Any surgical procedure involves cutting the skin of the human body or mucous membranes to gain access to an organ or cavity for diagnosis or treatment. The final step of the operation is to connect the severed tissues with sutures - this is the postoperative suture.

- How do I choose the right crutches?
- Types of forearm crutches
- How to choose?
- Modern surgical-medical devices from the company 'Tech-Med'
- The advantages of Tech-Med
- Equipment for surgical departments in the widest range
- Types of dressings HydroClean:
- Types of Hartmann sponge compresses:
- Postoperative dressings for open wounds.
- Walking aids – what are they?
- Who is the walking aid recommended for?
- Types of walking aids and their intended use
- Stationary
- walking aids
- On wheels
- Other accessories
- Walking stick and its variants
- Below you will find a classification of sticks according to their construction:
- walking aids
- Types of walking aids for the elderly
- Restoration of arterial blood flow
- Treatment carried out
- Can I remove the stitches myself?
- Absorbent dressings
- You might also be interested in:
How do I choose the right crutches?
The crutches can be either armpit or elbow crutches (also known as 'cane crutches'). The main difference between the two is their support. The first support is in the armpit, the second in the elbow, and the crutches are more like a stick. The wrong choice of this rehabilitation agent carries the risk of damage to ligaments, skin and muscles. Let's consider what crutches should be and which crutches are better for one case or another.

Crutches are a medical rehabilitation tool prescribed by a doctor. They are indispensable when the musculoskeletal system is impaired and we want to keep the strain on the legs as low as possible during the recovery phase.
If such a device is incorrectly selected, there is a risk of nerve entrapment:
- There is a risk of nerve entrapment;
- risk of skin abrasions;
- Inflammation of the shoulder joint is likely;
- Bone and muscle tissue can be affected;
- The load is not distributed correctly.
Types of forearm crutches
- Crutches under the arm. Required when it is necessary to completely unload the legs. Typically the first phase of recovery from an injury, which also involves light weight bearing on the arms. Not recommended for more than two years.
- Crutches with elbow support.. Prescribed by the doctor if the patient can walk or stand independently for a short time and has enough strength to put some weight on the arms. This partially relieves pressure on a limb that may already be overloaded during this phase of rehabilitation. It is suitable for permanent use, unlike the forearms.
Let's take a closer look at each of the types and the principles of selection.

Designed to shift body weight from the legs to the arms and shoulder girdle. Completely unburdens the limbs and allows walking without leaning on one leg. They consist of two rods that are joined together at the bottom of one leg. Equipped with a non-slip tab. For better support, the upper part is equipped with special padding that does not hurt the armpit. The crossbar, which is at hand level, is needed to hold the hand.
How to choose?
These orthopedic aids are selected depending on their height. The distance between the handle and the armpit and the height of the crossbar should be taken into account.
- The patient should put on familiar footwear and stand up.
- The crutch should be about 20 cm (depending on hip width) from the foot.


If the patient is unable to stand without support, the adjustments are chosen as follows: height minus 40 cm. If crutches are used, these will also need to be adjusted.
The crutches must be walked on briefly to assess the correct fit:

Modern surgical-medical devices from the company 'Tech-Med'
The company 'Tech-Med', a recognized leader in the supply of medical equipment and furniture in the Russian Federation, sells equipment for equipping institutions of any profile on favorable terms. On this page of our catalog you will find modern equipment for anesthesia and intensive care medicine from leading manufacturers. Convenient navigation as well as plenty of information about all the presented types of equipment available in this section will make it easier for you to find the right equipment and furniture.
The quality of equipment in the treatment room, intensive care unit, anesthesia and intensive care unit directly affects the effectiveness and speed of treatment. Although the most important factor is, of course, a highly qualified and experienced doctor, the use of modern equipment makes achieving the desired results much easier.
Advanced equipment in outpatient surgery makes it easier for specialists to treat multiple patients and therefore work more efficiently. Thanks to recent advances in science and technology, treatment has become increasingly effective. With modern instruments, doctors can now perform procedures and manipulations that were completely inaccessible 20-30 years ago. And the most important thing is that progress in this area is still ongoing.
The advantages of Tech-Med
Tech-Med has extensive experience in equipping medical facilities. In our catalog we have collected the best examples of modern equipment for intensive care, surgery, critical care and other departments. We constantly monitor the global medical device market and regularly update our catalog.
We work directly with manufacturers, without intermediaries, so we can sell all devices at the right price without markups. In addition, we have entered into mutual benefit agreements with many manufacturers that allow us to sell surgical medical devices at prices not available to other companies.
Equipment for surgical departments in the widest range
Browse our catalog, view the information and make your choice. Here you will find: multifunctional furniture for operating rooms, modern operating tables and lamps, the most reliable electrosurgical coagulators, syringe pumps, cryosurgical equipment and much more. Our staff will advise you if necessary and help you with your choice.
The company 'Tech-Med' differs from its competitors not only by its wide range and reasonable price level of surgical equipment, but also by its high efficiency in fulfilling all incoming orders. The equipment purchased from us is delivered to any region of Russia and the CIS countries in the shortest possible time.
Types of associations HydroClean:
HydroClean – Bandages activated with Ringer’s solution.
HydroClean plus HydroClean – Dressings activated with Ringer’s solution containing the antiseptic polyhexamethylene biguanide (PHMB).
HydroClean plus cavity – Double-sided release form for packing deep wounds and cavities with activated solution.
Hydrocline dressing series:
2. Sponge compresses -. Sponge compresses, absorb exudate and keep it inside. Maintains the right climate in the wound and stimulates healing. For non-infected wounds (use in combination with other remedies for infected wounds). They have a cushioning effect, which is beneficial in treating pressure sores. Suitable for the treatment of: pressure sores, trophic and diabetic ulcers, poorly healing wounds.

Sponge compresses Available in different sizes and shapes for use on different parts of the body.
Sacred – A dressing intended for use in the sacral area.

Sacral -. A bandage for the heel and elbow area.

Types of Hartmann sponge compresses:
PermaFoam – A sponge compress with large pores that face the wound and taper towards the top. It has a vertical capillary effect, exudate is absorbed and retained in the bandage and is not expelled even when the bandage is compressed. Creates a microclimate in the wound that stimulates healing. Use on non-infected wounds, on infected wounds use together with Atrauman Ag and other wound dressings recommended by professionals.
Permaf range of wound dressings:
HydroTac – Absorbent sponge compress covered on the wound side with a mesh layer of hydroactive gel. Thanks to the sponge-like structure and the capillary effect of vertical absorption, excess wound exudate is quickly and effectively absorbed and safely retained in the inner layer. The hydrogel coating ensures sufficient hydration for dry wounds, prevents the dressing from sticking to the wound and ensures an optimal moisture environment. For non-infected wounds.
3. hydrocolloid dressings (3) Hydrocolloid dressings are used for the treatment of moist wounds. The dressing forms a gel that absorbs exudate from the wound.
Postoperative dressings for open wounds.
If the wound is not covered by skin, things are more complicated - each case has its own nuances, and such a wound should only be treated together with a doctor.
However, it can be assumed that an atraumatic (mesh) bandage, such as B. the SilicoTulle silicone mesh dressing, and a secondary absorbent dressing will be required.
If there is heavy wound secretion, ExSorb and ExSorb Plus are suitable as secondary dressings.
If there is a risk of a wound infection, germ-soaked dressings such as TidySorb Povi with povidone-iodine are suitable.
A self-adhesive roll bandage, Roll, or a soft cohesive elastic bandage, Light, is useful for securing these bandages to the wound.
Walking aids – what are they?
A walking frame is a medical aid that allows a sick person to walk short distances. The construction consists of two strong, stable metal frames that lie opposite each other and are held together by two or more steel tubes arranged transversely to each other.
To use the walker, the patient stands in the space between the frames and grasps the upper part of the frame or the handles, if these are present in the model. Depending on the model, the patient then moves the walking aid forward about one step and then, leaning on the frame, covers the same distance with his legs.
Who is the walking aid recommended for?
- Elderly or severely disabled people who cannot walk without help.
- People with injuries or degenerative diseases of the spine and/or leg joints.
- Patients who have undergone surgery on the abdomen, pelvis, spine or lower limbs.
- Patients undergoing rehabilitation and recovering from prolonged bed rest – e.g. B. after a stroke or a broken femur.
Types of walking aids and their intended use
All walking aid models can be divided into three main groups based on their design and recommended use.
Stationary

The so-called 'classic' walking aids consist of two frames that are connected to each other by a cross tube. To move with this type of walking aid, the patient must lift it slightly and push it in front of him as far as possible and then take a step forward while holding the walking aid with his hands.
A stationary walking aid requires that the patient can withstand a certain amount of physical exertion, so this model is recommended for convalescents or people in a stable condition.
walking aids

These walking aids are similar to the stationary walking aids, but the cross tubes are attached to the frame with special joints so that the patient can move each frame in turn, giving the walking aid an I-shape.
Since the walker does not need to be lifted, it is suitable for very weak people - older people, after a stroke, after major operations, etc.
On wheels

These walking aids have a similar structure to stationary walking aids, but have wheels instead of legs. Such walking aids do not need to be lifted, but can simply be rolled, which is extremely important for people with disabilities, with complex spinal injuries, immediately after abdominal operations, etc.
Some models of this type of walking aid only have two wheels at the front and therefore still need to be lifted slightly. Many rollators are equipped with a handbrake system that prevents rolling on inclines.
Other accessories
In addition to the type, walking aids can also be classified according to the presence or absence of the following useful accessories:
Walking stick and its variants
A walking stick is a structure consisting of only three elements: a handle, a body and a tip. The cane provides stability and relieves pressure on the partially injured lower extremity.
Depending on the construction material, the sticks are divided into steel, aluminum or wood.
Below you will find a classification of sticks according to their construction:
- Standard canes (walking sticks). These are classic models with a one-piece (unassembled) stick drum. These models are often used by completely healthy people as an elegant accessory. However, for an elderly person who is weakened, the classic version of the cane is not safe and not always comfortable. Therefore, it is better to choose other models of orthopedic aids that are more functional.
- Telescopic poles. This type of product allows you to adjust the shaft up and down. A telescopic cane is ideal for most older people. You can easily change the length of the stick, which is certainly a necessity given the seasonal fluctuations. As footwear changes, a person's height also changes. The changes may be minor, but may still affect the usability of the stick.
- Canes with multiple supports. A stick that has 3 or 4 poles at its end. This model guarantees greater stability and is designed for higher loads. The cane with multiple supports is suitable for older people with severe musculoskeletal impairments, for people with severe physical limitations and for overweight people.
- A stick with an offset center of gravity. The cane is stable at different angles and is particularly suitable for older people who have problems with motor coordination.
- Stick stool. The mechanism of the model transforms into a small chair.
- Walking stick with armrest. Provides better support and relieves strain on the arm by distributing the load across the forearm. Suitable for the elderly with severe weakness of the lower limbs.
- Walking stick for blind people (tactile walking stick). This aid is usually made of lightweight materials and has reflective elements. Some models are equipped with sensors and ultrasonic signals to alert the blind person to objects on the road.
walking aids
If an elderly person has severe weakness in both lower limbs due to musculoskeletal diseases (arthritis, arthrosis, etc.), often suffers from dizziness and pressure fluctuations, or is recovering from a stroke, he or she definitely needs a walking aid.
The walking aid is a strong and stable construction with a four-point base. This walking aid helps minimize strain on the legs and improve coordination. In order for an older person to be able to use a walking aid safely and comfortably, it is worth choosing it carefully.
Types of walking aids for the elderly
- Stationary walking aid 'without step'. This is the basic and simplest model. The frame of this product is made of aluminum, making it lightweight and strong for a long service life. The walker is usually foldable or unfoldable, which is convenient for transport in the car. It is possible to adjust the height. The older person moves by repositioning the entire structure in front of them. It should be noted that at the moment of changing the position of the walking aid, the load rests completely on the legs, so this type of product is suitable for older people without motor coordination disorders.
- Walking aids. This type of support simulates walking using special articulated frame elements. For older people it is sufficient to alternately use the right and left side of the walking frame. They seem much more comfortable than a standard model. For a young person in the rehabilitation phase – yes. But do not forget that support measures are chosen for a grandparent who finds it difficult to immediately master such a structure. So be patient and spend more than one day with your elderly relative and help him or her practice getting around with a walker.
- Walking aid with two wheels. This is the same as the stationary model but has two wheels instead of legs at the front. To move, you lift your legs and roll the walker forward. A questionable form of support for an elderly person in terms of safety and comfort. Firstly, there is a high risk of losing balance. Secondly, the wheels are usually very small and there is no cushioning. This means they can only be used on a flat, hard surface. Even on a well-paved sidewalk, impacts cannot be avoided.
- Trolleys on wheels. This type of tool has all four ends as wheels. Unlike the previous model, the wheels are large and have wide inflatable rubbers. According to experts, this type of support is most popular among older people who need a walking aid. However, older people are initially afraid of rollators - they fear that the support will literally fly away. However, this is impossible because the model is equipped with a handbrake. The equipment also includes a seat and sometimes a practical shopping net. The maneuverability of the rollator is remarkable - the wheels can be rotated 360 degrees. This type of walker is definitely suitable for long outdoor walks, which is especially important for older people with health problems.
- For older people with excessive body weight, there is e.g. B. Rollators with a reinforced frame. Walking aids with reinforced frames. While a normal model can support a maximum weight of 110kg, these special models can handle a maximum weight of 225kg.
Restoration of arterial blood flow
Based on his examination and given the ineffectiveness of conservative treatment, the patient was referred to an angiosurgeon for reconstructive surgery of the arteries of the lower extremity. The operation was carried out from 05/13/03 to 06/02/03 at the 25th Central Strategic Missile Military Hospital.
The following results were obtained during the inpatient examination.
Clinical blood count: hemoglobin – 128 g/l, erythrocytes. – 4.36*10 12 /l, Leuk. – 6.8*10 9 /l (pall. – 2%, segmental – 62%, eos. – 2%, lymph. – 28%, mon. – 6%), sedimentation rate – 23 mm/h.
Clinical urinalysis: Specific gravity of urine – 1014, protein – 1.22%, no cyl. – 2-4 in p/zr, eryth. – 3-5 in p/zr.
Biochemical blood analysis: total protein – 69.0 mmol/l, bilirubin – 10.0 mmol/l, creatinine – 120 µmol/l, urea – 6.1 mmol/l, cholesterol – 4.8 mmol/l, β-lipoproteins – 40%, triglycerides - 1.0 mmol/L, ALT, AST - normal.
ECG: Sinus rhythm, normal, 68 beats/min. Horizontal position of the electrical axis of the heart.
X-ray of the chest organs: the lung fields are transparent. The roots are fibrous, with fossils. Left ventricular hypertrophy, thickening of the aortic arch.
Ultrasound examination of the abdominal organs: liver, spleen, gallbladder, pancreas, kidneys - no pathological changes.
Angiography of the arteries of the lower limbs: abdominal section of the aorta with irregular contours, the lumen is preserved. Contours of the main arteries of the lower limbs irregular, lumen preserved, significant calcification of the arterial walls. The main arteries of both tibiae had irregular contours and were severely compressed below the malleolar fissure. Two critical tandem stenoses were noted in the distal left posterior tibial artery. The soleus arterial arches are patent.
Treatment carried out
Antibiotic therapy (ofloxacin 200 mg twice a day), surgical treatment of the wound (excision of necrotic tissue from a pocket up to 3 cm deep), disinfection therapy, intravenous disaggregation. The patient was switched to insulin therapy (Actrapid 8 units p/w, 6 units p/w; Monotard 8 units p/w, 8 units - 22.00), carbohydrate balance was achieved (glycemic profile on 06/25/03: 8.9- 6.5-4.7-7.4-5.1 mmol/l). The patient is continuously treated with enalapril 10 mg/day for stage IV diabetic nephropathy.
On May 20, 2003, the patient underwent radiographic vascular angioplasty of the posterior tibial artery on the left side; blood flow in the artery was restored.
The operation was performed under local anesthesia 0.5%-20.0 Sol. Novocaini had the anterograde femoral artery punctured via a left transfemoral approach. A coronary conduit was inserted into the posterior tibial artery distal to the stenosis through a 5F diameter intraductor. A 2.5×20.0 mm balloon catheter segment was placed in the area of critical stenosis. Angioplasty was performed with a working pressure of up to 5 atm. On the follow-up angiogram, the stenosis was resolved and no obstruction to blood flow was noted. The guide wire was removed. The intraductal segment was sutured to the skin. An aseptic dressing was applied. During the procedure, the patient received an intraarterial injection of 7,000 units of heparin. The patient's condition did not change.
After hospital discharge: right and left Doppler study of main blood flow in the posterior tibial arteries showed altered main blood flow (LPI > 1), in the dorsal foot arteries there was collateral blood flow but LPI > 1 (possible overestimation of the brachial index of the ankle due to atherosclerosis of the Menkeberg arteries).
The transcutaneous oxygen tension (tcpO2) on the dorsal side of the left foot (three months after angioplasty): 19 mmHg in supine position, 20 mmHg in sitting position (possible underestimate due to foot edema). Based on a combination of clinical findings, wound condition, and instrumental findings, it was concluded that the critical ischemia phenomena had resolved.
In recent years, special absorbable suture material has been used, which dissolves over time from the human body. The choice of suture material depends on how long the effect of the connective tissue should last. If it is not possible to use absorbable sutures, ordinary sutures are used, which the doctor removes after the wound has healed. As a rule of thumb in medicine, there are certain time intervals between the insertion of the stitches and their removal:
- In the abdominal area – 7-10 days;
- On the chest – 10-14 days;
- Head/Face/Neck – 6-7 days;
- Lower leg/foot – 10-14 days;
- With laparoscopy – 6-14 days;
- After a cesarean section – 8-10 days.
It is not possible to determine in advance exactly when and how the procedure will be performed, since the regenerative ability of tissue is an individual process, which largely determines when the sutures will be removed. Older age, debilitation, comorbidities, abscessed or infected wounds may also affect how long the stitches are left in place.
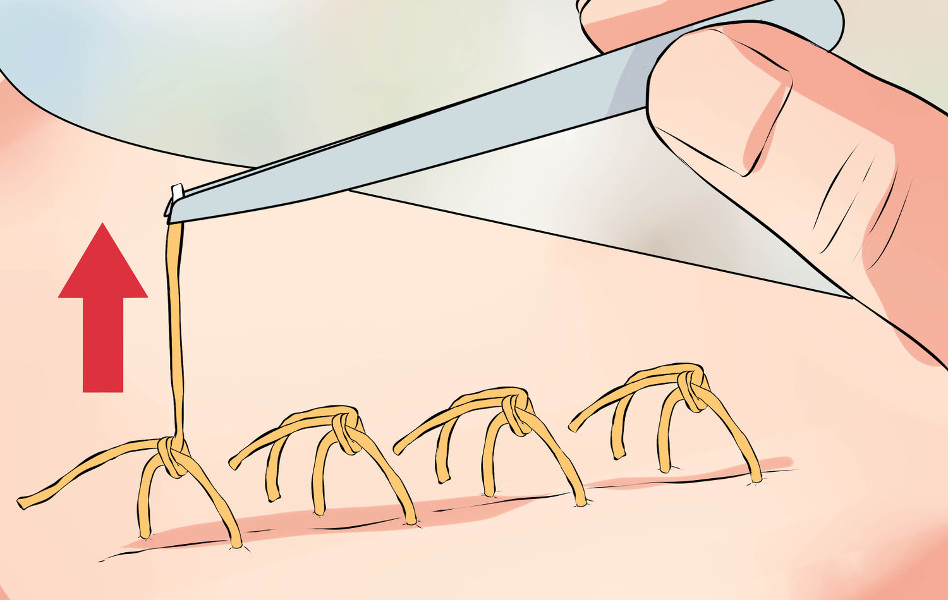
- Antiseptic treatment
- Removal of suture material (suture removal)
- Secondary antiseptic treatment
- Applying a therapeutic ointment
- Association
- Required materials and preparations
The main indicator that it is time to remove the stitches is the healing of the wound. This can be determined by various signs:

It should be borne in mind that too early intervention will cause the stitches to dissolve, and if removal is delayed, there is a risk that the wound will abscess and the stitches will grow into the skin. Regardless of whether the patient has the stitches removed at home or in the hospital, a surgeon should be consulted. Only an experienced specialist is able to assess wound healing and thereby minimize possible complications.
Can I remove the stitches myself?
At first glance, removing threads may not seem complicated. But even a small mistake can lead to serious problems. Only medical personnel have the proper skills and tools, so it is not recommended that you do it yourself.
If it is not possible to ask for help, you can at least remove the stitches yourself, but only for small wounds and when you are sure that the wound has completely healed. The most important rule is the sterility of the instruments. Please also note that it is strictly forbidden to touch the threads:
- After complex strip operations;
- after cosmetic surgical procedures;
- If staples or metal threads are used;
- in the presence of inflammation or pus.
If the patient wants the stitches to be removed at home after the operation, it is better to have this done by a trained specialist than to try to do it yourself and carry out the procedure without risk to health.
Absorbent dressings
Absorbent dressings are often used on wounds that are very wet and contain a lot of secretion. Such dressings help combat the odor of infected wounds and wounds with rotting tumors. They contain superabsorbents and silver.

CARBONET. Absorbent, deodorizing, non-adhesive dressing with activated carbon. Photo: rekate-medical.ru

Sterile dressing Zetuvit E. Photo: www.deznet.ru
The combination bandage consists of a layer of sponge, alginate and silver. It absorbs exudate well, reduces odor and maintains a moist environment. Used for infected wounds and necrosis.

Head wounds: prevention and treatment Doctors at Hospice Samara give tips on how to prevent pressure sores on the head of a seriously ill patient and what to do if they appear
Please remember that if you use modern dressings to treat pressure sores, you will not solve the problem. Bedsores can only be effectively treated if we eliminate the cause of the problem - the persistent stress on the body's tissues when a person lies in the same position for more than two hours. Without constant change of posture and correct positioning of the body, no bandage will help heal bedsores.
You might also be interested in:
Varicose veins: causes, complications, treatment. How varicose veins develop and what happens if they are left untreated.
Bedsores in children: prevention and treatment. To prevent pressure sores in seriously ill children, the same care regulations must be followed as for adults. However, some special rules apply to them.
Rules for using an anti-decubitus mattress. What anti-decubitus mattresses are there, how to achieve the effect of anti-decubitus mattresses.
The diabetic foot: recognition, treatment and prevention of amputations. How to avoid this dangerous complication of diabetes, how to treat it, how to choose the right footwear and care for your feet.
The material was prepared with the help of a grant from the Presidential Grant Fund of the Russian Federation.
Read more:- Shoes for the elderly with sore feet.
- Bracers for children with cerebral palsy.
- insoles for walking.
- disc stopper.
- footprint while walking.
- residual limb bandage.
- Walking school with prosthesis.
- Boots for a broken leg.

