Table 1: Pirani Initial Severity Scale (Points)

- Streptococcus equinus
- phylogeny
- The equinus foot - orthopedic problems
- Equine Foot Diagnosis
- Doctors' and patients' opinions on the Jaquinus procedure
- keywords
- case report.
- symptoms of the disease
- How the disease manifests itself
- How does the drug Eliquis help?
- Contraindications to taking the drug Eliquis
- Treatment of clubfoot (clubfoot)
- Treatment of equinovarus foot deformity
- What is equinus or equinus foot?
- How is this condition treated?
- Benefits of surgical treatment of an Achilles tendon rupture
- Achilles tendon rupture surgical treatment at 21st Century Medical Centre
Streptococcus equinus
Streptococcus equinus - Gram-positive, non-hemolytic, non-pathogenic lactic acid bacterium of the genus Streptococcus . (5) It is the most important Streptococcus in the gastrointestinal tract of horses [6] and makes up the majority of the bacterial flora in horse faeces. [7] The equivalence of Streptococcus bovis has been questioned. [4]
S equinus which is always abundant in horse manure, was first isolated from the air by Andrews and Horder in 1906, as dried horse manure was common in most towns at the time. [8th]
In 1910, Winslow and Palmer confirmed the findings of Andrews and Horder and reported further findings in bovine and human feces. [9]
phylogeny
After the discovery of the bacterium in 1906, the term Streptococcus equinus became a convenient 'garbage can' for non-hemolytic streptococci, which do not ferment lactose and mannitol. [9] Combining all streptococci that are unable to ferment lactose into one large category made classification very difficult S equinus .

Illustration 1. : Rootless tree showing some phylogenetic relationships of some species of Streptococcus . [10] .
However, it is known that, as shown on the left, S equinus , a non-enterococcal group D streptococcus, most closely related to the species S. bovis . [7] In 2003 it was found that. S. bovis i S equinus have a 99%ige similarity in the 16S rRNA sequences. [4] Although they are phylogenetically very similar, they differ in biochemical reactions and physiological properties. [4]
Taxonomy of Organisms Labeled. S. bovis i S equinus has a very complex history. Farrow et al. reported that S. equinus i S. bovis are synonymous. 1984, but were classified as separate species in the 'Bergey's Handbook of Systematic Bacteriology Listed in 1986. [11] More recently, the situation has been complicated by the description of two new strains originally identified as S. bovis. S. bovis than in reality S. caprinus , i C. gallolyticus . [11] Taxonomy of S equinus has not yet been fully clarified. [12]
The equinus foot - orthopedic problems
The equinus foot (pes equinus = horse's foot) is characterized by the fact that the heel cannot touch the ground when standing. The medical name comes from the fact that horses only walk on their toes, more specifically on the middle toe, which corresponds to the hoof. Toe walking is a serious problem for humans because all of the body weight falls on the front part of the foot. The foot does not roll when walking. The result is unstable posture and abnormal loading for which the feet are not anatomically prepared.
Equinus can be congenital or acquired.
The congenital equinus is usually based on a single malformation. Either the lower leg bones or the Achilles tendon are underdeveloped, or the unborn child was forced into this position in the womb.
In most cases, however, the equinus is acquired, that is, it does not develop until after birth. Various diseases can affect the nervous system, so a Lack of energy supply to the foot muscles Because the foot has to be turned around. If the nerve that supplies the calf muscle (nervus oculomotorius) is damaged, an equinus also occurs.
Diseases that affect the nervous system can also be paralysis cause. For example, after a stroke, hemiplegia often occurs, which can cause the foot to become unbalanced. A cerebral palsy, which z. B. caused by trauma or lack of oxygen during childbirth can be the cause of foot deformities.
In addition, other diseases can also cause equinus foot. An example is hemophilia, in which blood clotting is slowed down. Bleeding in the calf muscles can pinch the nerves, which can lead to paralysis.
B accidents or traumatic injuries The nerves that run through the calf muscles can become damaged. This can lead to equatorial foot, as can damage to the ankle or foot muscles.
Equine Foot Diagnosis
Equine foot can often be diagnosed with the naked eye. Examination of the muscles (electromyography), in which the electrical voltage is measured, helps to determine the muscular causes of the equinus foot. A radiological examination provides information about the extent to which bony structures are involved in the deformity. If necessary, a radiological examination of the knee and hip joints should also be carried out. You may already be suffering from the effects of an equinus position.
As a rule, every form of equilibrium position is treated. However, if the leg is shortened on one side, this does not have to be corrected.
The most appropriate treatment for each individual case depends on the severity of the deformity, the cause and the symptoms. There are conservative and surgical treatment options:
Non-invasive (conservative) treatment consists mainly of: physical therapy. Active and passive stretching of the shinbone attempts to relax the balancing foot and bring the foot into its normal position. If physical therapy is not sufficient for treatment, a tibial replication should be performed.permanent construction be created. With this plaster cast, the balance foot is gradually and gradually returned to its original position over a longer period of time.
If the conservative methods do not bring the desired success, surgical intervention necessary. The Achilles tendon is lengthened under anesthesia. After the operation, a plaster cast is put on for about four weeks to stabilize it. A night splint is then recommended to prevent regression. This treatment method is especially effective in children.
Surgical repair of joint stiffness (arthrodesis) may also be considered in adults with equinus foot. The upper part of the ankle is strengthened. The mobility of the ankle is maintained so that the foot remains mobile. However, this surgical procedure should only be performed when the articular cartilage has already been severely worn down by the equinus.
Doctors' and patients' opinions on the Jaquinus procedure
Both the doctors of the Yusupov Hospital and those of other institutions are positive about the use of Jaquinus. The drug's effectiveness has been observed in patients who have failed to respond to anti-inflammatory therapy, and a small percentage of patients have also been reported to experience side effects. According to the doctors' reports, no cases of overdose were observed in their practice. The doctors note that an unspecified indicator of inflammation, C-reactive protein, decreases significantly during treatment with Jaquinus and remains at the same level for two weeks after stopping the drug. The situation is similar with the pro-inflammatory immunoglobulins.
Patients who have been treated with Jaquinus also give positive feedback. They point to the convenient form of administration – tablets. The fact that taking the drug is not associated with food intake is also positive. Patients report satisfactory well-being, the effect is satisfactory, and the price of Jaquinus is satisfactory.
Analogues of Jaquinus - Azathioprine, Ecoral, Advagraf, Sandimmune, Leflunomide, etc. - have a different pricing policy, not quite identical composition, different country of manufacture (which can affect the quality), so the choice of drug is made together with the doctor should be consulted, taking into account his recommendations.
Yusupov Hospital provides diagnostic and treatment services for common and rare diseases in Moscow, 24 hours a day, with no weekends or breaks. The high qualification and professionalism of the doctors at the Yusupov Hospital makes it possible to treat 'difficult' patients, find solutions in desperate situations and make differential diagnoses between various diseases. The equipment of the Yusupov Hospital is modern, new and of high quality, which allows all instrumental and laboratory test procedures to be carried out as accurately as possible. The operators have a high level of competence, learning new techniques and carrying out each intervention automatically.
keywords
Jacobsen syndrome (JS) is a rare genetic syndrome caused by a partial deletion of the long arm of the 11th chromosome. JN belongs to a group of genetic syndromes characterized by multiple congenital anomalies in combination with delayed psychomotor development, visceral malformations and some orthopedic problems [1]. The syndrome was first described by Jacobsen in 1973 in several members of the same family who had inherited an unbalanced 11;21 translocation from a parent with a balanced translocation (1).
More than 200 cases of SN have now been described (2, 3). The incidence of SNF is 1 in 100,000 live births. The ratio of boys to girls is 2:1 (2-4).
The most common clinical features of SN are prenatal and postnatal physical and psychomotor developmental delays, characteristic facial dysmorphism, thrombocytopenia or pancytopenia. Patients present with cardiac, renal, gastrointestinal, genital, CNS, and/or skeletal malformations. Hearing and vision disorders as well as hormonal and immunological problems can also occur (2, 4).
The severity of the clinical symptoms is therefore variable. Cases have been described where PJD was accompanied by orthopedic pathologies such as flat foot, long toe, clinodactyly, brachydactyly, second and third toe syndactyly, and zygodactyly. It should be noted that the combination of clubfoot and congenital clubfoot is very rare. In the available literature, this pathology is mentioned only sporadically, and there are no data on the severity, methods and results of treatment.
Currently, the gold standard in the treatment of congenital clubfoot is the Ponseti method [5]. This method has revolutionized the treatment of congenital idiopathic and syndromic clubfoot [6].
In this publication we present our own clinical observation - a 2-year-old patient with SJ combined with congenital clubfoot.
case report.
A premature infant (weight 2870 g, height 50 cm, Apgar 7/7) was delivered at 38 weeks' gestation by cesarean section performed due to symptoms of imminent fetal hypoxia (amniotic fluid stained with meconium and no effect of labor). Initial examination revealed a moderate condition, congenital right clubfoot and clinical signs of grade II hypotrophy. In addition, numerous signs of dysembryogenesis were noted: low set ears, hypertelorism, high palate, transverse palatal ridges on both palms, cryptorchidism, underdevelopment of the foreskin and Divergence of the rectus abdominis muscle. Based on the above clinical signs, blood was drawn and sent to the genetic laboratory for karyotyping. The child was examined on day 2 of his life. An equinocavarus deformity of the right foot was found (Figure 1).

Figure 1: Patient's appearance before treatment
The severity was 5.5 points according to the Pirani system [7] (Table 1), 17 points according to the Dimeglio system [8] (Grade IV) (Table 2). Due to the patient's general severity, it was decided to defer orthopedic treatment until his condition improved. After that, there was frequent and severe belching. Therefore, the child was transferred to the surgical ward, where a duodenal obstruction was diagnosed. He was operated on day 12. The diagnosis of duodenal atresia was made. The clinical blood count showed a thrombocytopenia of 84 – 109/l. Genetic analysis revealed Jacobsen syndrome 46.XY, del(11)(q23)[18]/46.XY[2], a pathologic clone with deletion of 11q in 90 % of the metaphases (Figure 2).

Figure 2. Male karyotype, deletion of the long arm of chromosome 11 (locus 11q23)
symptoms of the disease

- Varus - Inward displacement of the foot in relation to the axis of the lower limbs.
- Plantar flexion, ranging from mild (heel slightly off the ground) to complex (supporting the metatarsophalangeal joints or arch of the foot).
- inward rotation of the toes.
- Absence of active bending movements.
The first changes can be seen by examining the footwear. The outer part of the shoe wears out much faster than the inner part.
With Equinus, the load on the foot becomes erratic and uneven, with the outer part of the foot bearing most of the load, reducing its cushioning function. Feet become heavy and painful, gait is unsteady, the patient has difficulty walking or jumping, and falls may also occur. If a limb is affected, a limp may be noticeable. The skin on the plantar, outer edge of the sole of the foot becomes thick and rough.
How the disease manifests itself
In most cases, the foot deformity has clear symptoms and can be detected by an external examination. However, since this part of the human skeleton is actively involved in movement, changes in its shape always affect the well-being and condition of the musculoskeletal system.
Aside from the external cosmetic blemish, different foot deformities can present the same symptoms:
- pain in the feet, ankles, knees and spine;
- Increased fatigability of the feet;
- disturbance of the gait pattern;
- Poor load distribution leads to incorrect posture and changes in shape of the feet;
- Calluses and corns appear.
Since the feet are in constant motion and have to withstand great loads, these deformations gradually progress. As a result, complications can develop: arthritis, bursitis, swelling, poor blood supply to the feet, curvature of the spine.
How does the drug Eliquis help?
Regular use of the drug is important for patients who are at risk for the following problems
- history of ischemic stroke;
- High blood pressure;
- chronic heart failure
- transient ischemic attacks;
- Diabetes;
- old age (over 70-75 years).
The drug is available in the form of film-coated tablets for oral use. The duration of treatment, dosage and frequency of treatment are determined strictly individually, depending on the indication. Please note that Eliquis has a fairly extensive list of contraindications, so treating this drug alone is dangerous.
Do you want to know more about analog medicines so you can choose the right drug for your budget? Our guide 'Popular analog medicines' from pharmacy experts will help you! It's very easy to get the guide: log in to our social networks and write 'analogues' in the message.
Mega pharmacy in social networks: VKontakte, Telegram, OK, Viber
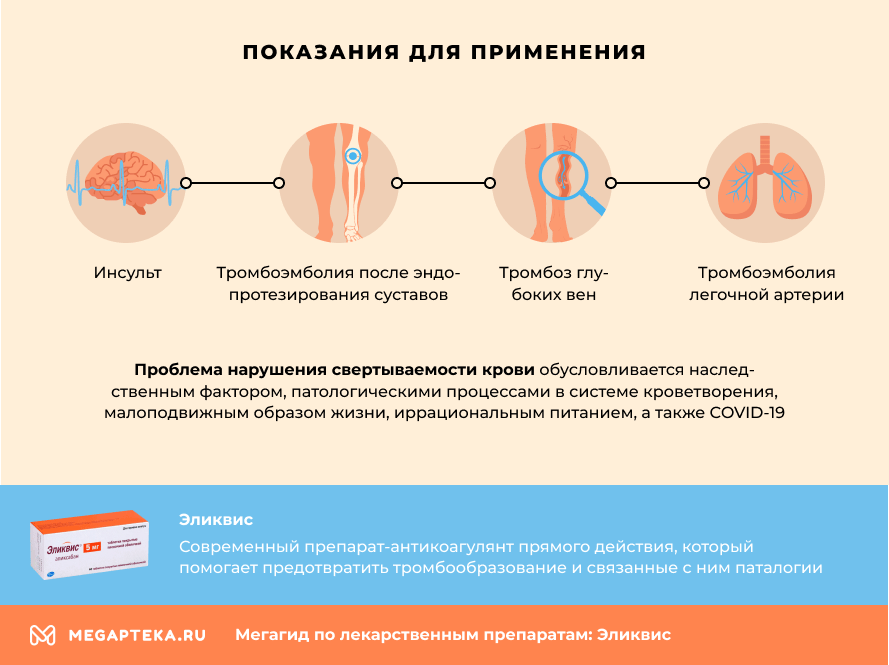
Contraindications to taking the drug Eliquis
- liver disease with blood clotting disorders,
- recent worsening of stomach or duodenal ulcers,
- malignant tumors,
- trauma or recent surgery to the brain, spinal cord, or eyes,
- recent hemorrhagic strokes,
- aneurysms,
- esophageal varices.
In addition, the drug is contraindicated in patients with impaired renal function and intolerance to the components of the drug.
'Eliquis' is not indicated in children and adolescents under 18 years of age and in pregnant and breast-feeding women - there are no data on its use in these groups.
Treatment of clubfoot (clubfoot)
The treatment strategy for clubfoot is determined by the podiatrist depending on the severity of the condition. Treatment should be as early, consistent and continuous as possible.
The result depends on the degree of clubfoot. In the case of mild clubfoot, the position of the foot can be corrected without surgery in 90% of the cases. A severe clubfoot can only be corrected conservatively in 10 % of the cases.
The conservative treatment of clubfoot begins in the first few weeks of life, because the bony structures of the child's foot are very soft during this time and the foot can be corrected without surgery.
Physiotherapy and foot massage are recommended. The foot is gently immobilized with flannel bandages. Once the foot shape is corrected, the child is fitted with a special splint. If the clubfoot is more severe, a cast is applied to gradually position the foot.
Later, children with clubfoot are treated with physical therapy, massage, therapeutic exercises, and orthopedic shoes. At night, special polyethylene splints are put on the feet.
If conservative correction of clubfoot is ineffective, surgery is performed. Surgical treatment is performed when the child is 1-2 years old and includes plication of the tendon, ligaments, and foot aponeurosis. In the postoperative period, plaster casts are prescribed for up to six months.
This article has no comments yet, you will be the first.
Treatment of equinovarus foot deformity
Equinovarus foot deformity treatment is a very lengthy and complicated process that requires a lot of effort and time. It is important to diagnose and treat equinovarus as early as possible, even in the earliest stages of equinovarus foot deformity development. Early diagnosis offers the best chance of a speedy recovery.
To make a diagnosis, Diagnosing and treating the cause of equinovarus foot deformity can only be done by an experienced podiatrist.. At the first signs of equinovarus foot deformity, you should immediately go to our Traumatology and Orthopedics Center, Clinical Hospital No. 85 of the Russian Federal Medicine and Biology Agency, for immediate medical assistance. Self-medication and folk remedies for the treatment of equinovarus foot deformity are strictly forbidden, since they can only relieve the pain for a while, but the deformity itself will continue to develop.
- Therapeutic physical exercises to correct foot shape and strengthen leg muscles;
- physiotherapeutic treatments;
- use of orthopedic accessories (correctors, supinators);
- use of orthopedic insoles and supinators;
- Comprehensive foot and leg massage including lumbar and gluteal massage.
In children, equinovarus deformity of the feet is very commonly treated with the Ponseti method. This is an internationally known technique that consists of manual correction and the gradual change of plaster casts. This method is very effective and guarantees minimal surgical intervention. With the Ponseti method, the equinovarus foot deformity can be corrected in just two months.
The main methods of treating equinovarus foot deformities in our orthopedic center:
- correction with a 3-point correction system;
- use of fixation prostheses;
- renewal of the foot surface;
- anti equinovarus shoes;
- Physiotherapy;
- administration of drugs to block neuromuscular conduction of the calf muscles;
- Surgical treatment (if other treatments fail).
What is equinus or equinus foot?
Equine foot is a curvature of the foot with a stable plantar flexion called equinus fitting. Equine foot often develops alongside other types of foot deformities. Manifestations of equinus pathology alone without other deformity components are relatively rare, accounting for 12.5 % of all possible deformities.

The equinus deformity is divided into two types:
- Congenital, meaning it is inherited genetically or develops during pregnancy, but is extremely rare;
- Acquired, caused by external or internal loads on the feet (as in gymnasts and ballet dancers).
Among the many factors that contribute to the development of deformities are:
- The development of flat feet (this is the most common cause);
- disruption of metabolic processes in the body;
- Significant weakening of the immune system and the body itself as a result of infections or inflammatory diseases;
- Endocrine disorders (thyrotoxicosis, diabetes, etc.);
- Inadequate absorption by the body of calcium and other substances and trace elements;
- Severe bone and joint diseases;
- any kind of injury or damage to the foot or the entire foot;
- tendency to be overweight or obese;
- hereditary or genetic predisposition;
- uncomfortable, too tight or ill-fitting footwear (narrow-cut models, high, unstable stiletto heels, etc.).

How is this condition treated?
Equinus foot deformity, treatment of the condition.
Equinus foot deformity treatment is a very lengthy process for the patient, requiring a lot of effort and stretching over a long period of time.
With this serious condition, it is important to make a correct diagnosis and start treatment right away – even in the early stages of equinus onset.

Timely diagnosis increases the patient's chances of a speedy and full recovery. Only an experienced podiatrist should diagnose the problem, determine the causes of the development of the equinus deformity and, based on a comprehensive examination of the patient, prescribe treatment.
Equinus deformity, in its milder forms, is treated with gymnastics, including specific foot exercises, foot massage, some physiotherapy treatments, the use of corrective splints, and the selection of orthopedic shoes. In more complicated cases, treatment is through the gradual application of plaster casts to the affected foot and shin, or through the use of a distraction-compression splint.
After surgery on the musculotendinous complex of the foot, the foot and shin may need to be immobilized in a cast for up to 46 weeks. After rigid immobilization of the ankle, the patient is prescribed a special complex of movements, therapeutic massage, hydrokinetic therapy (water aerobics) and physical therapy.
The operation can lead to a deterioration in leg function when the horse's foot has compensated for its length, since in such cases the compensation already formed is disturbed. Patients are advised to wear special orthopedic shoes to facilitate walking and gait.
Benefits of surgical treatment of an Achilles tendon rupture
In a study comparing surgical and conservative treatment, a decrease in the strength of the triceps muscle was noted: with conservative treatment by 38 % (with surgical treatment by 12 %), a decrease in strength by 36 % (with surgical treatment by 9 %). This is associated with a decrease in fiber tension of the triceps muscle on the shin.
The goal of surgical treatment of Achilles tendon rupture is to restore physiological tension to the triceps muscle with minimal surgical aggression. In general, the distance between the insertion of the Achilles tendon at the heel bone and the junction of the calf muscle with the tendon should be maintained for 6 weeks. During this time, the paratenon (tendon sheath of the Achilles tendon) forms a new Achilles tendon. In the rehabilitation phase, the collagen fibers can rebuild their complex internal architecture by increasing the movement correctly, without neglecting the rest of the musculoskeletal system.
Achilles tendon rupture surgical treatment at 21st Century Medical Centre
The 21st Century Medical Center typically uses a minimally invasive procedure to suture the Achilles tendon through an approximately 2 cm skin incision and 6 skin punctures. The operation is performed under nerve conduction (blocking the sciatic nerve with the long-acting anesthetic Naropin) and drug-induced sleep. This type of anesthesia is the most comfortable and safest for the patient, eliminates the pain in the first period after the operation and allows a good relaxation of the calf muscle, which is especially important in the case of 'non-refreshing' tears. Depending on the patient's condition and wishes, the operation can be performed under local anesthesia or with other anesthetics.
In most cases, the patient can leave the clinic 2 hours after the procedure. As with all surgical procedures, preoperative preparation is standard.
The postoperative period includes bandages, removal of stitches on day 12-14, and symptomatic treatment to reduce pain and swelling and prevent possible complications.
After the operation, a classic cast immobilization is carried out, which can be converted into a plastic immobilization on the 14th day after the threads have been removed. The knee joint is not immobilized.
From week 4, an articulating orthosis is fitted to bring the foot into a flexed position over a period of 2 weeks. After 6 weeks after the operation, the extremity may be loaded in a dosed manner.
In the early rehabilitation period, mechanotherapy with arthromotion, neuromyostimulation, and UWT is performed. After 8 weeks, physical therapy (exercise therapy, kinesitherapy) is the main method.
Once full range of motion is achieved, the crutches can be removed. The rehabilitation program is then based on the patient's own movement needs and sporting goals.
The average time to return to sport is 6-8 months, but this is an individual decision for each person based on an objective examination by a motor rehabilitation doctor.
Read more:- Balancing foot alignment.
- Equino valgus.
- equinovarus foot deformity.
- Clubfoot in 7-year-old children.
- Why does a child develop clubfoot?.
- What is clubfoot?.
- What to do if your child has clubfoot?.
- clubfoot.
