Interesting!!! The bones only form during puberty according to the gender type.

- hyperkeratosis
- symptoms
- In humans
- How the cubes were created
- CT and MRI
- CLASSIFICATION OF OSTEOCHONDRAL DEFECTS OF THE TARGET BONE.
- CONSERVATIVE TREATMENT
- SURGICAL TREATMENT OPTIONS
- Rehabilitation after arthroscopic debridement
- FIXATION OF LARGE FRAGMENTS OF DETAILED CARTILAGE
- MOSAIC CHONDROPLASTY OF THE INTERVERBAL DISC
- Latin terms from this lesson:
- Anatomical structure of the heart
- The atria and chambers of the heart
- How is the pelvic bone, the most important support for humans, structured?
- Normal anatomy of the pelvis
- Pathological anatomy
- Rare anomalies
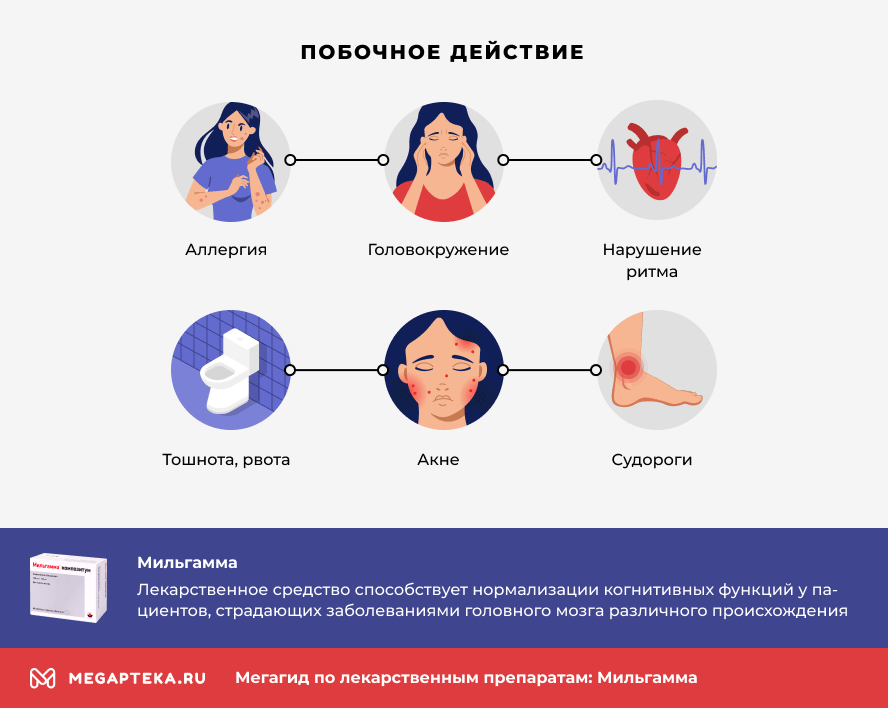
- Contraindications, side effects
- How often can Milgamma be injected?
- symptoms
- diagnosis
- Standards for second trimester fetal ultrasound findings in the summary table
- Third trimester
- Third trimester fetal ultrasound examinations in a summary review
hyperkeratosis
Hyperkeratosis is the general name for a group of diseases whose main symptom is excessive keratinization of the skin. The cells of the outermost stratum corneum are exposed to a stimulus that slows down their exfoliation process. As a result, the skin is covered with a stratum corneum, the thickness of which varies from a fraction of a millimeter to several centimeters. Depending on the cause, keratosis can affect any part of the body.
A distinction is made between hereditary and acquired skin hyperkeratosis. Depending on the clinical manifestation, the pathology can take different forms:
- Follicular – scales of the exfoliated epidermis clog the follicular ducts, creating numerous small, pustular thickenings on the skin;
- Lentiginous – keratinized papules appear on the hair follicles of the lower limbs; when they are removed, small depressions remain on the skin;
- Diffuse – skin growths that resemble short, thickened hairs;
- seborrheic – flaky, greasy, easily removed crusts form on the scalp and sometimes on the face, including reddened areas of skin;
- diffuse – affects large areas of skin anywhere on the body, sometimes even the entire skin; the sebaceous glands stop working and the skin becomes dry and flaky;
- Warts – wart-like lesions appear on the skin, but without the involvement of the papilloma virus, which sometimes develop into tumors;
- Age spots – dark, calloused spots appear on the skin of older people.
Diffuse and lentiginous forms usually occur in older men. Women and young people are rarely affected.
symptoms

The main symptom of hyperkeratosis is the appearance of thickened skin in areas of the body with reduced sensitivity, often with pigmentation that differs from the original color. Initially the skin appears rough, later the stratum corneum becomes thicker, sometimes to the point of becoming uncomfortable. In particular, advanced hyperkeratosis of the feet can lead to a change in gait. The keratinized epidermis peels or partially peels off, and thicker, drier areas may develop painful cracks that are slow to heal and become sites of infiltration. The pathology is often accompanied by dry skin and reduced sebaceous gland function.
Only a doctor can accurately diagnose this condition. Don’t delay your consultation – call us at +7 (495) 775-73-60.
In humans
Despite its irregular shape, the rash can be divided into three parts.
Facing forward Head The forward-facing head rests on the articular surface of the navicular bone and the Neck Rough surface between trunk and head, with shallow vascular channels. [3]
The body has several projecting articular surfaces: On the upper side is the trochlea of the thallus, which is a semi-cylindrical shape [6] and is surrounded by the articular surfaces of both ankles. [The notch on the ankle, called the ankle fork, holds the three articular surfaces tightly together, ensuring the stability of the ankle joint. However, since the ankle block is wider at the front than at the back (approx. 5-6 mm), the stability of the joint depends on the position of the foot: when the foot is in dorsiflexion (toes extended upward), the ligaments of the joint remain stretched . However, when the foot is in plantar flexion (as in the toes), the smaller width of the block results in less stability of the joint. (7) Behind the block is the posterior process with medial and lateral tubercles separated by a groove for the long flexor tendon of the thumb. In exceptional cases, the lateral part of these tubercles forms an independent bone called the os trigonum or accessory talus; it can be about that the proximal middle tubercle of the tarsus . On the underside of the bone there are three articular surfaces for connection to the heel bone and also several differently shaped articular surfaces for connection to the ligaments. [3]
How the cubes were created
Knuckles were originally made from the scrapes of ungulates, leading to the nickname 'knuckles' for bones. They are commonly known as 'knuckles' and are roughly tetrahedral in shape. Modern Mongols still use such bones as shagai for games and divination, with each piece having a symbolic meaning. [11]
The talus appears to have been formed by the fusion of three separate bones in the feet of primitive amphibians; shin connection to the shinbone, intermediary between the bases of the tibia and fibula and the the fourth middle piece which lies in the middle part of the tarsal bone. In modern amphibians, these bones are still partially separated, so they do not have a true talus bone. [12]
In mammals, the talus forms a much more flexible joint than in reptiles. This is most pronounced in straight-toed mammals, where the distal surface of the bone has a smooth keel, allowing greater freedom of movement of the foot and therefore greater running speed. [12]
In non-mammalian amniotes, the talus is commonly referred to as the astragalus.
In modern crocodilians, the talus has a shaft that inserts into a corresponding socket on the calcaneus, and the ankle joint is located between the two tarsi; this condition is referred to as 'normal crocodile condition'; this 'normal crocodile state' was probably inherited from the archosaurs. In dinosaurs (including modern birds) and pterosaurs, however, the ankle joint is located distal to the two tarsi. [13] [14] Much rarer are archosaurs with a 'crocodile' ankle joint, in which the calcaneus has a peg and the talus has a socket. [15]
In the dinosaurs of the Theropoda line leading to birds, the talus gradually increases in size until it forms the entire proximal phalanx of the ankle joint; In addition, the anterior process gradually lengthens more and more proximally. In modern birds, the talus fuses with the tibia to form the tibial tarsus. [16]
CT and MRI
However, computed tomography (CT) is preferred for preoperative planning. CT includes a 0.5 mm scan with 3D reconstruction of the injured joint. MRI is useful for diagnosing concomitant soft tissue injuries (muscles, ligaments, and tendons).
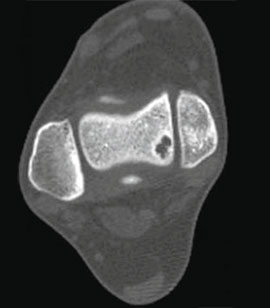


CLASSIFICATION OF OSTEOCHONDRAL DEFECTS OF THE TARGET BONE.
Stage I: small compression fracture.
Stage III: complete detachment of the fragment with dislocation.
CONSERVATIVE TREATMENT
Asymptomatic or minimal damage is treated conservatively: rest, ice, temporary weight-bearing, and orthotics for unstable joints.
SURGICAL TREATMENT OPTIONS
Several surgical techniques are available for the treatment of osteochondral injuries of the ankle. They are all usually based on one of the following principles:
- Bone marrow debridement and stimulation (microfracture, abrasion chondroplasty, perforation); New articular cartilage grows by releasing stem cells from the medullary canal into the defect area.
- reattachment of the detached cartilage fragment to the talar block if large;
- Stimulating the formation of articular cartilage by implanting the body's own chondrocytes;
- Relocation of cartilage from the knee joint (mosaic chondroplasty) or replacement of the defect with artificial cartilage.
Rehabilitation after arthroscopic debridement
After arthroscopic debridement and perforation, active flexion of the foot at the ankle joint is recommended. In the next 5-6 weeks after the operation, the foot should only be placed under moderate weight. Full weight bearing is permitted after 6 weeks. Walking on level ground is possible 12 weeks after the operation. Return to full activity and sporting activities usually occurs 4-6 months after surgery.
FIXATION OF LARGE FRAGMENTS OF DETAILED CARTILAGE
If the fragment is 18 mm or larger, fixation with one or two 2.0 mm screws is the preferred technique.
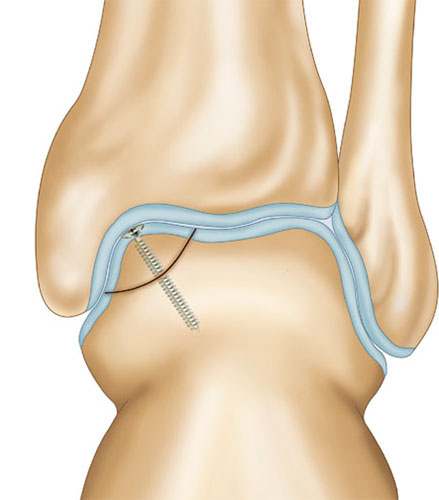
In adolescents with unsuccessful conservative treatment (of a sufficiently long period), re-fixation of the fractured plate fragment should also be preferred. The presence of a large osteochondral defect is considered negative for the health of the joint.
A spiral CT scan is mandatory to accurately assess the size and location of the defect.
The operation involves microperforation of the necrotic (dead) part of the plate. After repositioning, the fragment is fixed with 2 screws that are tightened tightly.


Biodegradable pins or anchors can be used as an alternative to metal screws.
MOSAIC CHONDROPLASTY OF THE INTERVERBAL DISC
The size of the talus defect is assessed through x-rays and CT scans.
Latin terms from this lesson:
- pes;
- Tarsus;
- metatarsus;
- ossa digitorum;
- talus;
- corpus tali;
- collum tali;
- caput tali;
- Facies superior ossis tali;
- trochlea tali;
- facies malleolaris medialis;
- facies malleolaris lateralis;
- Processus lateralis tali;
- medial tubercle;
- Tiberculum laterale;
- Sulcus tendinis musculi flexoris hallucis longi;
- Sacies articularis calcanea posterior;
- sulcus tali;
- facies articularis navicularis;
- tuber calcanei;
- facies articularis cuboidea;
- Facies articularis talaris posterior;
- facies articularis talaris media;
- Facies articularis talaris anterior.
In the next lesson I will discuss the other bones of the foot so that my articles won't be too long. At the end of this lesson, I would like to draw your attention to the fact that all the bones of the foot are very dense and have many connecting surfaces.
When studying the anatomy of each bone, pay particular attention to the articular surfaces and which surfaces of other bones they are connected to. This is the most important thing to remember about this topic.
Anatomical structure of the heart
Let's take a closer look at the anatomical structure of the heart and its chambers. Even the chambers with the same name (atria or ventricles) have completely different structures and fulfill different functions.
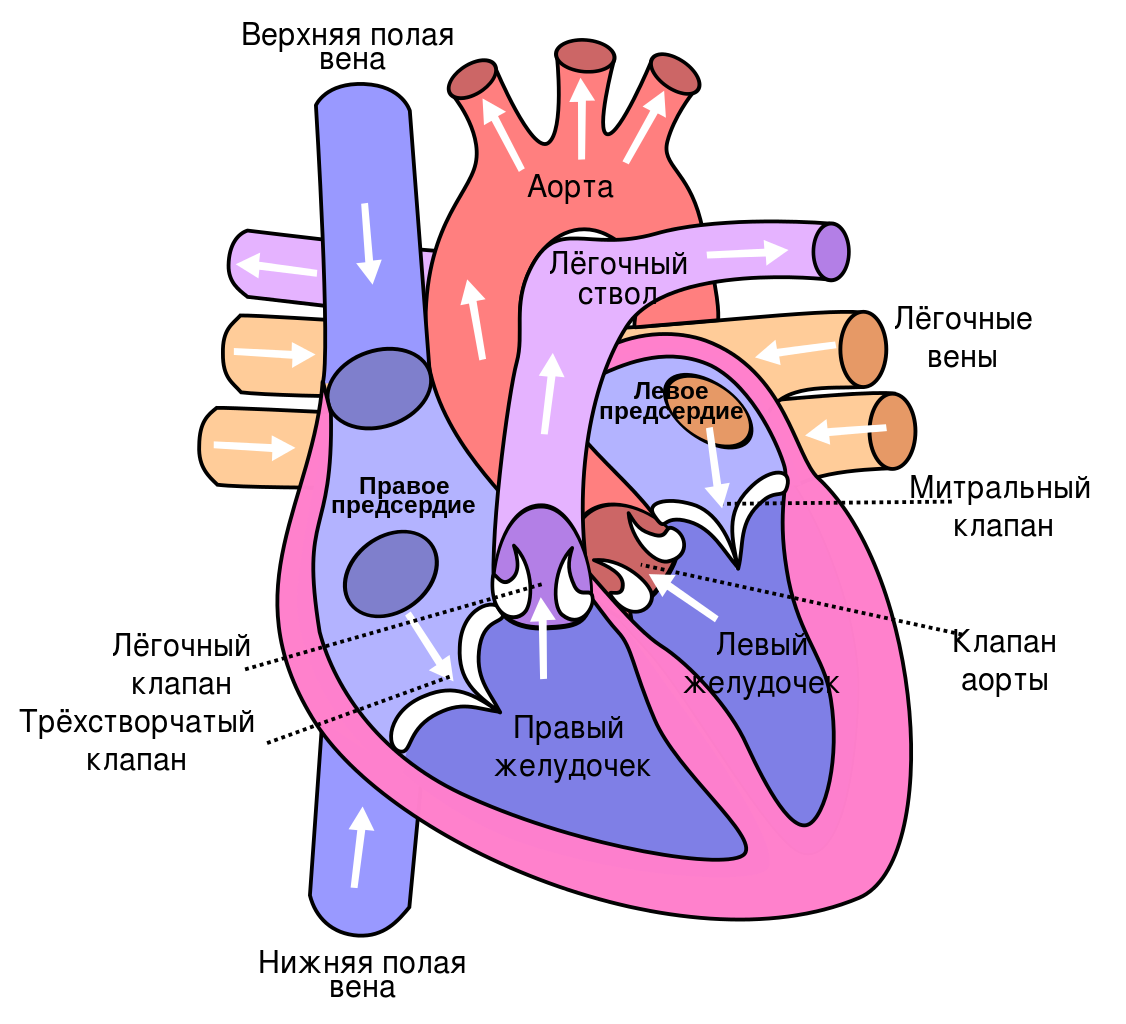
The heart is shaped like a pear, lying slightly on its side, with the tip on the left side and bottom and the base on the right side and top. The apex is the part of the heart whose movements can be felt when you place your hand on your chest in the fifth intercostal space to the left of the sternum. The heartbeat can be easily felt by both you and your child. It is the movement of the apex of the heart with each contraction. These contractions are almost synchronous with the pulse, which can also be easily felt in the arm (at the transition from the forearm to the hand) or in the neck vessels. The pulse is the filling of blood vessels with a wave of blood from the heart with each heartbeat. The frequency of the pulse and its rhythm are an indirect and easily accessible indication of the activity of the heart itself.
The apex is the most mobile part of the heart, although the whole heart, all its parts, is in constant motion.
The work of the heart, its movement, consists of two alternating phases, systole and diastole.
The rhythmic and regular alternation of these phases, essential for the functioning of the heart, is achieved through the generation and transmission of electrical impulses through a system of special cells, nodes and fibers The conduction system of the heart. The impulses are first generated in the upper node, the so-called sinus node. The impulses initially arise in the upper heart node, the so-called sinoatrial node.and then move to the second node, The atrioventricular node.From there it reaches the right and left ventricular muscles via finer fibers and causes all ventricular muscles to contract.
The atria and chambers of the heart
Right atrial The right atrium receives venous blood from the vena cava, that is, from the entire body, as well as venous blood from the heart itself. It is the largest and perhaps the most diastolic chamber of the heart. If necessary, it can absorb many times the normal blood volume, meaning it has a huge 'reserve' volume. The wall of the right atrium consists of a layer of thin muscle fibers. The right atrium not only has the task of receiving venous blood, but also controlling the heart rhythm. The two main nodes of the cardiac conduction system are located in its walls.
The right atrium is connected to the right ventricle of the heart or opens into it through a atrioventricular openingregulated through the tricuspid valve. This opening is so large that during the diastolic phase of its muscles, the diastolic phase, the entire volume of blood from the atrium enters the right ventricle and fills its cavity.
– The atrium is a much thicker muscular structure than the ventricle. It is the front part of the heart and lies directly below the breastbone. It is relatively stretchy when needed. The shape of its cavity resembles a new moon appearing in the sky. If you look closely, you can see how the bright band of the month surrounds the large dark sphere of the unlit part of the moon. In the same way, the right chamber surrounds the solid, cylindrical left chamber with its cavity.
Inside this chamber there are two cones that merge into each other: and . They converge at the apex of the heart and are separated at the top by a muscular shaft.
opens into the pulmonary artery, which together with the aorta forms the so-called main vessel. At the transition from the ventricle to the pulmonary artery is the tricuspid valve, a crescent-shaped valve of the pulmonary trunk that allows blood to flow in one direction - to the lungs.
– is the most posterior of the heart chambers. It receives oxygen-rich arterial blood from the pulmonary veins. There are a total of four veins that flow into the posterior wall of the left atrium. The ventricle of this atrium is much smaller than that of the right atrium, and its ability to expand is much less.
How is the pelvic bone, the most important support for humans, structured?
The pelvic bone provides secure support for the entire human skeleton as well as a strong structure to protect the organs located under the abdominal cavity. The anatomy of the pelvic bones is particularly interesting because of their structure and the time it takes for the structures to finally form.

Each pelvic bone is divided into the following three:
- The hipbone is the opening bone that forms the upper lobe of the pelvic bone. You can feel it by placing your hands on your hips.
- The ischium is the part of the hip bone that is located in the lower back and resembles an arch.
- The pubic bone is the anterior lobe at the base of the pelvic bones.
Together, these bones form the acetabulum, the main cavity that houses the head of the femur.
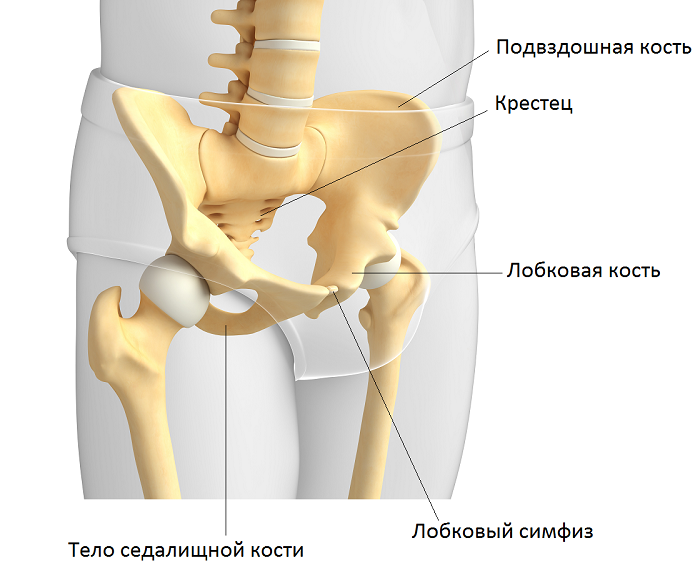
During childhood (until the ages of 16-18), these bones are connected to each other by cartilage; As we age (after the age of 18), this tissue hardens and gradually becomes a solid bone that we call the pelvis. The shaft of the ischium can be seen in the picture.
Interesting fact!!! At the base of the ischium are tubercles - rough, thickened bones. They are popularly known as sit bones because the weight of the human body is distributed across the pelvic bones when sitting.
Normal anatomy of the pelvis
The anterior pubic joint and the sacroiliac joints, which arise from the plane of the posterior ear bone and the base of the sacrum, this is the normal anatomy of the pelvic bones. The video provides a detailed insight into the structure of the human pelvis.
Pathological anatomy

There are numerous bone anomalies that depend on a number of factors ranging from intrauterine underdevelopment of bones (most common in premature babies) to trauma (dislocations, fractures), which then lead to pathology of the pelvic bones.
The most common anomalies are a wide pelvis, a narrow pelvis or a deformed pelvis.
- Broad. Today, clinically and anatomically, a distinction is made between a wide pelvis. This pathology is most often found in tall, obese people.
- Narrow. As with width, the pelvis is divided into clinically and anatomically narrow. A narrow pelvis can be caused by developmental disorders in the womb, malnutrition and some serious diseases such as rickets.
- Deformity (displacement of bones). In 99 % of cases, dislocation of the baby occurs at birth (if the baby's mother has deformed pelvic bones, the baby's skeleton, not just the pelvis, is distorted and displaced as it passes through the birth canal). This pathology is passed on from mother to child. In only 1 % of patients the pelvic deformity is the result of trauma.
- Aplasia or hypoplasia is a rare inherited disorder in which one of the pelvic bones is missing or underdeveloped.
- Deep acetabulum – the head of the femur is located lower. The pathology is unilateral or bilateral (most common).
- Diastasis pubis – most common in patients with central nervous system, bladder, or spinous process disorders.
Radiological findings provide a clearer picture of the extent of the anomaly.
Rare anomalies
The following types of malformations occasionally occur:
Contraindications, side effects
The medicine is not prescribed for children, pregnant and lactating women, patients with hypersensitivity to the components of the drug and with congestive heart failure.
- Allergic reactions (rash on the skin and mucous membranes, shortness of breath, Quincke's edema, anaphylactic shock);
- dizziness, rarely disorientation;
- Rhythm disturbances, accelerated or slowed heart rate;
- nausea, vomiting;
- Increased sweating, skin pruritus, urticaria, acne;
- convulsions.
Sometimes irritation occurs at the injection site. Tell your doctor if you notice any side effects.
How often can Milgamma be injected?
Two milliliters of the drug can be injected daily for ten days to quickly relieve the pain syndrome. Once the pain has subsided and the condition is mild, patients are given oral medication or injections of the medication solution at intervals of two to three days for two to three weeks.
Neurologists prescribe the drug Milgamma in combination with nonsteroidal anti-inflammatory drugs and central muscle relaxants. Which is better – Milgamma injections or tablets? These are the two forms of the drug that doctors prescribe one after the other. Patients first receive Milgamma injections and then tablets. With a mild course of the disease, treatment is carried out with the tablet form of the drug.
symptoms
Osteochondrosis is a condition known to be painful. It is a pain that is more localized in the joint affected by osteochondrosis and worsens with movement, especially sports. It is classified as mechanical pain. So, with Panner's disease (also known as osteochondrosis of the elbow), the patient is prone to supraspinatus pain (the pain is localized at the level of the elbow joint).
This mechanical pain can be accompanied by many other symptoms such as: B:
- Swelling and redness of the affected area.
- Limited joint mobility: The patient has difficulty bending the knee or using the affected joint. Locking of the joint may also occur.
- A lame patient with osteochondritis of the hip or knee.
diagnosis
A family doctor can diagnose osteochondrosis. It can be diagnosed by both an orthopedist and a rheumatologist. This is followed by a clinical examination and, in a second step, a series of additional medical examinations:
- The diagnosis is usually made correctly through radiological examinations. However, they do not provide data to determine the appropriate therapeutic approach because there are often discrepancies between radiological and surgical findings.
- CT provides good anatomical contouring of the osteochondral lesion but does not allow assessment of the healing potential of the lesion.
- MRI detects bone and cartilage lesions earlier than conventional X-rays and is just as accurate as arthrography. It provides data on the extent, morphology and blood flow of the lesion and is a non-invasive method that assesses the local status with high sensitivity.
Standards for second trimester fetal ultrasound findings in the summary table
Third trimester
The final routine ultrasound examination is the most comprehensive and includes the measurement and study of such fetal data:
- BPD – two-color head size;
- LZR – frontal-occipital size;
- OH – head circumference;
- OH – waist circumference;
- HD – length of glenoid bone;
- HR – length of femur;
- HD – length of humerus;
- Height – 430 – 470 mm;
- Weight – 1400 – 2400 grams;
- Beklar testicles – less than 5 mm with normal development;
- thickness of the afterbirth;
- maturation of the baby's seat;
- location of placenta, placenta previa and presence of abruption;
- IAW – Amount of amniotic fluid – 1.5 liters is the normal value;
- Length of the cervix – the normal value is between 30 and 35 mm.
Third trimester fetal ultrasound examinations in a summary review
In the first trimester, abnormalities due to chromosomal abnormalities such as: B. a frozen pregnancy and a lack of embryo growth. In addition, signs of Down, Patau, Edwards, Cornelia de Lange, Smith-Opitz, triploidy and omphalocele syndromes are clearly visible.
In the second trimester, in addition to the syndromes of the first trimester, Scherchevsky-Turner syndromes, Klinefelter syndromes, hypertensive-hydrocephalic syndromes, polysomy, polyploidy, malformations of internal organs or their absence, heart defects, defects of the facial bones, hypertensive hydrocephaly, multiple pregnancy, multiple or low fertility, umbilical cord pathology, fetal presentation, delayed fetal development diagnosed.
In the third trimester, fetal infections, defects of the brain, heart muscle, internal organs, delayed fetal development, cleft lip and palate, and fetal presentations can be noted.
The earlier fetal anomalies are discovered, the better. If chromosomal abnormalities are diagnosed, the pregnant woman will likely be offered a first or second trimester abortion. In most cases, acquired anomalies are treated with medication during pregnancy and, if necessary, after birth.
Professionals suggest solutions to the problem, and the expectant parents choose them taking into account all the risks. Each situation is individual and there are no standard treatment regimens. But even if a problematic pregnancy occurs, it is important to understand that the level of development of medicine and plastic surgery makes it possible to correct most anomalies.
Read more:- The shaft of the heel bone.
- metatarsal bones.
- pelvic bone Latin.
- pelvic bones.
- Anatomy of the heel bone.
- fibula.
- Photo of the right leg.
- pelvic tilt.
