First and foremost, attempts should be made to eliminate the causes of the disease. In the early stages, conservative methods are used, and if these are ineffective or in later stages, surgical methods are used.

- Schlatter's disease (Osgood-Schlatter disease, osteochondropathy of the tibial tuberosity)
- Symptoms and course of the disease
- Dressings for anterior tibial syndrome[edit].
- Exercises for anterior tibial syndrome[edit].
- causes of the problem
- Types and severities of impingement syndrome
- Types of bone marrow edema:
- Edema of the trabecular bone marrow
- Edema of the femoral bone marrow
- Treatment of bone marrow edema
- Symptoms of metaphyseal dysplasia
- Janssen-type metaphyseal dysplasia
- treatment methods.
- Articles from medical experts
- Causes of lower leg pain
- Main causes of tibial neuropathy
- Symptoms of tibial neuropathy
- Peripheral vascular occlusions
- Blockages of the blood supply vessels to the brain
Schlatter's disease (Osgood-Schlatter disease, osteochondropathy of the tibial tuberosity)
Schlatter's disease is an inflammatory disease that is associated with bone necrosis. It most commonly occurs on one leg, but can also occur on both legs.
It usually occurs in children and adolescents between the ages of ten and eighteen, when the bones are in their strongest growth phase. It is much more common in boys. The disease often develops without a clear cause (in some cases it can be linked to bruising and trauma).
The following factors are often responsible for the development of the disease:
- direct injuries: fractures and dislocations of the kneecap or shinbone, damage to the knee joint;
- permanent micro-injuries to the knee related to sports activities.
According to medical statistics, Schlatter-Osgood disease affects about 20 % of young people who actively play sports and only 5 % of those who do not play sports.
Children who participate in the following sports belong to the risk group
- basketball
- volleyball
- Hockey;
- Football;
- Do gymnastics;
- Acrobatics;
- Figure skating;
- Ballet;
- wrestling;
- Weightlifting.
As a result of overloading, constant microtraumatization of the knee and overstretching of the patellar ligaments that occurs when the quadriceps is contracted, blood flow to the tibia, more precisely to the tibial tuberosity, is impaired. Small hemorrhages, rupture of the patellar ligament fibers, aseptic capsulitis, and necrotic lesions of the tibial tuberosity occur.
Symptoms and course of the disease
Schlatter's disease is characterized by a gradual, asymptomatic onset. Patients usually do not attribute the onset to a knee injury.
The main symptoms of Osgood-Schlatter disease include.
- Swelling and pain in the area of the tibial tuberosity, directly under the patella;
- Pain in the knees that increases after physical activity - especially running, jumping and climbing stairs - and decreases with rest;
- Tension in the surrounding muscles, especially the thigh muscles (quadriceps).
The pain varies from person to person. Some people only experience mild pain during certain activities, especially running or jumping. For others, the pain can be constant and debilitating. Osgood-Schlatter disease usually develops in only one knee, but sometimes both knees can be affected. The symptoms can last from a few weeks to several months and can recur until the child stops growing.
When examining the knee, swelling of the knee is noted, which flattens the contours of the tibial tuberosity. Palpation of the nodule reveals local tenderness and swelling that is firm elastic in consistency. A hard bulge can be felt through the swelling.
Schlatter's disease has a chronic course, sometimes with fluctuating progression and pronounced phases of exacerbation. The disease lasts one to two years and often results in the patient recovering after bone growth has completed (around age 17-19).
Complications of Osgood-Schlatter disease are rare. This can include chronic pain or local swelling, which can be well treated with cold compresses and anti-inflammatory medications. Often, even after the symptoms have subsided, a nodule can remain on the lower leg at the site of the swelling. This nodule can persist to varying degrees throughout life, but usually does not affect the function of the knee.
Dressings for anterior tibial syndrome[edit].
There are many methods for treating lower leg pain, between which the choice usually has to be made empirically. If the pain is caused by flattening of the longitudinal arch of the foot, a simple bandage on the arch of the foot in combination with 2-3 circular bands applied to the distal part of the tibia to reduce extension may be helpful to the athlete (Fig. 2.23 ). A closed braided bandage to limit pronation of the foot helps with inflammation of the tendon of the tibialis posterior muscle. Athletes also note the great effect of compression bandages on the lower leg (Fig. 2.24). Bandages do not help with anterior tibial fascia bed syndrome or stress fractures.

Figure 2.23. Bandage for anterior shin syndrome, which is caused by a flattening of the longitudinal arch of the foot. This is a combination of a simple bandage on the arch of the foot and a bandage that relieves pressure on the bunions.
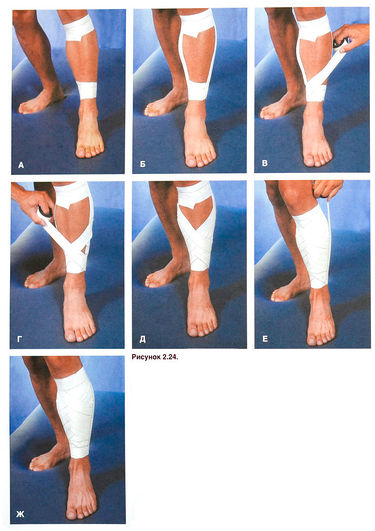
Figure 2.24. Bandage on the anterior surface of the tibia in tibialis anterior syndrome. First place the proximal and distal (А)as well as medial and lateral (Б) Anchoring strips. The tape strips are then applied diagonally: from the medial to the lateral side (В) and from the lateral to the medial side (Г)transversal. Once the front surface of the shinbone is completely covered (D)Attach the fixation straps on the medial and lateral sides (F). (Ж).
Exercises for anterior tibial syndrome[edit].
Exercises to stretch and strengthen the muscles that affect the ankle joint (see Figures 2.8 and 2.9), as well as exercises for the longitudinal arch of the foot (see Stretching the Muscles and Ligaments of the Foot), are helpful. The athlete should strengthen the front and back muscle groups of the lower leg equally and use good footwear.

Figure 2.8 А. Stretching the calf muscle with a towel. The athlete should place the foot in a dorsal position and then pull on the ends of the towel to stretch the muscle. During the stretch, the neutral position of the foot should alternate with supination (Б) and pronation (В). To stretch the cambium muscles, repeat the exercise with the leg bent at the knee and hanging over the edge of the table. Г. D. You can stretch the lower leg muscles without additional aids by changing the plantar flexion position of the foot.
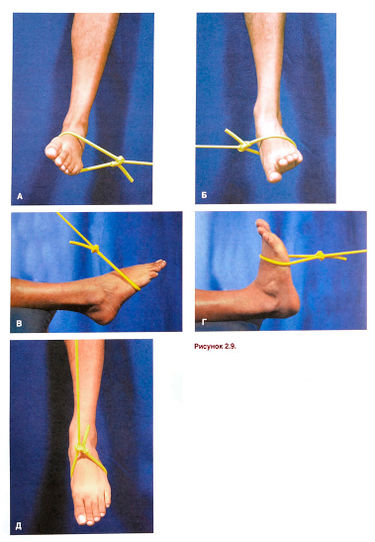
Figure 2.9. Exercises to strengthen the lower leg muscles with an elastic band. A. Supination of the foot. B. Pronation of the foot. В. Flexion of the sole of the foot. Г. D. Dorsiflexion of the foot. D. To strengthen the hamstring muscles in isolation, plantar flexion of the foot is repeated by bending the leg through 90° at the knee joint.
Orthotics are shoe inserts designed to restore proper biomechanics to the foot.
causes of the problem
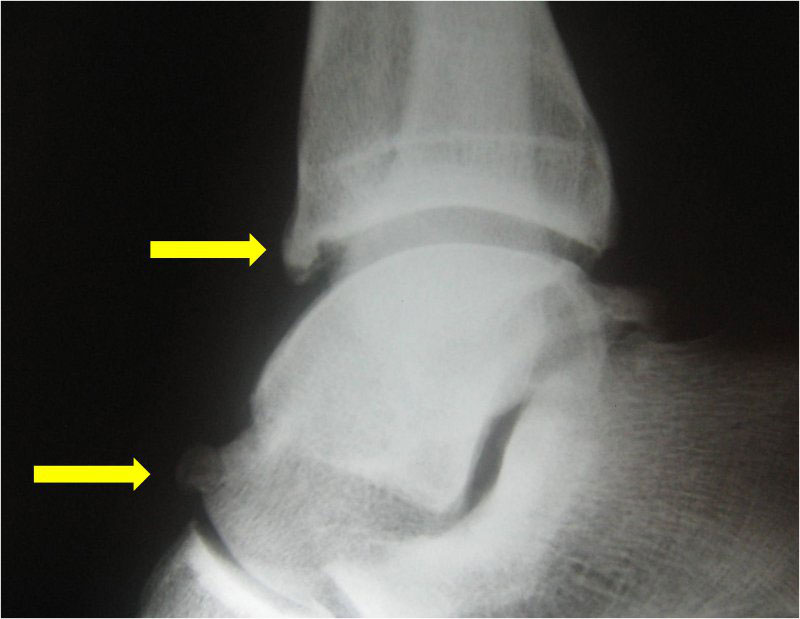
The inclination of the joint capsule, together with the synovial membrane in the area of the ankle joint, causes impingement. Osteophytes (also known as bone cones) begin to grow in the areas of compression and an active inflammatory process develops.
The presence of osteophytes further reduces the natural distance between the talus and tibia bones. As a result, the joint capsule and synovial membrane become even more compromised, inflammation increases, and pain increases.
There are three main causes that contribute to the development of this condition:
- Patients with a congenital predisposition;
- ankle injuries sustained or inadequately treated;
- Chronic inflammation caused by other factors.
Each of these factors can contribute to negative changes in the joint. This results in symptoms of illness and significant discomfort.
Types and severities of impingement syndrome
There are two main types of impingement syndrome: anterior and posterior.
Anterior impingement is primarily caused by traumatic damage to the ligaments of the ankle joint. Any instability of this joint, no matter how slight, contributes to its injury in extreme extension.
Statistically speaking, anterior impingement primarily affects athletes. Anterior impingement is caused by frequent heavy loading of the anterior joint and results in permanent damage to the joint. Overstretching of the joint is the main cause of impingement.

Posterior impingement is often related to the anatomy of the ankle joint and trauma. Posterior impingement is particularly characteristic of ballet dancers. Because in this dance you have to walk a lot on your toes, which leads to a strong backward bending of the ankle and the resulting trauma.
The presence of posterior impingement is often forgotten, although this condition can actually lead to severe impairment of joint function.
The disease can also be divided into several degrees:
- Grade I – characterized by the presence of a spur up to 3 mm in size on the tibia, called the synovial stage;
- Grade II – osteochondral, the size of the spur exceeds 3 mm;
- Grade III – exostoses with or without fragmentation can be found, and the spur also appears on the talus;
- Grade IV – changes that are characteristic of osteoarthritis develop.

Types of bone marrow edema:
The types of bone marrow edema can be distinguished based on several characteristics. The measures chosen to combat this pathology and its consequences depend on this.
Edema of the trabecular bone marrow
Swelling of the trabecular bone marrow is the first sign of a vertebral fracture. This is particularly possible if the height of the vertebral body is reduced due to a fracture. If there is only swelling, the presence of a bruise or a vertebral fracture is questionable. Diagnostic procedures such as X-rays or CT scans best show the situation in this case, and the MRI procedure is helpful as a complementary method. This is because soft tissue pathology is diagnosed by MRI.
With trabecular edema, there should be an increase in the volume of fluid in the bone tissue, which is not only a traumatic genesis, but also an inflammatory process. The treatment would be potassium iodide, which has an anti-inflammatory effect. As long as the protrusion is small, it should be treated regardless of its location. In addition to medications and physical therapy, acupuncture and physical therapy are prescribed to prevent spinal bulging and the development of myelopathy.
Edema of the femoral bone marrow
Edema in the bone marrow of the thigh can be very severe. The cause of the swelling is important. When accompanied by bone inflammation, the symptoms are very serious. It is a complex process with pus formation. It penetrates the bone and bone marrow, where malignant bacteria also spread, and requires complex treatment. In this case, the swelling is a consequence of the disease itself.
Osteochondrosis and herniated discs are also side effects of the disease. They are diagnosed using magnetic resonance imaging. An accurate diagnosis can be made by a surgeon.
Such swelling may indicate abnormalities related to a bony prominence in the femur. In this case, this bone is considered part of the knee, and if there is dysfunction, one should be concerned about whether the patient has bone marrow edema on this bone.
Treatment of bone marrow edema

Treatment of bone marrow edema depends on several important factors:
- the cause of the edema;
- the extent of manifestation of the pathological process;
- the nature and extent of the role and the effects of mass on joint function.
The treatment of bone marrow edema is a rather complex task. Even highly qualified specialists approach the solution with great caution. Self-treatment is out of the question.
The situation is particularly complicated by the fact that any inappropriate action is often fatal. If an exacerbation occurs, the doctor must ensure that cerebral blood flow pressure is restored. This is commonly referred to as CPC. This ensures normal blood flow and a normal supply of substances to the nerve cells. The normal accompaniment of bone marrow edema is an increase in intracranial pressure followed by a sharp decrease in CPC values.
Help is sought to reduce the high pressure:
- Maintaining oxygen supply to the body.
- Treatment and prevention of pain syndromes.
- Treatment of seizures.
- Maintaining body temperature within normal limits.
- Administering diuretics to the patient to flush out excess fluid.
- Moderate hyperventilation.
- Eliminating the cause of abnormal fluid discharge.
- Normalization of spinal cord volume supported by forced diuresis with electrolyte-regulating drugs.
The water-electrolyte balance should always be monitored. When treating bone marrow edema, discontinuation of glucocorticoid therapy is important. Its function is to stabilize cell membranes. This prevents the accumulation of catecholamines in damaged cells and tissues. Membrane protectants, also known as nootropics, are ideal.
Symptoms of metaphyseal dysplasia
The disease is characterized by a severe displacement of the long bones with a simultaneous significant enlargement of the Erlenmeyer hump in the legs. Symptoms are particularly pronounced when the thigh bone is affected. In metaphyseal dysplasia, the negative changes in the structure of the skull are minimal. In rare cases, the frontal lobes protrude significantly beyond the eye sockets, creating an asymmetrical facial structure.
Dysplasia involves an enlargement of the chest, an abnormal pelvis with curvature and changes in the hip joint. The angle of the lower jaw is changed and the upper arm bones are also wider than normal.
Many patients have a severe curvature of the spine and severe forms of scoliosis. Even in childhood, bone density is much lower than normal, which leads to osteoporosis. The bones become too brittle and can hardly support the weight of the body when walking and during active movements. This is the main cause of frequent pathological fractures of the ribs and lower limbs.
The symptoms of metaphyseal dysplasia are also common:
- Severe forms of dental caries with multiple dental lesions in the neck region;
- Abnormal structure of the paranasal sinuses, frontal sinuses;
- Restriction of mobility of the upper limbs in the elbow region;
- Significant muscle weakness;
- hypotonia of the lower limbs;
- malocclusion;
- flat feet.
In some forms, scoliosis progresses quickly. The nerve endings in the spinal cord that supply internal organs are compressed. This is one of the causes of cardiovascular and endocrine problems, digestive organs, headaches and muscle pain.

Janssen-type metaphyseal dysplasia
An extremely rare disease: To date, no more than 10 cases have been reliably described. The characteristic features that indicate this type of disease include:
treatment methods.
In some forms of metaphyseal dysplasia, patients suffer from a severe lack of bone mass. After determining bone density, the doctor may recommend treatment with mineralizing agents based on calcium, fluoride, magnesium and vitamin D. These do not change the structure, but reduce the risk of pathological bone fractures.
Any pharmacotherapy of metaphyseal dysplasia is supportive and is used to eliminate symptoms. In modern medicine there are no drugs that can stop pathological changes in the metaphysical parts of the bone. In Pyle's disease, hormone levels must also be monitored and corrected.
In case of frequent dislocations and subluxations of the hip joint, wearing special prostheses is recommended. Patients are individually fitted with orthopedic shoes to correct shortened limbs. A brace and ongoing physical therapy are needed to slow the progression of scoliosis. If there is no effect, surgery is indicated.

Articles from medical experts
All iLive content is reviewed by medical experts to ensure it is as accurate and factual as possible.
We have a strict policy in selecting information sources, citing only reputable websites, academic research institutes and, where possible, peer-reviewed medical studies. Please note that the numbers in parentheses ([1], [2], etc.) are interactive links to such studies.
If you think any of our material is inaccurate, out of date or otherwise questionable, please highlight it and press Ctrl + Enter.
Shin splints are a fairly complex problem for humans, as they can be a symptom of a life-threatening condition such as thrombosis. And thrombosis is not the only disease that signals lower leg pain. Sometimes such lower leg pain is associated with diseases that are still in their early stages - in this case they can be treated quickly. How do you distinguish between a dangerous situation and one that can be dealt with quickly?
Causes of lower leg pain
- There is a reduced concentration of certain salts in the blood, e.g. B. Magnesium, calcium, potassium. The cause of the reduced salt concentration can be diuretics.
- The person takes medications uncontrollably: statins (these can cause destruction or deformation of muscle tissue, thereby reducing blood cholesterol levels).
- Muscle cramps, especially during prolonged exertion, physical stress.
- Torn ligaments or tendons as a result of muscle injuries
- Fracture of a bone in the lower leg or ankle
- Deformation or damage to the meniscus
- Venous thrombosis (deep or superficial), occlusion
- tendonitis
- Damage to the meniscus.
- Atherosclerosis in the blood vessels of the legs
- Infectious tissue lesions of the lower leg
- Deformations, tears, strains, trauma, nerve fiber damage (smokers, alcoholics and diabetics are at risk).
- So-called 'trap syndrome', in which the lower extremity becomes trapped or compressed as a result of trauma or overstretching of the muscles
- Fractures resulting from excessive muscle stretching
- Muscle contractures – so-called muscle stiffness as a result of overstretching or overexertion
- Periostitis of the tibia
- Tears – large and small – in the calf muscles
- Enlarged veins, rupture of ligaments below the knee.
- Inflammation of the tibial tuberosity
- Inflammation of the tip of the kneecap - so-called jumper's knee
- Tumors of the shinbone or hip or osteomas
- Misuse of medications such as corticosteroids
- Malignant tumors of the lower jaw bones
- Paget's disease (breast cancer)
- Raynaud's Syndrome
- Muscle compression syndrome
- Compression of nerve roots in the lower leg
Main causes of tibial neuropathy
Let's look at the main situations that provoke a problem such as tibial neuropathy:
- Severe trauma - fracture of the lower extremity, dislocation of the ankle, tendon dysfunction, sprain of the ankle ligaments;
- Repeated trauma from sports training, foot deformities, which include flat foot;
- Long-term malposition of the lower limbs with severe compression (tibial nerve entrapment);
- Impaired metabolism;
- Diseases of the knee and ankle.
Symptoms of tibial neuropathy
If the disease affects the tendons, the patient has difficulty flexing the foot and cannot control the toes properly. There is an inability to stand on toes. There is complete muscle dysfunction in the lower leg, foot, and the foot takes the shape of a clawed foot.
In some cases, the problem is triggered by prolonged walking or running. The sole of the foot becomes very painful and radiates into the calf muscle. The pain increases significantly when standing and walking.
In professional runners, the median nerve is most commonly affected. The pain occurs on the inside of the sole of the foot and in the area of two or three toes.
Women who regularly walk in high heels or are overweight suffer from this condition. In this case, any movement, including running, significantly increases the painful sensations.
Calcanea affects the heel area. This condition is usually caused by unfortunate heel hopping, walking barefoot for long periods of time, or wearing thin-soled shoes. The affected person cannot step on their heels because of the burning and unbearable feeling.
Peripheral vascular occlusions
Vascular occlusions affect large arteries in the limbs, most commonly in the lower limbs. Obstructions are an unpleasant consequence of vascular diseases of the lower limbs. The danger of acute occlusion in this area is that tissue necrosis occurs, leading to amputation of the affected limb. Characteristic symptoms of obliterative thrombophlebitis, atherosclerosis of the leg vessels and other common pathologies are:
- pain in the legs that does not go away even with rest;
- Pallor of the skin on the limbs;
- feeling of cold in the legs;
- tingling and numbness in the limbs;
- Impairment of the motor function of the limbs.
If these symptoms occur, immediate examination and treatment of the blood vessels of the limbs is indicated: the slightest delay can lead to gangrene. In the early stages of the disease, obliterating atherosclerosis of the lower limbs and other sclerotic pathologies are treated conservatively, while in the advanced form it is difficult to fight the disease.
Occlusion processes occur in the renal arteries, leading to renovascular hypertension and renal dysfunction. The disease also affects the aorta, the largest vessel. Read about the effects of atherosclerosis on the aorta here.
 Blockages of the blood supply vessels to the brain
Blockages of the blood supply vessels to the brain
Blockages in the arteries that supply blood to the brain have dangerous consequences. Impaired blood flow to the brain poses a risk of stroke or cerebral ischemic infarction, often leading to patient death, paralysis or dementia. A common cause is blockage of the carotid artery. It is accompanied by loss of consciousness, nausea and vomiting, problems with coordination, speech and vision, as well as weakness and numbness of the limbs. A precursor to a stroke is the transient (cerebral) ischemic attack, which we have already discussed in detail.
In most cases, surgery is the only way to remove the blockage and restore blood flow. If the blockage is complete, an arterial bypass, an open operation in which the diseased part of the vessel is replaced with an artificial prosthesis, should be performed.
Read more:- Growing bones in the foot.
- Legs in adolescent boys.
- shin sprain.
- Child has a bump on his foot.
- Anterior tilting of the pelvis.
- Root nodules in children.
- lower leg flexion.
- Why the shin hurts.
