgical treatment of fracture of the elbow process
- Immobilization of the elbow joint with screws
Anomalies and malformations of the spine
Chiropractic practice During chiropractic treatment, radiologists pay attention to all the details and deformities of each patient's spine.
Vertebral malformations play a key role in this. This article only discusses the most common malformations that radiologist encounters almost every day.
The numerous classifications of malformations and spinal anomalies are based on the experiences of leading surgical clinics. They are useful to surgeons and radiologists in terms of general understanding of the processes of embryogenesis and ontogeny of the spine.
The practice of working with chiropractors shows that it is much more important to know the anomalies that do not require surgical intervention, but should be taken into account when analyzing the spatial position of the vertebrae.
Developmental abnormalities help the radiologist explain why the scoliosis occurred and where the early osteochondrosis in this particular patient came from in these vertebral segments.
Developmental anomalies and malformations have a significant influence on the statics of the The spine Spine and the movement in the individual motor spinal segments. It is more likely that these are multiple anomalies.
In 88 % cases they occur throughout the spine, with an average of five abnormal vertebrae per patient [Ulrich EV, 1995].
Changes in the number of lumbar vertebrae and Sacral vertebra. Sacralization of the fifth lumbar vertebra occurs when the transverse processes become large and form an anatomical connection with the sacrum and ilium of the pelvis, which may be bony, cartilaginous or articulated, immobile or mobile. In the latter case it can cause pain. Functionally, only four vertebrae remain in the lumbar spine [Maykova-Stroganova VS, Finkelstein MA, 1952].
Asymmetrical position of the articular plates
The asymmetrical position of the articular plates of the vertebrae is called Tropism anomaly. One of the articular processes occupies the normal position, closer to the sagittal plane, while the other protrudes with its long axis into the frontal plane. Tropism anomalies of the thoracic, lumbar and sacral parts occur (according to the skeletons) in 33 % cases [Diachenko VA 1954]. Shortening of the articular processes was found in 19 % cases.
Complete loss of the vertebral arches (posterior spina bifida) occurs in 19 % cases. The most common developmental anomaly affects the first sacral vertebra (5-10 %). An open sacral canal (S1-S5) is found in 3.6% of cases [Diachenko VA 1954; Ulrich EV, 1995]. Non-union of the vertebral bodies (anterior spina bifida) is most common in the thoracic segment with 5.28 % [Diachenko VA 1954; Ulrich EV, 1995].
The congenital bilateral deformity (spondylolysis) is most common in the fifth lumbar region with 4.5-5 %. Anomalies in the number of ribs can have a significant impact on the statics of the spine.
For example, the formation of additional ribs, in particular asymmetrical ribs, can be one scoliosis. Cervical ribs occur in 0.5-1.5% (according to Diachenko VA 1954) to 7% (according to Maykova-Stroganova VS, Finkelstein MA 1952) of patients, lumbar ribs in 8-9%.
Hypoplasia
Underdevelopment (hypoplasia) or complete absence (agenesis). XII ribs occur in 0.5-0.9 % of cases. Limitations in thoracic mobility and function are often associated with variants of rib development (cleft formation, synostosis, exostosis, disarticulation, rib concretion, etc.), occurring in 0.5-1 % of patients.
Anomalies in cranial and spinal development are of particular importance. In a study by MK Mikhailov (1983) these were found in 8 % patients.
Read more:Insufficiency of the posterior arch of the first cervical vertebra occurs in 1.3 % of patients, blockage (concretion) of the second to third cervical vertebrae in 2 %, and complete assimilation of the first cervical vertebra and occipital bone in 1-2 % of skeletons.
Symptoms of an ulnar fracture
When consulting the doctor, the patient complains of pain syndrome and impaired function of the elbow joint.
Physical and specialist examination reveals the following symptoms of an ulnar process fracture
- deformation and swelling of the elbow joint;
- Restriction of extension and flexion of the forearm (in the event of a sprain, extension is limited because the triceps only pulls on the broken fragment);
- hemarthrosis (bleeding into the joint);
- Pain on palpation of the spinous process;
- In the case of a fracture of the spinous process with displacement, a skin depression can be seen instead of the typical bony process.
Diagnosis of fractures of the ulnar process with and without dislocation
In fractures of the ulnar process without dislocation or with acceptable dislocation, no deformity of the elbow joint is detected. Movement is only limited by pain, meaning the function of the arm is not affected. Therefore, it cannot be said with certainty that there is no fracture with normal function.
To determine whether there is a fracture, an x-ray of the elbow joint is taken in two projections. This examination is sufficient in most cases. To examine the type of fracture in more detail, a computed tomography (CT) scan is performed. In this way, the extent of damage to the appendix can be determined and a treatment strategy can be determined. Whether to operate and which metal structures to use. All these nuances are very important for better fixation and the best treatment result.
Causes of mandibular fractures
There are four types of mandibular injuries:
1. Domestic injuries that occur during conflicts at home or during housework.
2. Road traffic injuries caused by the use of vehicles and road traffic injuries not caused by the use of vehicles. These include falls while walking on ice, other bad weather conditions, or illness.
3. Sports injuries sustained during sporting activities.
4. Occupational accidents suffered in industrial production in agriculture.
With a fracture of the lower jaw, patients may experience limited or no mobility of the lower jaw, pain that may worsen with movement, biting or chewing, bite problems, changes in skin sensation on the lower lip or chin, and bleeding from the mouth a characteristic symptom of a tear in the mucous membrane.
The range of complaints reported by the patient helps the doctor understand the injury and the location of the fracture.
The diagnosis is based on the examination and recording of the patient's complaints.
When examining the patient, the doctor notes the condition of the skin, determines whether the patient has bruises, abrasions or lacerations, notes the presence of hypersensitivity, bruises. He determines whether there is asymmetry on the injured side of the face.
If a lower jaw fracture is suspected, the doctor will first feel the unaffected area and then the injured area with his fingertips. He notes the most painful places, irregularities, disruptions of integrity and determines the amplitude of the mandibular head in the socket by inserting the fingertip into the external auditory canal. The doctor determines the condition of the mandibular head or its displacement by palpating the area in front of the ear canal both in motion and at rest.
A fracture of the lower jaw can be confirmed by a number of symptoms accompanied by pain in the area of \u200b\u200bthe fracture:
First aid for lower jaw fractures
Can be performed at the scene of an accident or in an ambulance. Can be provided by both medical and non-medical personnel as a form of mutual aid.
The injured person is temporarily (for a few hours) fixed with bandages or other devices (the upper jaw is pressed against the lower jaw) so that the injured person can be transported to a medical facility.
For fixation can be used: a temporomandibular joint circular bandage, a soft chin sling (Pomerantseva-Urbanskaia), an entina splint (a rigid standard transport bandage) and various types of interjaw ligature bands. In the event of a traumatic brain injury, ligature bandages should be used with extreme caution as the immobilized jaws do not allow the mouth to open and may result in aspiration of vomit or blood.
triggering factors
Osteoarthritis develops over a long period of time. In order for it to progress from a chronic first stage to a painful second stage, a triggering factor is required. Such triggers include:
- Trauma, e.g. B. a fracture of the middle long bone (on the edges of the fracture osteophytes form in the form of bone marrow);
- Fracture of the periosteum (the body uses the osteophytes to attach the periosteum to the bone);
- Inflammatory processes (arthritis, osteitis, brucellosis);
- malignant joint diseases such as: B. a sarcoma.
If you have arthritis, your risk of developing osteophytes in your joints increases.
How osteophytes are treated today
Treatment of osteophytes is part of the overall treatment of coxarthrosis, gonarthrosis or arthritis of another joint. It is almost impossible to get rid of the bone growths. The goal is to relieve pain and increase range of motion. For this purpose, the patient is prescribed various medications depending on the stage of arthrosis:
- Ointments to relieve unpleasant symptoms, e.g. B. Hydrocortisone;
- non-steroidal anti-inflammatory drugs in the form of tablets or injections into the joint;
- Physiotherapy – lasers, magnets, electrophoresis and shock wave therapy.
One of the physiotherapy treatments for joint pain is magnetic therapy. The specialist explains what it consists of and why it helps:
Treatment of sprains and subluxations
Restoring dislocated and subluxated vertebrae is not an easy task, even under anesthesia. Incomplete unilateral cervical dislocations are more easily corrected by pulling the neck behind the head (along the body) with a Glisson sling and rotating it in the opposite direction; Complete cervical dislocations, ie those with 'traction', must be resolved by bending the head in the direction of the dislocation and then turning it to the healthy side, keeping the traction constant. Once the clutch is released and traction is maintained, a reverse maneuver is performed by pulling the head back to the sound side and then rotating it to the dislocated side.
In an emergency, a Gardner-Wells orthosis is used; The neck is lengthened using an adjustable block attached to a radiolucent table.
It is recommended to first convert a flexion dislocation of the cervical vertebrae into a rotational dislocation, unilaterally, and then carry it out. After the reduction, an operation to stabilize the vertebrae is performed (discectomy with anterior and posterior spondylodesis). For this purpose, various designs of fixation plates, implants (cages) and transpedicular fixation screws are used.
In the cervical spine, these dislocations most often occur at the level of C3–C5, C5–C6 C3, ie in the middle part of the cervical spine, where the greatest anterior mobility exists. In the area of the two upper cervical vertebrae (C1 i C2), where there is no cartilaginous disc and the joints are wide, are so heavily bandaged that dislocation at this level is rare and exceptional. contortion C1 Dislocation of the C1 vertebra (displacement of the skull relative to the atlas) is possible during acute head flexion or rotation and is almost always fatal.
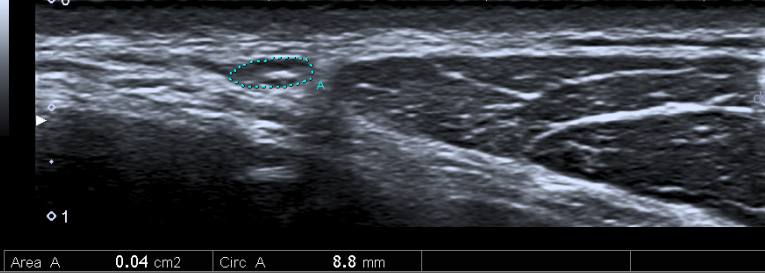
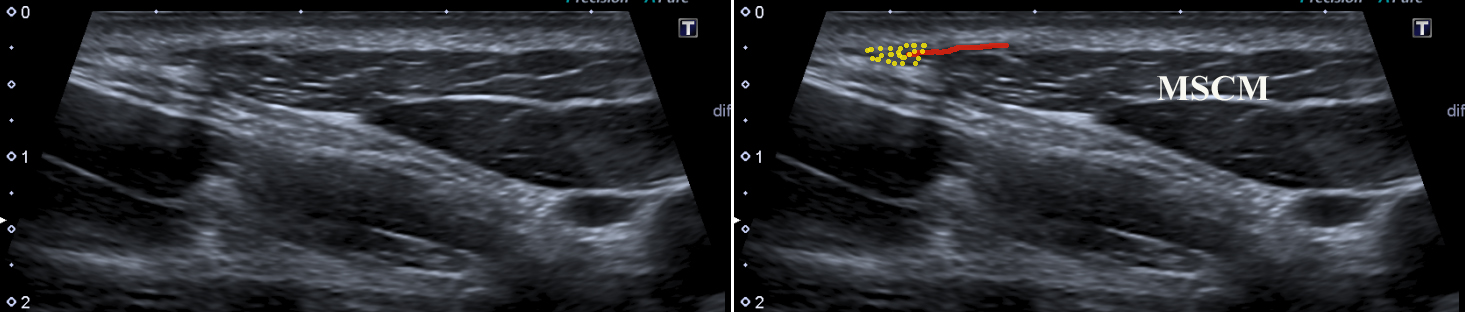
The cervical plexus is a superficial part of the
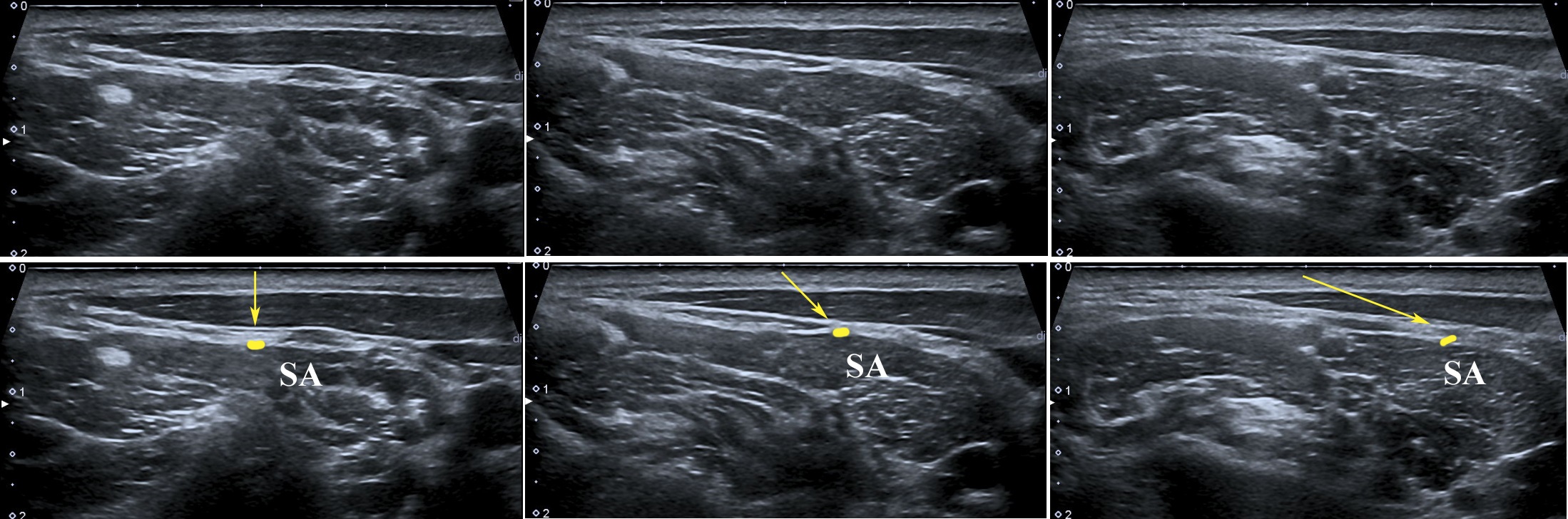
The easiest way to identify all superficial nerves is to look for 'Erb's point' (punctum nervosum).
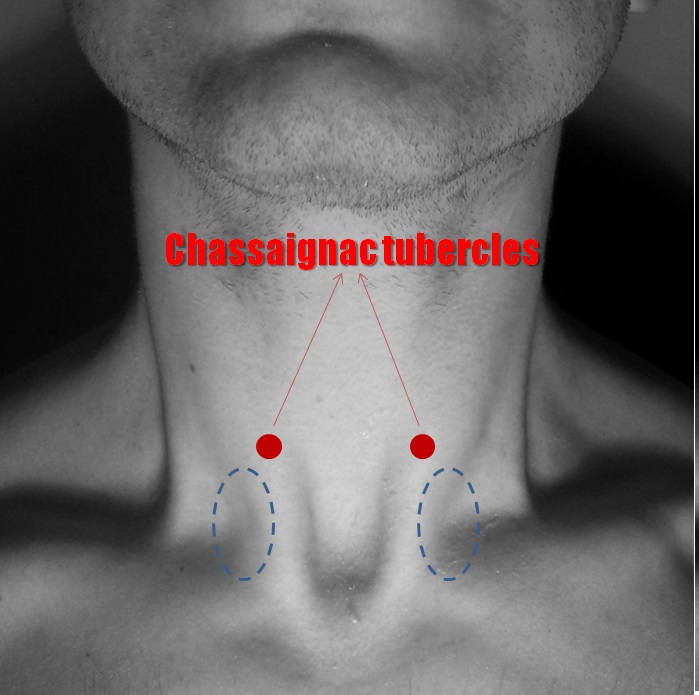
This is usually located in the middle of the posterior edge of the sternocleidomastoid muscle (approximately at the level of the C3 vertebra).
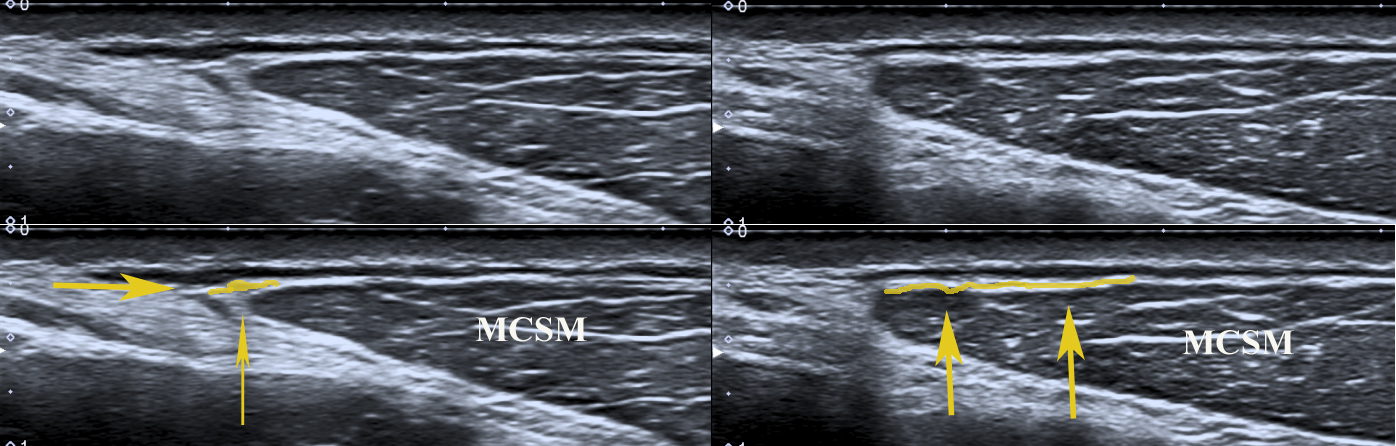
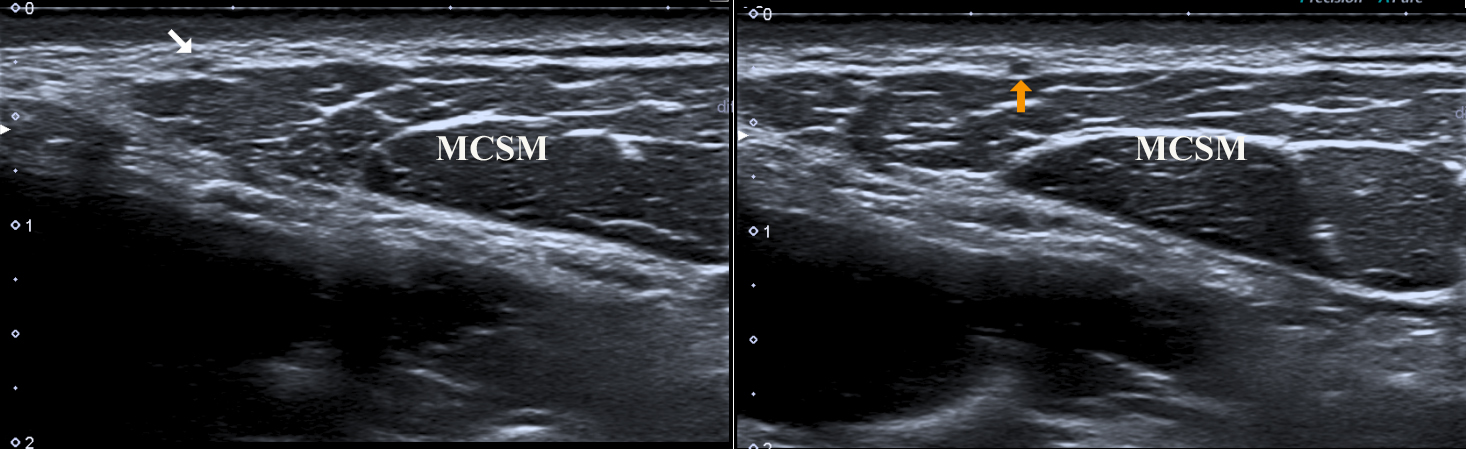
Tricks and Tips: Erb's Point is difficult to find, but there is an easy way to locate it. The probe should be placed in the short axis of the upper part of the MSM.
When using the 'elevation technique', the greater auricular nerve is clearly visible on the lateral side of the MSM. Moving downward with the nerve, one finds the punctum nervosum (Figure 17).

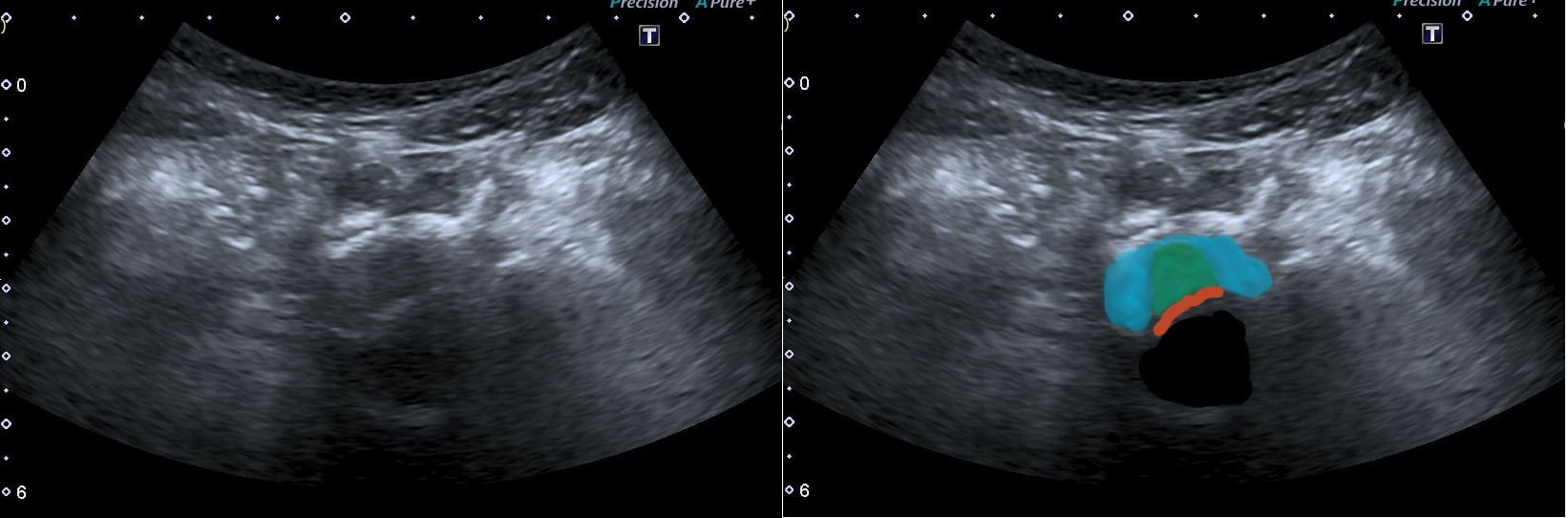
Stellate ganglion
In about 80 % of the population, the inferior cervical ganglion fuses with the first thoracic ganglion to form the stellate ganglion, which is also known as the cervicothoracic ganglion.
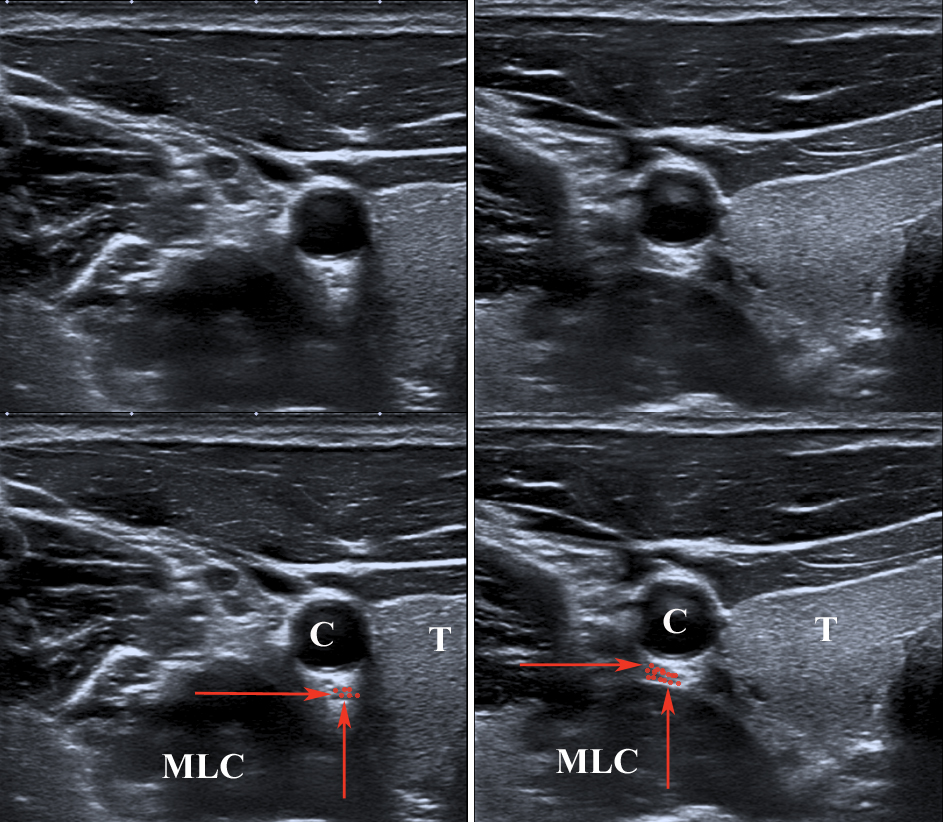
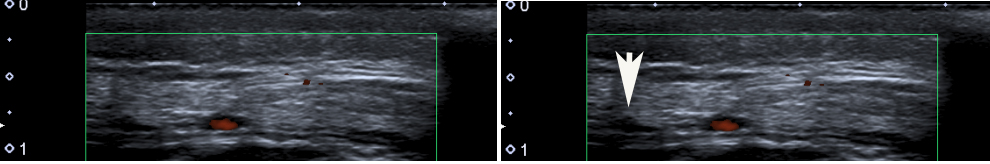
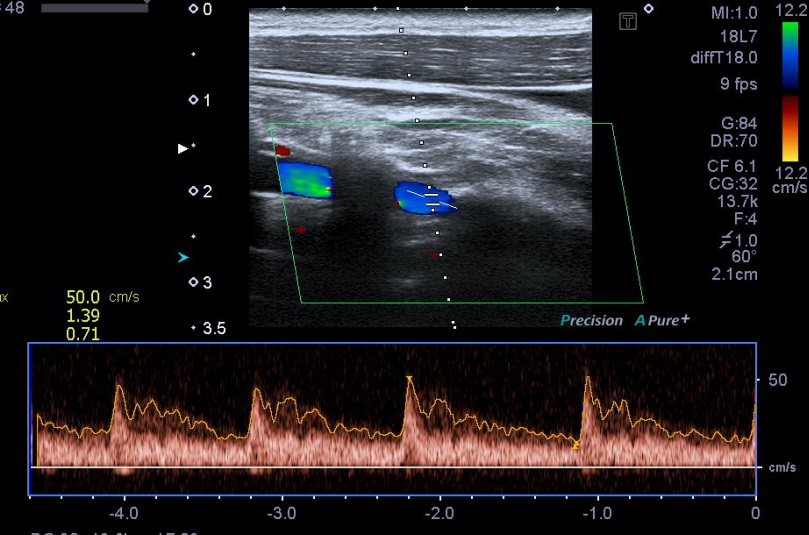
Vertebral artery: The examination algorithm is typical for this artery. The following segments should be examined: V0, V1 and V2.
After the classic medical examination, the patient's head should be turned to the side and all examinations should be repeated.
This procedure is used to rule out Bowhunter syndrome (rotational occlusion of the vertebral artery).
Muscles should be assessed in relation to the subclavian vessels and brachial plexus, as there are many anatomical variations in this area.
The most important variants are the accessory muscles (M. albinus, M. clavicularis levator) and the intramuscular course of one or more nerve roots.
Fibromyalgia: Although fibromyalgia does not have any specific ultrasound symptoms, we can press on 'trigger points' with the probe.
Pain (particularly severe) or a 'jumping symptom' that occurs after pressure on the trigger points is a clear indication of fibromyalgia.
X-ray
The X-ray examination allows you to visualize the dense anatomical structures of your bones. This is the main method for diagnosing fractures of the elbow joint.
Depending on your symptoms and the symptoms found during the physical examination, the doctor may recommend an x-ray of the arm, forearm, shoulder joint, wrist and/or hand.
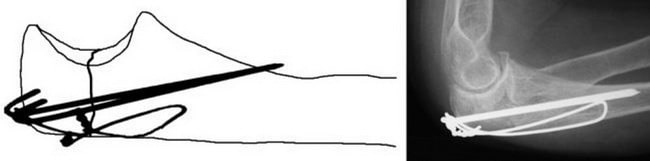
X-ray image of the elbow joint in a lateral view showing an elbow fracture with displacement
In the emergency room, the doctor will apply a temporary splint (or cast) and immobilize the arm in a sling. Initial treatment may include:
The doctor will then decide whether surgical treatment is necessary. Not all elbow fractures require surgical treatment.
If the fragments have not moved, the doctor will immobilize the elbow joint to immobilize the fragments until they heal. After this time, the doctor will repeat the X-ray examination several times to ensure that there is no displacement of the fragments.
Immobilization of the elbow joint usually takes 6 weeks, and only then does the joint begin to move again. If dislocation of the fragments occurs during this time, surgical treatment may be offered.
(Left) The elbow joint is immobilized with a splint from the upper third of the shoulder to the wrist. (To the right) The splint is fixed to the arm with an elastic bandage.
In some cases, elbow fracture surgery is indicated:
Surgery is usually intended to correct dislocated fragments and ensure that they do not move until healed.
Surgical treatment options.
Open reduction and internal fixation. This is the most common method of treating elbow fractures. During this operation, the bone fragments are joined together and fixed in their normal position with screws, wires, pins or metal plates.
Some of the most common methods for fixing the elbow process are presented below.
Immobilization of the elbow process fracture with spokes and wire loops
(Left) To fix an elbow process fracture, a single screw can be inserted into the metacarpal canal. (To the right) Immobilization of the fracture with a plate and screws.
Bone grafting. In open fractures, some bone fragments may be lost or severely shattered. In such cases, bone grafting is required to fill the bone defects. Donor bone or the patient's own bone (usually from the pelvic bone) can be used as the plastic material. In some cases, artificial bone replacement material may also be used.
Removal of a bone fragment. If the bone fragment is too small to be repaired, it sometimes needs to be removed. The tendon of the triceps muscle, attached to the fragment, is then attached to the rest of the elbow bone.
Symptoms, diagnosis
The diagnosis is made on the basis of the characteristic symptoms and the clinical picture. If necessary, additional examinations are carried out. For example, if there is a bruise, an X-ray is required to rule out a fracture of the styloid process.
Pain is the main symptom. It occurs in the wrist on the radial side (thumb side). This pain can be acute (e.g. as a result of trauma) or progressive (as a result of chronic overuse). Pain when moving the wrist or thumb is characteristic. Pain at rest is much less common and can occur with very severe inflammation or with chronic, long-term illnesses.
As a rule, no changes can be detected on external examination. In rare cases, a slight swelling may be seen above the styloid process. There is practically no redness of the skin.
Palpation of the styloid process is painful. Movement of the wrist and/or thumb is moderately painful.
There are several tests to diagnose radial styloiditis.
Hand extension test
The patient places his hands on a table and moves them to one side and vice versa. Restricted movement and pain are noted at the elbow (on the side of the little finger).
The local symptoms of styloid ulnar osteitis are similar to those of an injury to the radial bone. One difference is that the pain in ulnar styloiditis extends to the 4th and 5th nerves. This is due to the entrapment of the ulnar nerve in the inflamed tissues. There is also a difference in diagnostic tests.
Finger and Finkenstein tests are not performed for this disease. During the hand reversal test, the pain and limitation of movement occur on the radial side (thumb side).
Surgical treatment of fracture of the elbow process
Fractures of the spinous process with displacement are treated surgically – osteosynthesis (insertion and fixation of the fragments in their correct position). Depending on the severity of the fracture, there are different methods of immobilization - plate, screws or needle and wire (so-called Weber immobilization). If they don't bother you, they don't need to be removed; if they bother you, they can be removed after a year. Metal holders on the forearm generally do not respond to metal detectors. NCC No. 2 (RAS CCB) uses titanium plates, medical steel spokes and steel wire. These metals are inert, do not react, do not cause allergic reactions, and are designed to remain in the body permanently. In our clinic we use metal structures from leading western manufacturers from Germany, Switzerland, France and the USA.
Elbow fractures take an average of 6-8 weeks to heal. Follow-up radiographs will be performed 1 and 2 months after surgery. When treating elbow fractures, it is necessary not only to perform the exercises recommended by the doctor, but also to participate in physiotherapy to improve the function of the elbow joint.
Immobilization of the elbow joint with screws
In the case of a slight sprain, the elbow joint is usually fixed with screws through small punctures in the skin. A plaster splint is usually not used. The stitches are removed on an outpatient basis after 2 weeks. Since this is an intra-articular fracture, work on the elbow joint should begin on the second day after immobilization, but only with exercises that the doctor orders. This is to ensure that the joint does not stagnate, does not become stiff (contracture) and that maximum freedom of movement is restored.
Follow-up examinations are carried out 1 and 2 months after the operation, and in some cases more often if the doctor recommends it.
- Fracture of the lateral condyle.
- tibia and fibula.
- Rupture of the radial-clavicular joint.
- How much does a rib removal cost?.
- Diagram of a joint with and without a dislocation.
- Anatomy of the foot x-ray.
- Complete separation of the articular ends of the bones.
- dislocation of the foot.