The main causes of forearm muscle pain are due to triggers that directly affect the muscle tissue and not the joints or vascular system. It is assumed that muscle sprains, ligaments and strains are accompanied by pain sensations that are typical of the symptoms of muscle injuries. It should be noted that in recent decades other conditions and diseases have also become quite common etiological causes encountered by clinicians as part of a comprehensive diagnosis.

- Radial band of the superficial muscles of the forearm
- Ulnar group of superficial muscles of the forearm
- The forearm: where is it located? Photo of human skeleton
- The bones of the forearm
- Symptoms of muscle pain in the forearm
- Diagnosis of muscle pain in the forearm
- How is the production carried out?
- Production steps of the insoles:
- Testing methodology.
- Knee ultrasound protocol
- Characteristic signs
- diagnosis and treatment
- What is the correct difference between systolic and diastolic pressure?
- conclusion
- INTERNET STORE ANATOMYASNA sleep in Azov
- Special offers
- Article
- Popular Brands
Radial band of the superficial muscles of the forearm
1. M. brachioradialis, the brachialis muscle, lies on the anterolateral surface of the forearm, along its lateral edge.
This muscle attaches to the side edge of the humerus and is located between the brachialis and triceps muscles. Its belly then descends in front of the radius and merges into a long tendon in the middle part of the forearm, which attaches to the radius above the styloid process.
Medially, this muscle borders the pronator teres and flexor carpi radialis muscles.
Function. Bends the forearm at the elbow joint and brings the radius into an intermediate position between pronation and supination (this is the position that the forearm and hand normally assume when the arms are lowered freely). (Inn. CV-VIII-N. radialis.).
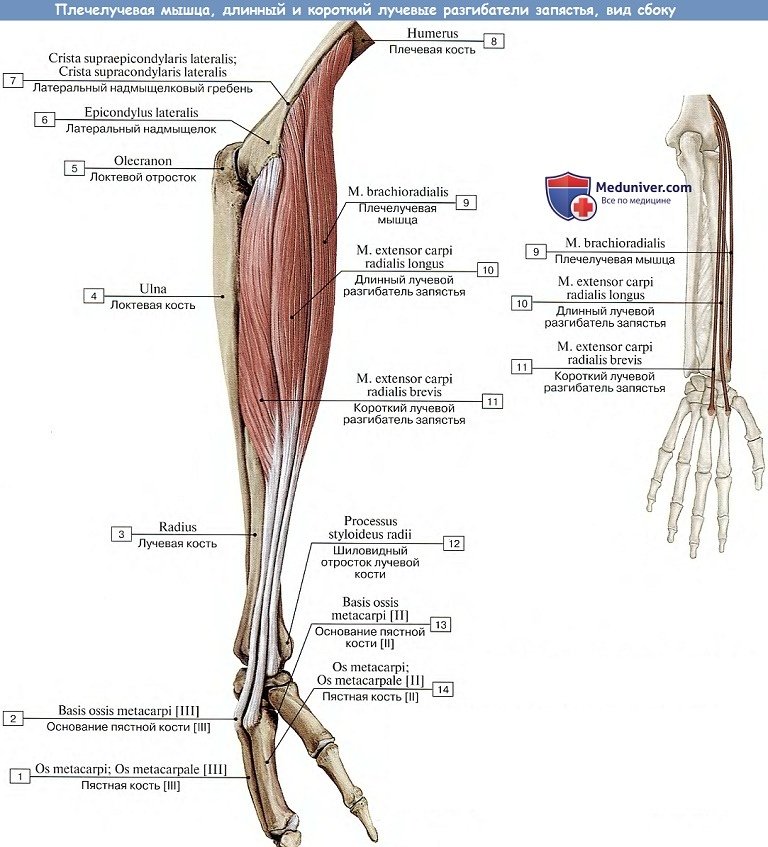
2. M. extensor carpi radialis longus, the long radial extensor muscle of the wrist, The extensor carpi radialis longus muscle is located on the posterolateral surface of the forearm, behind the preceding muscle and attaches to the lateral edge and lateral epicondyle of the arm.
In the middle part of the forearm, the muscle passes into a tendon, which runs along the lateral surface of the radius bone, then approaches the extensor retinaculum and attaches to the dorsal surface of the base of the second metacarpal.
Features. Allows extension of the hand as well as abduction (radial side) (the latter together with the flexor carpi radialis muscle). (Inn. CV-VIII to the radial nerve).
3. M. extensor carpi radialis brevis, the short radial extensor muscle of the wrist, The extensor carpi radialis brevis is located behind the long radial extensor and begins at the lateral epicondyle of the humerus, together with the tendon of the extensor carpi radialis longus, and both cross the abductor pollicis longus and the extensor pollicis brevis distal third of the forearm and the tendon of the long extensor of the thumb at the wrist.
Ulnar group of superficial muscles of the forearm
4. M. Extensor digitorum, finger extensor, The extensor digitorum muscle is located on the entire posterior surface of the forearm and arises together with the extensor carpi radialis brevis muscle on the lateral epicondyle. In the middle part of the forearm, the muscle divides into four bellies, each of which gives rise to a long tendon. The tendons run down to the back of the hand, under the extensor retinaculum through the fourth canal there and are then distributed over the four fingers (II-V).
On the back of the hand near the metatarsophalangeal joints, the tendons are connected to one another by oblique fiber bridges, the intertendine connexus, so that the two middle fingers can only be extended together; The index finger and partly also the little finger retain their independence through the presence of their own extensor muscles.
Each of the common extensor tendons on the dorsum of each finger merges into a triangular extensor tendon, which is divided into three bundles, the central one attaching to the base of the middle phalanx and the lateral ones to the base of the distal phalanx.
Features. Stretches the fingers II – V and causes the hand to stretch. (Inn. CVI-VIII to N. radialis).
5. M. extensor digiti minimi, extensor muscle of the little finger, is separated from the common tendon of the fingers on the ulnar side. Its long tendon passes through the fifth canal under the extensor retinaculum on the back of the hand to the little finger and joins the common extensor tendon of this finger.
The function of the is evident from the name. (Inn. CVI-VIII is radial nerve).
6. M. extensor carpi ulnaris, the ulnar extensor muscle of the wrist, which borders with its lateral edge on the common extensor muscle and the extensor muscle of the little finger, attaches with these muscles to the lateral epicondyle of the humerus and to the posterior edge of the ulna. The tendon of the muscle runs through the sixth tendon canal under the extensor retinaculum and attaches to the base of the metacarpal bone V (tuberositas ossis metacarpi V).
The forearm: where is it located? Photo of human skeleton
So, a bit of theory. An anatomical atlas or skeletal model will help answer the question of where the human forearm is located. The forearm bones are one of the components of the human upper limbs that play an important role in the mobility of the arm. If you look closely at the picture of the skeleton, you can easily see where the shoulder and forearm are.
The name suggests that the forearm lies below the arm bones, precedes them and together forms the base of the human upper limb. To understand the anatomy of the upper limbs, one must examine the bones that make them up.
The bones of the forearm
The part of the upper limb - the forearm, where the two bones are located - has a fairly simple structure. It consists of the long bones ulna and radius, each of which has a special structure.
What you need to know about the structure of long bones:
- They consist of the diaphysis, the metaphysis and the pineal gland. The diaphysis is the moderately elongated part of the bone that has a cylindrical or triangular shape. The metaphysis is the space between the diaphysis and the pineal gland. The pineal gland is the thickening necessary for connection to the joint.
- The articular surface is located on the epiphysis, which is covered by articular cartilage.
- Depending on the location of the bone, the epiphysis can be proximal (top) or distal (bottom).
- The metaphysis and the cartilage above ensure that the long bones grow in length.
- The cap is spongy and the diaphysis is compact.
The shaft of the elbow and radius bones is triangular, meaning it has three faces. The front of the bone faces forward and the back faces backward. The position of the third side on the radial and ulnar bones is different.
Symptoms of muscle pain in the forearm
Symptoms of pain in the body can vary depending on the location of the pain, its cause, and associated complications. The symptoms of forearm muscle pain are no exception and can be independent, such as: B. in myofascial syndrome, but also occur secondary to an underlying pathology.
In general, the symptoms of forearm muscle pain are very typical of myogenic sensations. The muscle thickens due to overstretching, which often manifests itself as a stabbing pain, but the symptom does not occur alone. It can be made worse by palpation, squeezing, bending or extending the arm, moving the arm, or applying additional pressure. If the muscles are not relaxed, chronic pulling pain occurs and an inflammatory process can develop - myositis. Myalgia caused by a chiropractic factor can also cause numbness, coldness, and weakness in the fingers of the injured hand. It should be noted that of all types of pain, myalgia is the least studied, so the doctor needs not only knowledge, but also practical experience and mastery of all modern diagnostic methods and techniques in order to differentiate the symptoms and make an accurate diagnosis .
Diagnosis of muscle pain in the forearm
Due to the non-specificity of the symptoms, the diagnosis of forearm muscle pain should primarily be differentiated. Traumatic injuries to the arm - sprains, fractures - are the easiest to diagnose because their symptoms are obvious and the x-ray confirms the injury.
Unfortunately, there is no diagnostic standard, no 'red flag pain system' for the forearm, so the doctor has to rely on his own experience and use all possible means to determine the cause of the symptom.
First of all, cardiovascular disease - angina pectoris, heart attack - is excluded, especially if the patient complains of pain in the left arm. Radicular syndrome, to which forearm pain may be secondary, must also be ruled out or confirmed.
The most important examination methods in the diagnosis of forearm pain are as follows:
- Interview the patient, including inquiring about precipitating occupational factors, to determine possible radicular syndrome. The characteristics of the pain - intensity, sensation, location, duration, dependence on postural changes and arm movements noticed by the patient - are also examined.
- Visual inspection of the patient's upper body, examining not only the painful forearm, but also the other arm.
- Assessment and examination of the neurological condition, palpation of the sore arm, spinal sections.
- Examination of rotational movements – at the elbow and wrist.
- X-ray examination of the spine. Examination of the cervical spine with functional tests.
- To clarify the diagnosis, a CT or MRI scan can be ordered to determine the type of compression changes (herniated discs, hernias).
- Electromyography, which assesses the bioelectric potential of muscle tissue and its conductivity (speed of pain signal conduction).
The diagnosis of forearm muscle pain directly depends on the clinical symptoms and their specificity. Therefore, the doctor often performs various motor tests that are particularly effective in detecting tunnel syndrome, epicondylitis, tendinitis and rheumatic joint injuries.
How is the production carried out?
 | First, the causes of the symptoms are clarified. |
 | A clinical examination is carried out by an orthopedist. |
 | The arch of the foot is assessed visually, the area of overload and the distribution of the load on the different parts of the foot are determined. |
 | Functional tests are used to determine the reaction of the arch of the foot to changes in position (loads). |
 | Based on the results, the doctor fits the foot with an orthopedic insole made of semi-fabric (thermoplastic). |
Danger! The custom insoles can be tailored to any footwear, are available in a variety of shapes, are made from a variety of natural materials and can be inserted into any shoe or boot.
Production steps of the insoles:
 |  |  |  |
Read more:If you have any questions about making custom insoles, please call us: +7-926-379-74-00
Testing methodology.
The examination is carried out using linear or convex transducers with a frequency of 5 to 10 MHz. The sonographer must not only be familiar with the normal and ultrasonic anatomy of the joint being examined, but also carefully follow the proposed ultrasound protocol.
An anatomical feature of the knee joint is the meniscus, a triangular cartilage lamella that is located between the articular surfaces and protrudes somewhat into the joint cavity (Fig. 1, 2). The outer edge of the meniscus is connected to the joint capsule, while the inner edge is wedge-shaped and faces the joint cavity.
Illustration 1. Knee joint: a – front view, b – cross section.
1 – femur, 2 – lateral femoral condyle, 3 – anterior cruciate ligament, 4 – postmeniscofemoral ligament, 5 – postcruciate ligament, 6 – capsular ligament; 7 – fibula, 8 – tibia, 9 – tibial col. ligament, 10 – medial meniscus, 11 – medial condyle of the femur, 12 – medial meniscus, 13 – lateral meniscus, 14 – ant ligament. cruciate lig., 16 – ligament post. meniscofemoral, 17 – ligament post. cruciate.
1 – femur, 2 – tibia, 3 – m.quad. tendon of the tendon of the tendon of the knee, 4 - upper knee splint, 5 - anterior capsule of the patella, 6 - fat body, 7 - medial ligament of the patella, 8 - deep capsule of the patella, 9 - patella.
Injuries and diseases of the meniscus are one of the most common causes of pain in the knee joint.
At the beginning of the examination, the patient is lying on his back with his legs slightly bent at the knees. The probe is placed in the popliteal fossa parallel to the long axis of the lower limb at the point of maximum arterial pulsation determined by palpation, and this position is used to determine the correct position of the probe on the screen (Figure 3).
Knee ultrasound protocol
The following points should be documented in the knee ultrasound report:
- Presence of liquid in the top opening (present, absent).
- Echostructure of the fluid (homogeneous, heterogeneous).
- Presence of foreign bodies (yes, no).
- Straight hamstring tendon (intact, intact).
- Calcaneus – contours (smooth, uneven), presence of bursa (present, absent).
- Inner ligament – integrity (impaired, not impaired), structure (homogeneous, heterogeneous, reduced echogenicity), thickness, presence of bursitis (yes, no).
- Status of fat bodies (structure changed, not changed), hypertrophy (yes, no).
- Status of metacarpophalangeal folds – structure (changed, not changed), damage (yes, no).
- Collateral ligaments – structure (changed, not changed), presence/absence of tendon diastasis in functional test.
- Femoral and tibial articular surfaces (smooth, uneven), bony hypertrophy (yes, no), presence of additional inserts (yes, no).
- Hyaline cartilage – outline (smooth, uneven), thickness (sanded, within normal limits – up to 3 mm).
- Menisci: external – shape (regular, irregular), structure (homogeneous, heterogeneous), contours (distinct, indistinct; smooth, uneven), fragmentation (yes, no), calcification (yes, no), presence of liquid bone formation in the appendicular area (Yes No); internal – similar description of shape, structure, contours, presence of fragmentation, calcification, appendicular area.
- Presence of Becker's cysts in the tendons (yes, no).
Characteristic signs
Depending on what type of pathology develops, the symptoms vary. However, there is a general characterization of symptoms that can be used to determine the type of disease:
- Pains. Jaw discomfort can bother you when you are quiet or active. However, the pain is often not only found in the joint area. Those affected complain of a feeling of heaviness in the head and stabbing pain in the ear.
- The mobility of the joint is impaired. The joint structures do not function normally, the patient has difficulty opening and closing the mouth, and crunching and cracking are heard when moving.
- Formation of swelling. Swelling due to inflammation, the skin becomes hot and painful when palpated.
- Bruxism. The inflammation causes spasms that prevent the muscles from relaxing. This leads to teeth grinding, both during the day and at night.
diagnosis and treatment
In order to make an accurate diagnosis, diagnostic tests are essential. The dentist palpates the joint, locates the pain and determines the degree of displacement of the joint components. It is important that the patient describes the symptoms in detail, as the dentist can determine the cause of the discomfort based on the information collected. The main instrumental examination method is x-ray.
The treatment regimen depends on the type of disease. For degenerative, destructive and inflammatory diseases, antibiotics, anti-inflammatory drugs and painkillers are prescribed. If the jaw is dislocated or subluxated, the active movable structures are reduced and temporarily immobilized with an elastic bandage. Treatment should be comprehensive and monitored by a doctor.
What is the correct difference between systolic and diastolic pressure?
We want to find out what difference in blood pressure is considered normal. Let's take the normal values, which are 120/80 mmHg for an adult. It is easy to calculate the difference, which is 40 units.
However, if this difference is more than 65, this is a sign of the possibility of rapid development of cardiovascular disease. In addition, malfunction of the heart and blood vessels leads to their premature discoloration and thus accelerates the aging process.
A difference of more than 45 or less than 35 may indicate the presence of pathological processes in the body. Symptoms may not appear with such a difference, sometimes general weakness and lethargy appear.
In older people, a difference of up to 50 units between systolic and diastolic pressure is considered the age norm. After all, their tissue has become quite worn out and has lost its vascular elasticity.
conclusion
The optimal difference between systolic and diastolic pressure in 70 year olds is 40 mmHg. However, a slight fluctuation of 10 units up or down is also within the tolerance range.
If your blood pressure fluctuates by 20 units more or less and you feel fine, you probably measured your blood pressure incorrectly. However, if you feel worse, you should see your doctor immediately.
If the difference between your systolic and diastolic blood pressure is sixty or more units, you are at risk of developing cardiovascular disease. In this case, you should definitely see your doctor. To make an appointment with our specialist, you can submit an inquiry online or contact us by phone.
This entry was posted in Cardiology. Bookmark the permanent link.
All material on this website is for educational purposes only and is not intended as medical advice, diagnosis or treatment. The site administration, editors and authors are not responsible for any consequences or damage that may arise from the use of materials on this site.
INTERNET STORE ANATOMYASNA sleep in Azov
I bought a topper from the online store anatomiaasna.ru. The consultants were very friendly and helped me choose the best option for me – PROMTEX LATEX ECO 6. No prepayment was required and the order was processed quickly.
Aleksey described in detail each mattress I was interested in, pointing out all the advantages. I then decided on the mattress I wanted.
The mattress was completely wrapped in thick polyethylene. The workmanship is of high quality. My sleep was much better.
We bought a sofa topper from Sleep Anatomy. It took us a long time to decide what kind of filling we needed. The friendly staff showed and explained everything to us several times. We looked at all the options and finally decided on the Lonax Latex Memory 7 (150*200) - a mattress with two fillings. She slept fantastically comfortably!
Special offers
Article
Popular Brands
The online store 'Anatomia Snu' in Azov offers a large selection of spring and non-spring mattresses for sleeping at attractive prices. On our website you will find both high quality and budget models for children and adults, as well as many related products.
Our pricing policy and cooperation with the best suppliers allows us to sell only high quality products. We offer our customers favorable offers and discounts, a convenient ordering system and a structured catalog with ready-made mattresses in every size. If you have decided to buy a mattress or a comfortable bed for a healthy and healthy sleep, we invite you to the online store 'Sleep Anatomy'.
- pronator and supinator muscles.
- The long section of the big toe.
- Pronator - what does that mean?.
- The pronator is in anatomy.
- These are the pronator muscles.
- What is the anatomy of the supinator?.
- The flexor muscles of the foot.
- toe bone in Latin.







