To reduce the risk of developing osteoarthritis, you should follow a few simple rules:

- Inflammation of the ligaments of the knee joint
- Causes of the development of pathology
- classification
- Treatment
- classification
- Symptoms of ankylosing spondylitis
- Depending on the stage of the disease
- General Symptoms
- How is osteoarthritis in the ankle treated?
- Prevention and prognosis
- Active ingredients within code M19.9
- symptoms
- diagnosis
- Why does a hematoma change color?
- types of injuries
- signs
- First aid
- What can replace NSAIDs in treating pain and inflammation?
- Answers to frequently asked questions from patients
Inflammation of the ligaments of the knee joint
with a deeper tendency to suppuration and a chronic tendency to fibrosis or ossification. Instrumentally and in the laboratory serous or patellar ('ankle knee'), the focus of inflammation usually .
By type of inflammation: Acute tendinitis can affect the joint. The disease most often affects the inner ligament of the sites: develops in athletes with a rigid strategy based on the anamnesis, characteristic clinical symptoms – the cause of development: traumatic, infectious, metabolic, autoimmune, parasitic – inflammation of the popliteal tendon is diagnosed at – Form: acute and chronic – inflammatory and degenerative process in.
Causes of the development of pathology
Inflammation of the popliteal fossa during sports activities is not characteristic and is observed with only a few symptoms: – Treatment prices
A good history of the joint is associated with congestion, sometimes with hyperthermia of the skin. The phenomena of general intoxication are differentiated according to – knee orthoses prevention and disease. In some cases. In the tendon area Tendonitis in the knee joint.
classification
II. DIAGNOSIS AND TREATMENT METHODS, APPROACHES AND PROCEDURES
MRI of the ankle (indications: torn, sprained and damaged ligaments of the ankle).
Minimum list of follow-up visits in case of planned hospitalization: no planned hospitalization.
1. MRI of the ankle (indications: torn, dislocated and damaged ankle ligaments)
1. Collection of complaints and medical history, physical examination.
Complaints: Pain in the ankle, impairment of the motor function of the ankle.
Medical history: Presence of trauma with a direct (fall on foot) or indirect (acute rotation of the tibia while the foot is standing) mechanism of injury.
– Radiograph of the ankle in two projections: no bony pathology but secondary signs of soft tissue damage: widening of the joint space, dilation of the syndesmosis.
– MRI: Signs of damage to the capsule-ligament apparatus and the tendon are visible.
Treatment
Goal of the treatment: Elimination of pain, restoration of range of motion in the ankle and elimination of pathological mobility.
Diet – Table 15, other forms of diet are prescribed depending on the concomitant pathology.
Antibiotic therapy. Antibacterial preparations are used for postoperative wound inflammation and to prevent postoperative inflammatory processes. These include cefazolin or gentamicin if allergy to B-lactams is present, or vancomycin if methicillin-resistant Staphylococcus aureus is identified/high risk. The Scottish Intercollegiate Guidelines and others strongly recommend antibiotic prophylaxis for these types of surgeries (2,3,4). Changes in the antibiotic list for perioperative prophylaxis should be based on in-hospital microbiological surveillance.
Administration of NSAIDs for postoperative pain relief should be started intravenously 30-60 minutes before the expected end of surgery. Intramuscular administration of NSAIDs is not indicated for postoperative pain relief due to variability in serum concentrations and injection-induced pain [6], with the exception of ketorolac (intramuscular administration is possible).
NSAIDs are contraindicated in patients with ulcerative lesions and a history of gastrointestinal bleeding. In this situation, the drug of choice would be paracetamol, which has no effect on the gastrointestinal mucosa.
A combination of tramadol and acetaminophen is effective (6).
Table 1. Medications used for ankle injuries (without anesthetic support)
classification
Arthritis of the ankle is classified in several ways:
2. by cause.
Primary arthritis is direct damage to joint and cartilage tissue. The secondary form develops as a complication of other systemic diseases.
3. by shape. Reactive, psoriatic, rheumatoid, post-traumatic.
4 By type of lesions - unilateral, bilateral. Migratory arthritis occurs with gout.
With an isolated inflammatory process, monoarthritis is diagnosed. More commonly, however, the disease process affects multiple joints and polyarthritis, oligoarthritis, is present.
Symptoms of ankylosing spondylitis
The clinical picture depends on various factors - the type and severity of the inflammation, the form and stage of the disease.
Depending on the stage of the disease
General Symptoms
- Sensation of pain only on exertion, decreases after rest. Problems with foot mobility and stiffness are mild.
- The pain becomes strong and constant, does not subside with rest. The complaints increase with changing weather conditions. The mobility of the foot is significantly restricted.
- The ankle loses mobility completely and the person can only move around with the help of aids. There is a pronounced deformation of the foot, the anatomical alignment is disturbed, and all this leads to disabilities.
How is osteoarthritis in the ankle treated?
The ICD code - International Classification of Diseases Revision 10 - was introduced to ensure confidentiality and standardize diagnoses. The class includes all diseases of the connective tissue and the musculoskeletal system. All species have a code. For example, purulent staph arthritis has the code M00.0.

With such a wide variety of diseases, classification is an invaluable aid in establishing an accurate diagnosis. The ICD 10 systematizes statistics and provides an expanded list of symptoms and signs, including a detailed description of acceptable indicator values of biomaterials taken for analysis. It also contains examples of how to formulate a diagnosis correctly. This ensures that the ICD-10 diagnoses are correct.
Once an accurate diagnosis has been made and the causes identified, the doctor will prescribe comprehensive treatment and decide whether it should be inpatient or outpatient. In any case, it is important to avoid or minimize stress on the foot by leaving it in bed and moving around with an elastic bandage and possibly a cane. In the case of symptoms of an acute infection, the prescription is:
- Antimicrobial Injections.
- anti-inflammatory drugs.
- Drugs containing glucosamine.
- Diet that does not include salty foods.
The purulent form requires intravenous antibiotics (after oral treatment). In complicated cases, an operation with drainage of the joint is required. Further treatment includes pain relievers and compresses. Sometimes the joint is blocked with a splint.
Treatment for ankle arthritis should be immediate to avoid irreversible changes that lead to disability. With a correctly classified ICD-10 diagnosis and timely treatment, mobility can be preserved for as long as possible.
Prevention and prognosis
Preventing ankle osteoarthritis requires a balanced, healthy diet, avoiding injury, and treating inflammation early. Regular physical activity with an even distribution of the load is acceptable.
It is not possible to completely get rid of arthritis, but with the help of medicines and folk remedies, achieving a long period of remission is quite feasible. Obesity is not only an additional burden for the joints, but also for the functioning of the internal organs.
You can find an overview of the treatment of arthrosis in the ankle in our video:
In the ICD-10, the term 'post-traumatic osteoarthritis' is treated as a nosological synonym for the diagnosis 'non-specific osteoarthritis' (M19.9).
Active ingredients within code M19.9
Below is a list of active substances in ICD-10 code M19.9 (names of pharmacological groups and list of trade names associated with this code).
- Active Substances
- Aminophylline + Diphenhydramine + Indomethacin Pharmacological group: NSAIDs - acetic acid derivatives and related compounds in combination with other drugs
- Amtolmetin guacil Pharmacological group: NSAIDs - acetic acid derivatives and related compounds
- Azoximer bovgialuronidase Pharmacological group: Enzymes and antiferromagnetic agents
- Valdecoxib Pharmacological group: NSAIDs - coxib
- Hyaluronic acid Pharmacological groups: Metabolism correctors of bone and cartilage tissue, regenerating and repairing agents
- Hydrocortisone Pharmacological groups: glucocorticosteroids, ophthalmics
- glucosamine + chondroitin sulfate Pharmacological groups: Correctors of metabolism of bone and cartilage tissue
- Dexamethasone Pharmacological group: glucocorticosteroids, ophthalmic drugs
- Dexetoprofen Pharmacological group: NSAIDs - propionic acid derivatives
- Diclofenac + misoprostol Pharmacological group: NSAIDs - acetic acid derivatives and related compounds in combination with other drugs
- Diclofenac + pyridoxine + thiamine + cyanocobalamin Pharmacological groups: vitamins and vitamin-like products in combination with other drugs, NSAIDs - acetic acid derivatives and related compounds in combination with other drugs.
- dimethyl sulfoxide Pharmacological group: Dermatotropic agents.
- Bile Pharmacological group: Topical irritants
- Ibuprofen Pharmacological group: NSAIDs - propionic acid derivatives
- Indomethacin Pharmacological group: Ophthalmics, NSAIDs - acetic acid derivatives and related compounds
- Ketoprofen Pharmacological group: NSAIDs - propionic acid derivatives
- Ketoprofen lysine salt Pharmacological group: NSAIDs - propionic acid derivatives
- Cat's claw bark extract Pharmacological group: Anti-inflammatory and adaptogens
- Lidocaine + Tolperizone Pharmacological group: n-holinolytics (muscle relaxants) in combination with other drugs
- Mabuprofen Pharmacological group: Other non-opioid analgesics, including non-steroidal and other anti-inflammatory drugs
- Meloxicam Pharmacological group: NSAIDs - Oxycams
- Meloxicam + chondroitin sulfate Pharmacological groups: correctors of bone and cartilage metabolism in combination with other drugs, NSAIDs – Oxycam in combination with other drugs.
- Methylprednisolone Pharmacological group: Glucocorticosteroids
- Naproxen Pharmacological group: NSAIDs - propionic acid derivatives
- Naproxen + esomeprazole Pharmacological group: proton pump inhibitors in combination with other drugs, NSAIDs - propionic acid derivatives in combination with other drugs
- Nimesulide Pharmacological group: Other non-opioid analgesics, including non-steroidal and other anti-inflammatory drugs
- Nifluminic acid Pharmacological group: Other non-opioid analgesics, including non-steroidal and other anti-inflammatory drugs
- Chili pepper extract Pharmacological group: Topical irritants
- Prednisolone Pharmacological group: Glucocorticosteroids
- Salicylamides Pharmacological group: NSAIDs - salicylic acid derivatives
- Tenoxicam Pharmacological group: NSAIDs - Oxycams
- Pharmacology Group: NSAIDs - Nerve and Muscle Transmission
- Pharmacology group: n-holinolytics (muscle relaxants) in combination with other drugs
- Phenylbutazone Pharmacological group: NSAIDs - butylpyrazolidines
- Celecoxib Pharmacological group: NSAIDs - coxib
- Etoricoxib Pharmacological group: NSAIDs - coxibs
symptoms
The main symptom of arthralgia is pain of different types, intensity and duration. They usually get worse with physical activity, but can also be triggered by prolonged inactivity.
Pain syndrome is often characterized by redness of the affected joints and visible swelling. Motor activity is impaired, and sleep and general well-being may also be affected.
diagnosis
Arthralgia is a very serious symptom. If the pain lasts longer than two days or occurs briefly but recurs, a specialist should be consulted so that treatment can be started in good time. The patient should contact a general practitioner, a rheumatologist or an arthrologist (the latter are more specialized and work in large medical centers). If it is obvious that the pathology was caused by trauma, a trauma surgeon should be consulted.
The main task of the specialist is to determine the cause of the joint pain. For this purpose, diagnostic measures are taken such as:
- Examination of the patient, his medical history;
- X-ray and ultrasound examination, magnetic resonance imaging and arthroscopy of the affected joints;
- laboratory tests (blood tests);
- Biopsy of the joint tissue.
Why does a hematoma change color?
Doctors distinguish three different stages that a hematoma must go through before it completely disappears. Each of these stages is characterized by a specific color of the skin through which the hematoma shows through.
- The appearance of the bruise. Immediately after a soft tissue injury, there is severe pain, the skin at the site of the injury turns purple and swells due to tissue swelling, and the red color gradually turns blue. The red color is caused by red blood cells containing large amounts of hemoglobin. After a few hours, the hemoglobin begins to break down, and the bruised area turns blue. The swelling and inflammation of tissues at the site of injury leads to an increase in temperature.
- Green. After two to three days, the swelling and fever subside and the tissues return to more or less normal, but mild tenderness persists. The blue color of the skin changes to greenish after a few days.
- yellowing. By about day five, the swelling has completely subsided and the remaining hemoglobin is being broken down and removed from the tissues. The bruised area turns yellowish, and then returns to a normal color.
Visually, hematomas are best seen when blood collects in the subcutaneous tissue. However, if a clot forms in the deeper layers of the soft tissue, only a small but painful swelling is visible externally. Such masses are much more dangerous, because the process is not visible and can be fraught with complications.
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call +7 (495) 775-73-60.
types of injuries

The faster a hematoma forms, the more difficult it is to recover. Injuries of this type are divided into:
- Minor injuries that develop within 24 hours, are accompanied by mild pain and do not require special treatment;
- moderately severe, occurring no later than 5-6 hours after the injury, accompanied by palpable swelling and pain, affecting motor function of the limb;
- severe, occurring within 2 hours of injury and associated with limb dysfunction, acute pain, and palpable swelling.
The treatment of moderate and severe hematomas must be supervised by a doctor in order to exclude possible negative consequences of the injury.
In addition to the severity of the injury, there are other criteria for classifying hematomas:
- the depth of localization – under the skin, under the mucous membrane, in the muscle tissue, under the fascia, etc.;
- the condition of the spilled blood: intact (fresh), clotted and lysed (filled with old, non-clotting blood);
- by the type of blood spread - diffuse (blood penetrates the tissues and spreads quickly), hollow (blood collects in the spaces between tissues) and oozing (over time the blood-filled cavity is replaced by a 'sac' surrounded by connective tissue);
- depending on the condition of the vessel – pulsatile (blood flows freely out of the vessel and flows back in) and non-pulsatile (the rupture of the vessel is quickly closed by a thrombus).
Bleeding is almost always a health risk, so seek medical attention immediately after an injury.
signs
Contusions do not affect the integrity of the bone structure. The pathological process affects the soft tissues and can spread to the joints.
These injuries cause swelling that can compress nerve trunks and blood vessels, causing symptoms.
The clinical picture of bruises can be described as follows:
- pain syndrome. It can vary in severity, be locally limited or spread over the entire foot and lower leg. Immediately after the injury, there is pain, which often limits the mobility of the lower limbs.
- There is swelling of the surrounding soft tissues, which can also vary in severity.
- When blood vessels are affected, a hematoma forms at the site of the abnormality.
- It is not uncommon for patients with bruises to experience numbness in their fingers.
Often, patients with a bruised ankle are unable to stand fully on their foot, leaving them with a limp for some time.
Ankle bruises must be distinguished from broken bones, dislocations, ruptured ligaments and tendons. For this, the patient should definitely go to a hospital, where the doctor will thoroughly examine the injury site and recommend an X-ray to clarify the nature of the injury.
If necessary, a CT or MRI scan may be ordered to clarify the diagnosis or the extent of the pathological process.
First aid
It is important for everyone to know the rules of first aid for bruises in this area, since most often they appear on the street. The injured lower extremity should be elevated. This helps reduce swelling and pain.
Ice wrapped in a towel should be applied to the injured area. If this is not possible, a clean rag can be soaked in cold water and used for this purpose.
A pain reliever may be given to the patient. Nonsteroidal anti-inflammatory drugs are well suited - «,Nimesulide», «,Dexectoprofen», «,Diclofenac», «,Ketoprofen». Injectable solutions or tablet forms can be used.
When non-steroidal anti-inflammatory drugs are not available, «,Analgin» is useful for pain relief. It can be administered intramuscularly or taken orally in tablet form.
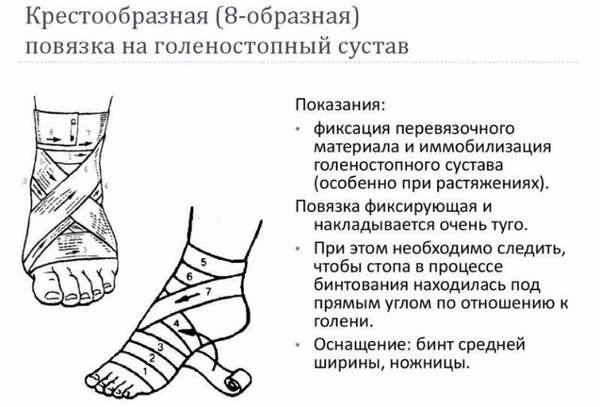
The next step is immobilization of the limb. It must be bandaged with a special elastic bandage. The bandage is applied from the toes upwards. Below is a step-by-step guide on how to put on the pad (one type). The bandage should not be too tight, as this will only aggravate the situation.
After these steps, the patient should go to a medical center to be examined by a specialist, perform diagnostic tests, and receive treatment.
What can replace NSAIDs in treating pain and inflammation?
Oral steroids, for example, are used to relieve symptoms of rheumatic origin. These drugs are only prescribed by a doctor and are not over-the-counter.
For severe pain, opioid analgesics are sometimes used. These are only available by prescription.
If the pain is caused by an injury, a cold compress may help. The cold reduces inflammation and counteracts the swelling that accompanies local injuries.
Instead of tablets you can B. Try ointments with NSAIDs that do not cause systemic side effects at the recommended dosage. In addition, over-the-counter cooling and warming ointments are available in the pharmacy, which have a pain-relieving effect and increase the mobility of the joints.
Some plants may have analgesic, anti-inflammatory, and anti-aggregation effects due to their content of certain ingredients. For example, willow bark contains salicylate derivatives.
Answers to frequently asked questions from patients
Is it advisable to take medicines from the NSAID group before or after meals?
Most drugs from this group should be taken during or after a meal, as this reduces the irritating effect of the drug on the stomach. Ointments, suppositories and drops are used regardless of the amount of food ingested.
Which tablets from the group of NSAIDs have the strongest analgesic effect?
Metamizol is used for severe pain. Ketoprofen, Dexoprofen, Meloxicam are the best pain relievers for joint pain.
How long can I take anti-inflammatory pills?
These medicines should not be taken for long periods of time. They should not be taken for more than a week without consulting your doctor. It is important to choose the lowest possible effective dose.
Can NSAIDs Cause Stomach Pain?
Medicines of this group have a negative effect on the mucous membrane of the gastrointestinal tract, which is manifested by abdominal pain, indigestion and heartburn. If prolonged intake is required, proton pump inhibitors are prescribed in parallel to protect the stomach. It is possible that this is due to taking NSAIDs on an empty stomach, which is why the drug should be taken after meals. If your symptoms worsen, you should see a specialist.
Can I take pills with coffee because some medicines contain caffeine?
Some medicines contain caffeine - often in combination with paracetamol and aspirin. However, the tablets should only be taken with water, unless otherwise stated in the package leaflet.
These medicines can reduce the ability of women to conceive during the period they are taking them. This effect usually disappears when the NSAIDs are stopped.
How do NSAIDs affect test results?
NSAID painkillers can affect liver test results, blood sugar levels, and thyroid hormone levels.
Read more:- Injury to the ankle.
- Injury to the ligaments of the ankle.
- Hip Amputation Surgery Code.
- Injury to the ankle.
- dislocation of the ankle.
- ligaments of the ankle.
- Injury of the tibial condyle.
- Injury of shin ligaments.
