This arch forms the upper part of the foot.

- The fins of the foot: recognition and correction of transverse flatfoot.
- Why does transverse flatfoot occur?
- causes
- symptoms
- The human foot – the pinnacle of evolution
- Headache from feet
- diagnostic methods
- Treatment options for metatarsalgia
- Clinically Relevant Anatomy
- characteristics
- Flatfoot treatment
- prevention
- Drawing the feet
- Adding details.
- Toes:
- Profile view:
- Symptoms of pes cavus
- How is the diagnosis made?
- Flat feet: types, risk factors, symptoms, prevention
- When should you see a doctor immediately?
The fins of the foot: recognition and correction of transverse flatfoot.
The arch and the arch of the foot cushion and distribute the load on the foot like springs when walking. In AS, the metatarsal bones become detached and the foot feels like a goosefoot. This causes the transverse arch of the foot to 'bend'. We will try to find out what side effects this can have on the foot and how you can live with it. Try it!
In transverse flatfoot, the metatarsal bones pull apart and the forefoot widens. This causes the foot to rely on the second, third and fourth metatarsals rather than the first and fifth as it normally should. While previously the heads of the 2nd, 3rd and 4th metatarsals were relaxed, with flat feet they begin to bear the full load. As a result, due to the inefficiency of the muscles, the thumb moves to the side and the joints fuse together and become a 'lump'. This results in a valgus deformity of the big toe or, as it was once said, an 'ankle' of the foot.

Why does transverse flatfoot occur?
Transverse flatfoot can occur for various reasons - either hereditary or acquired. The most important of these are described below.
- Genetically conditioned. Genetic weakness of the musculoskeletal system is most often inherited in women. Hereditary flatfoot occurs less frequently in men. So women are at risk!
– Unsuitable footwear. If you do not want to develop or worsen transverse flatfoot, you should avoid wearing shoes with high heels, narrow toes, or stiff, inflexible soles. Instead, choose comfortable shoes with a low heel. Also tidy up your shoe closet: replace shoes with uneven soles, as they keep your feet in the 'wrong' position and slow down their recovery.
- muscle weakness. Weakened metatarsal muscles – caused by a passive lifestyle and sedentary work. Keep moving!!! Then your leg muscles will become stronger and more resilient.
– Excessive weight. Excess weight puts too much strain on your legs and prevents your muscles from performing their primary function.
- Stand. Constant standing puts static strain on the legs. This leads to excess fat in the muscles and increases the risk of getting flat feet. Standing work also worsens blood flow to the legs, causing pain and tension.
– injuries. If the arch of the foot is initially normal, flat feet can develop as a result of trauma... The most common causes are a fall from a height, a car accident, or a sports injury.

causes
- Passive lifestyle;
- Uncomfortable, unsuitable footwear that loosely supports or compresses the foot;
- overweight;
- movement disorders caused by neurological diseases;
- work that requires long standing;
- osteoporosis (decreased bone density);
- Foot injuries (fractures, breaks, sprains, torn ligaments and tendons).
One of the predisposing factors is not walking barefoot. This leads to a gradual weakening of the muscles and ligaments of the foot because they are not being stimulated externally.
People with diabetes and chronic joint diseases are at higher risk of developing foot deformities.
symptoms
- Pain in the feet of various types (aching, pulling, burning);
- Increasing pain in the heel area when walking;
- burning in the calf and foot muscles;
- feeling of heaviness in the legs;
- swelling of the feet and ankles;
- Calluses and corns on the little toes and the toe bones of the big toe;
- pain when standing on toes;
- Difficulty choosing comfortable footwear.
There is also a visible flattening of the foot. In women, pain is noted when wearing high-heeled shoes.
These symptoms are similar to those of varicose veins. It is therefore advisable to see not only an orthopedist, but also a surgeon.
The human foot – the pinnacle of evolution
The human foot is an extremely complex machine, shaped over hundreds of thousands of years by natural selection and the struggle for survival, according to Charles Darwin. No animal is known to have a springy arch. Even hopping kangaroos and jerboas get by without it. According to biologists, the appearance of the arch of the foot in humans is directly related to walking on two legs. The more a primitive ancestor stood up, the more noticeable the indentation in his foot became.
Our distant ancestor, the great ape, moved on completely flat feet. Pitecanthropes and australopithecines also did not have a pronounced arched foot. The foot of Cro-Magnon man, on the other hand, did not differ significantly from that of modern man. Recently, archaeologists in southern Italy found footprints sealed in volcanic rock that are approximately 323,000-383,000 years old. Scientist Chris Stinger, who heads the Department of Human Origins at the Natural History Museum in London, suspects that the footprints come from the first Neanderthals. The same primitive people who lived somewhere between the Pithecanthropus and the Cro-Magnon people. The middle part of some of the footprints found was significantly tapered, suggesting that the early Neanderthals were the first to develop an arch. After our ancestor finally got a concave foot, his life on two feet became much more comfortable. The arch of the foot bulges when walking and absorbs shocks and stress.
Headache from feet
The average modern person takes about ten thousand steps per day. And each time the human foot experiences a shock load of 18-20 g. Considering that a spaceship takes off at an acceleration of 10 g, you can imagine how hard it is on our feet. And also for the rest of the body. Without the springy properties of the arch of the foot, we would risk a concussion with every step, and running and jumping could easily lead to death.
Scientists have calculated that the arch structure of the foot absorbs 70 % of overloads. Consequently, only 6-7 g act on the lower leg. Of course, the spine, knee and hip joints can also absorb the acceleration of the impact, but to a lesser extent. When all shock absorbers work normally, the sensitive brain reaches a relatively moderate 0.5-1g.
However, when one has flat feet, the body is in an extreme situation when walking, similar to driving a chariot with iron wheels on cobblestones. The shock wave, not dampened by the arch of the foot, immediately propagates upward through the skeleton. The joints, the spine and the brain are hit. The joints in the legs begin to wear out more quickly. The spine deforms to create an additional spring to protect the brain. And the brain itself, fatigued by the excessive shock, responds with constant headaches. The affected person feels broken, but doesn't even realize that the cause of his discomfort is flat feet. It seems like such a small thing, a little foot that curves inward.
We suspect that many people who suffer from headaches of unknown cause have them in addition to their flat feet. The great Julius Caesar, the ailing philosopher Friedrich Nietzsche, the founder of communism Karl Marx and even Charles Darwin himself could be among them. However, in their time, no one recognized flat feet as a disease, so today it is not possible to confirm or refute this assumption.
diagnostic methods
A high-quality diagnosis is a prerequisite for correct and effective treatment. Diagnostic measures help to understand what caused the pain and how to treat it.
If you suffer from metatarsal pain and don't know which doctor to see, you should first consult your family doctor, who can refer you to a specialist after an examination.
Diagnosing the cause of metatarsal pain involves several steps. The first step is an initial medical examination. The doctor draws attention to important points:

Many doctors also ask the patient to leave during the visit. During this visit, the nature of the gait can be assessed and even (not always, but in some cases) a preliminary diagnosis can be made.
After the initial examination, the patient is always referred for instrumental examinations. With their help, the clinical picture can be analyzed in more detail and the condition of the tissues and bones of the foot can be examined from the inside. The list of commonly performed instrumental examinations includes:
- X-rays. In this procedure, images of the foot are taken in two projections. The images can be used to determine whether bone and joint deformations are present and how severe they are.




Treatment options for metatarsalgia
Depending on the exact cause of the pain in the arch of the foot, the patient is referred to a specialist. If the symptom is due to trauma, it will be treated by a trauma surgeon; if it is due to arthritis or other musculoskeletal disorders, it can be treated by a rheumatologist; if it is due to a neurological disorder, it can be treated by a neurologist. In some cases, more than one doctor may be needed at the same time. The type of treatment also depends directly on the type of impairment. She can be:
- physiotherapy. It is prescribed for conditions that are not very serious and do not require major medical or surgical treatment.



In addition to the basic treatment, supportive therapies are also used. This includes wearing special orthopedic shoes and orthoses.
To relieve pain, improve blood circulation and metabolism, and correct curvature, doctors recommend walking barefoot on grass and sand. This treatment is effective for both the complementary treatment of pain and its prevention.

Clinically Relevant Anatomy
Clinically, hollow foot is characterized by an abnormally high longitudinal arch. From a biomechanical perspective, hollow foot is formed by an inwardly turned toe, a high heel angle, a high metatarsal, and plantar flexion of the toes.
When the talar angle is reduced, the heel bone is no longer in the middle, but at the top of the ankle. This impairs the function of the Schopar joint. The scaphoid connects the foot to the ankle. A healthy foot revolves around the scaphoid; The rectus femoris, on the other hand, always moves at the same time as the heel bone.
characteristics
During the support phase of the gait cycle, the heel is in an inverted position and the toe is in a varus position, resulting in poor load distribution throughout the foot. This can lead to metatarsalgia, first metatarsal stress fractures, plantar fasciitis, medial longitudinal arch pain, iliotibial tunnel syndrome, and balance problems.
In cavus foot syndrome, the heel bone rotates inward under the ankle bone, resulting in a small talofemoral angle. Since the calcaneus follows the talus bone, the latter is in a plantar position relative to the navicular bone rather than adjacent to it. This position causes locking of the metatarsal bones and overloading of the lateral side of the foot.
The mobility of the foot can be assessed differently by looking at the foot from the front and mentally drawing a straight line along the foot through the Lisfranc and Chopar joints. The parallelism of this straight surface is a prerequisite for the free flexion of the foot. The larger the angle between the straight line and the surface, the more limited the mobility of the foot is. With very high longitudinal arches, the load is distributed unevenly across the heads of the metatarsal bones and the lateral edge of the foot. This can lead to pronation of the foot and damage to the heel bone due to excessive pressure and the formation of osteophytes at the junction of the metatarsal and talus bones.
Flatfoot treatment
Effective treatment of flat feet is only possible in childhood, when the bones and ligaments are not yet fully formed. Later, doctors can only slow down the deformation process, relieve those affected of pain and prevent complications from developing. This is done by:
- Hand massage of the feet and lower legs: This contributes to improving blood circulation, strengthening the ligaments and musculoskeletal system;
- Massage with a special mat or electric massager;
- Therapeutic exercises: walking on heels and toes, bending and straightening the toes, lifting objects from the floor with the feet, rolling objects; it is recommended to do these exercises daily;
- Physiotherapy: magnetic therapy, phonophoresis, electrophoresis to stimulate muscles, improve blood circulation and effectively administer medications;
- Medication: Pain relief with analgesics, pain-relieving ointments (as prescribed by a doctor);
- Wearing orthopedic shoes: Special shoes or insoles for the usual models help to redistribute the load on the foot and relieve pain; in children they support the correct formation of the arch of the foot;
- Surgical treatment: the only way to cure adults with flat feet.
prevention

Director, chief physician, orthopedist and traumatologist
The most effective way to prevent flat feet is to wear appropriate footwear. It must be true to size, made of high-quality leather and have a flexible sole. Heel height for an adult: 4 cm, for a child: 0.5 cm.
- to avoid foot injuries;
- lead an active lifestyle with moderate physical activity (no competitive sports!);
- Use massage mats, walk barefoot on sand, grass, pebbles;
- Avoid excessive body weight.
Drawing the feet
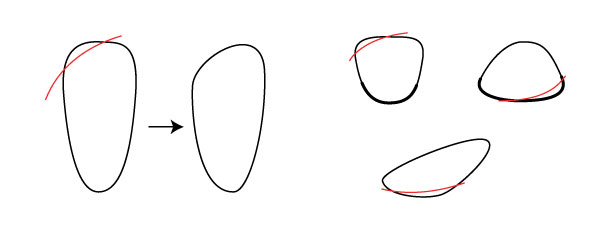
An easy way to depict the feet is to start by drawing the sole of the foot. No toes or arches, just the basic shape. The foot is shaped like a long egg, flattened on one side.
The advantage of this is that this shape is simple enough to be shown in perspective and from different angles. This part of the foot bends almost imperceptibly, so it is not necessary to bend it. Anatomical precision is not required here, just a guide for further work.

If you have trouble with perspective, draw a basic shape on a piece of paper and place that piece of paper at the correct angle. This is also a useful exercise to familiarize yourself with how this shape changes at different angles.
The next step is to make small adjustments to the shape and trim the angle so that the foot is closer to its natural shape. If this is more convenient for you, you can start with this step:
Now let's put them in three-dimensional space. As you can see, they are flat, curved pyramids with the tip near the heel: a circle where the foot and leg come together to form the ankle. I drew dotted lines to make the contours easier to see. Only black lines are needed for the drawing.
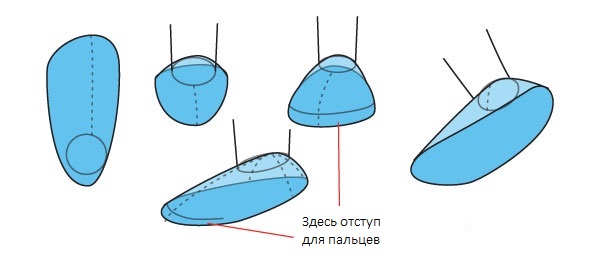
Now let's move on to the toes. Drawing them separately helps to depict the movement of the fingers independently of the main shape, which, as written above, is almost stationary. If necessary, make a sketch to determine the general shape of the fingers before drawing them individually (see later). They are pressed against each other in such a way that they overlap from almost all angles. Note the position of the little toe: its base is between 1/4 and 1/3 of the total length of the foot (here the lines divide the foot by 4, i.e. 1/4).
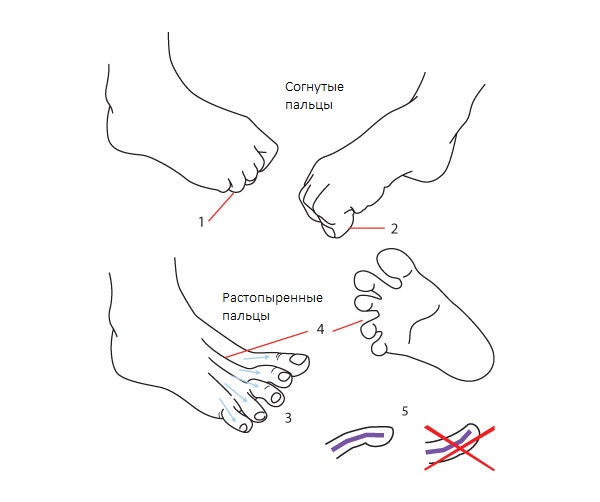
Adding details.
A few extra details to make the feet look more believable.
Toes:
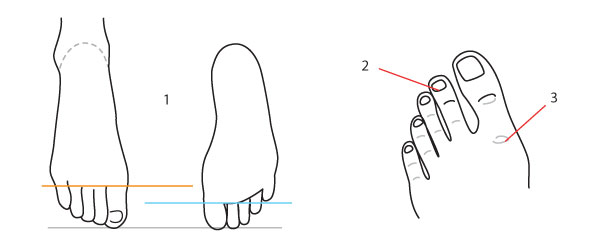
- The toes look longer at the top of the foot than at the bottom. The longer the toes, the wider the nails.
- Also note that the big toe is much larger than the ring toe. His first joint is in the foot and is difficult to move.
What the toes look like when the foot is flexed depends on how much weight it is supporting:
Foot A bottom of the picture is relaxed. Even if the toes are slightly bent, there is no real weight pressure on them. In this situation they retain their slight curvature towards the ground (1).
Pictured. bIn this situation, most of the weight rests on the toes (note: this is only possible on the ground, this is not possible in the air). Under pressure, the second joint bends as shown (2). Bend the links at the other joints (3). The thumb is then even straighter and presses completely onto the floor.
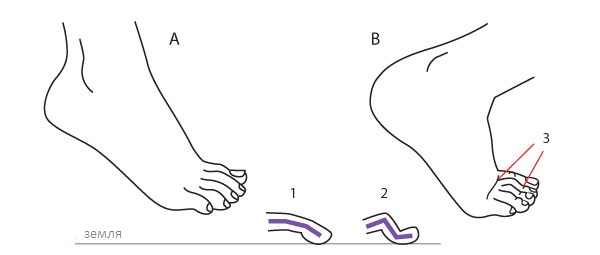
When the fingers are not pressed against the floor, their range of motion is limited to two extremes: retracted and extended.
- The first joint of the fingers can disappear completely under the foot….
- ...except for the thumb, which is at a 90º angle.
- When the toes are spread too far, they point in different directions...
- The tendons are visible, as is the space between the toes.
- Note that all fingers (except the thumb) remain curved downward, they are never curved upward.
Profile view:
1) There is always a tubercle that is more or less visible.
2. the protruding ankle bone is higher on the inside.
3. At least two fingers can be seen behind the big toe, this depends on the viewing angle.
Symptoms of pes cavus
Those affected complain of a changed gait and poor resilience, especially when walking for long periods of time. An unpleasant pain occurs in the lower part of the foot. The symptoms often extend to the ankle joint. The elevated position of the foot makes it difficult to choose footwear and insoles. The normal position of the shoe does not provide comfort as it is too low and too tight for the patient. The forefoot arch is another characteristic external symptom.
Other clinical signs and symptoms:
- Limited mobility of the lower limbs
- Persistent swellings, calluses, corns
- Weakening of the leg muscles
- Weakened tendon reflexes
Other symptoms depend on the cause of the deformity.
How is the diagnosis made?
The doctor examines the lower extremity, assesses the nature of the abnormal structure and determines the severity of the movement disorder. A plantogram is created. Other symptoms and risk factors are looked for to identify the underlying disease. Previous trauma, malignant tumors, congenital syndromes and other pathologies must be excluded. A diagnosis can only be made after definitive tests are performed.
Additional diagnostic procedures:
X-rays. X-rays show the position of the bones and previous traumatic influences.
Computed tomography or magnetic resonance imaging. The scans provide the doctor with high-resolution slice images of various anatomical structures.
MRI is a more precise and modern imaging method without the disadvantage of radiation exposure. The detailed images allow the doctor to find the cause of abnormalities in the skeletal system. The specialists at CMRT clinics detect hollow feet using this type of examination.
Flat feet: types, risk factors, symptoms, prevention
A distinction is made between transverse and longitudinal flatfoot. In transverse flatfoot, the transverse arch of the foot is flattened and the forefoot rests on the heads of all five metatarsals, not just the 1st and 5th. In longitudinal flatfoot, the longitudinal arch is flattened and the entire surface of the sole of the foot is in contact with the ground. The main cause of flat feet is muscle and ligament weakness caused by trauma or an occupational disease (in people whose jobs require long periods of standing or walking). Flat feet are more common in overweight people than in people of average body weight. Many people's feet also become flatter and longer in the evening (due to muscle fatigue).
Flat feet manifest themselves as pain in the foot area and rapid fatigue in the legs. The pain can also occur in the shin and thigh area and be accompanied by deformation of the toes. In children, flat feet can develop due to frequent physical exertion: carrying heavy objects, the habit of lifting younger siblings, etc.
Prevention of flat feet consists in strengthening the muscles of the foot and lower limbs through special exercises (for example, walking on the toes and the outer edge of the foot), creating an environment that prevents prolonged contact with the feet , and to use special insoles to raise the arch of the foot.
Occupational stress on the foot leads to significant changes in the foot. An example is the foot of ballet dancers. When standing and walking on tiptoes, the entire body weight rests on the first three toes, so the metatarsals and phalanges of these toes are relatively more massive than in other jobs. Although the human foot is highly specialized as a support and locomotion organ, it is used by some peoples as an auxiliary organ for work. For this reason, the joint movements of the foot are very flexible and the muscles are dexterous. If necessary, the mobility of the ankles can be increased through appropriate exercises.
When should you see a doctor immediately?
If the outside of the foot hurts, but only causes discomfort, you should consult a doctor after 2-3 days, avoiding overexertion and other unusual situations that could trigger the pain syndrome. However, if you have an injury or acute, stabbing pain without an apparent cause, you should consult a doctor immediately. If you experience a sprain or fracture, medical treatment can help prevent further damage and maintain mobility in the foot. If pain is unexplained, you should undergo a comprehensive examination to rule out degenerative processes or hidden fractures.
Read more:If your foot pain lasts longer than two days, you should definitely get checked out to rule out a number of medical conditions, otherwise you risk losing mobility in your foot and becoming disabled.
- Latin Arch.
- Which ligaments strengthen the transverse arch of the foot?.
- flat foot pronation.
- Metatarsal tarsal bones.
- Valgus flatfoot (valgus flatfoot).
- flat feet (valgus foot).
- Which doctor treats flat feet?.
- The dorsum of the foot is where.
