Scaphoid fixation is now considered the gold standard in the treatment of displaced fractures.
- Fractures of the heel bone of the foot
- Conservative treatment
- Flexible hypermobile flatfoot.
- Tarsal coalition
- Most cases of tarsal coalition fall into one of two types:
- clubfoot
- clinical picture
- Diagnosis and differential diagnosis
- Surgical treatment of hammertoe deformity
- postoperative period
- Two weeks after surgery
- Six weeks after surgery
- causes
- Symptoms of fifth toe deformity
- What is Keller disease type 2 or Freiberg disease?
- The course of type 2 Keller disease can be divided into four stages:
- Treatment
- Conservative treatment:
- Clinically Relevant Anatomy
- Epidemiology/Etiology
- nail leg
- Clinical Significance
- Horse anatomy
Fractures of the heel bone of the foot
The scaphoid is a key bone in the longitudinal arch of the foot. It is located at the tip of the longitudinal arch of the foot between the head of the talus and the three sphenoid bones. Its special anatomy makes it a kind of unique link between the hindfoot and midfoot.
The navel is a key bone in the longitudinal arch of the foot. It is located at the tip of the longitudinal arch of the foot between the head of the talus and the three sphenoids. The special anatomy makes this bone a kind of unique link between the hindfoot and midfoot.
The tendon of the tibialis posterior muscle attaches to the lateral surface of the navicular bone. This muscle supports the longitudinal arch of the foot. Dysfunction of the tibialis posterior muscle leads to flat feet.
The heel bone also serves as an attachment point for the various ligaments of the foot.
The ankle joint is covered with cartilage on almost all sides, so that the blood vessels only penetrate the bone in a few places.
There are four types of fractures of the heel bone:
Treatment for these fractures depends on the type and mechanism of injury and is discussed in more detail below.
A burst fracture is caused by forced plantar flexion of the foot.
This involves tearing a bone fragment from the scaphoid to which the taloclavicular ligament is attached. This fracture is the most common type of navicular fracture.
Statistically speaking, such fractures account for 47 % of all scaphoid fractures in the foot.
Patients with this type of fracture usually report acute pain and swelling in the foot, difficulty walking, and increased pain when flexing the sole of the foot.
Examination may reveal dorsal swelling, bleeding (bruising), and local tenderness of the navicular bone and/or the navicular oval joint.
Conservative treatment
Fractures of the heel bone can usually be treated conservatively.
In these cases, immobilization is recommended, although the type of immobilization may vary.
If the fragment is small, an elastic bandage may be sufficient.
If the fragment is larger or the patient cannot tolerate an elastic bandage for various reasons, immobilization with an orthopedic shoe or even a short plaster splint may be possible.
The duration of immobilization depends on the load capacity and the presence or absence of accompanying injuries to the metatarsal and collateral ligaments of the ankle joint.
Immobilization usually lasts 4 weeks, after which the load on the foot can be gradually increased as the load tolerance increases.
It must be recognized that this radiological classification is used only in Russia, primarily because of the excitement surrounding the draft. In the rest of the world, these angles are taken into account, especially when planning surgical treatment, but they do not constitute a classification of their own, since the angles on the radiographs and the degree of clinical manifestation have little correlation.
In terms of timing, a distinction is made between congenital (associated with developmental anomalies) and acquired forms of flat feet. Congenital causes include such rare and severe forms as congenital vertical talus and calcaneal valgus. The more common (1 to 6 % of the population) and less serious causes of congenital flat foot include calcaneal synostosis and some other synostoses, as well as bony outgrowths of the heel bone. Abnormalities in these bones result in abnormal load distribution in the gait cycle and overloading of the other stabilizers of the foot. In this case, the picture of flat feet appears between the ages of 8 and 15, due to ossification and the transition of the relatively flexible synchondrosis into a synostosis.
Depending on which arch of the foot is more involved in the pathological process, a distinction is made between longitudinal and transverse flat feet. Longitudinal flatfoot is primarily due to dysfunction of the pastern joint, heel wedge, supporting ligaments, and plantar fascia. Transverse flatfoot is associated with dysfunction of the thumb lever muscle and interdigital ligaments. In most cases, both longitudinal and transverse flat feet occur at the same time.
Depending on the clinical appearance, two main forms of flat foot are distinguished - the rigid and the flexible form. The flexible form only occurs when standing and disappears when lifting the toes or at rest. The rigid form remains at rest.
Flexible hypermobile flatfoot.
Currently considered a normal variant. It is characterized by a reduced height of the medial longitudinal arch at rest and a valgus position of the heel bone as well as abduction of the metatarsus during movement.

It is extremely common (20-25 % of the population). It is genetically determined and tends to run in families. It is often accompanied by hypermobile syndrome in other joints. In most cases, the severity of the deformity decreases with age.
Tarsal coalition
Children with tarsal coalition have abnormal bone fusion in the midfoot and hindfoot. The condition is usually diagnosed in pre-adolescence or early adolescence, when the bony adhesions begin to affect the mobility of the foot, causing pain and sometimes stiffness.
The symptoms are particularly noticeable when walking on uneven surfaces such as sand or gravel, when the foot constantly has to adapt to the unevenness of the ground. Frequent ankle sprains may also indicate a tarsal coalition.
Most cases of tarsal coalition fall into one of two types:
Talocalcaneus or subtalar coalition – a connection between the heel bone and the talus (in the ankle area).
- A talocalcaneal coalition is a pathological fusion of the heel bone with one of the bones of the foot - the heel bone.
The fusion can occur between two pieces of bone, between bone and cartilage or fibrous tissue. In about half of cases, the tarsal coalition occurs in both lower limbs. The primary treatment is conservative. The patient is recommended to protect and immobilize the foot.
Although this method relieves the pain, it only has a temporary effect. Conservative treatment is appropriate in patients with asymptomatic tarsal coalition (where the diagnosis is made only on radiographs, which are often incidental, such as in an ankle sprain).
Surgery is indicated for children with persistent pain that cannot be treated conservatively. During surgery, the orthopedic surgeon cuts out or removes the joint tissue. In most cases, foreign tissue - usually fatty tissue - is placed between the bones to prevent regrowth.
clubfoot
Clubfoot is a condition in which the foot - often both feet - is turned inward and the toes point downward. Clubfoot is diagnosed soon after birth. The condition occurs during the fetal development stage when the fetus is 9-14 weeks old.
It is often diagnosed during a routine ultrasound scan of the fetus. It is extremely important for parents to accept the facts and plan their next steps knowing in advance what to expect.
Clubfoot occurs in one in a thousand births and is more common in boys (births in Israel are best performed at Sheba Hospital). A family history can play a role, but it is common for children to live with clubfoot who have never had it in their family.
In most cases, treating clubfoot does not require surgery. The Ponseti method is used, which involves weekly gradual corrections and casts for the feet. Treatment should begin soon after birth as the infant's foot, with its tendons, ligaments and joint capsules, is the most deformable. After completing the first phase of treatment, long-term use of an orthopedic splint (tightly tied shoes) is recommended to consolidate the foot straightening achieved. Correct application of the Ponseti method produces excellent results. In some cases, surgical intervention is still necessary. The surgical method of clubfoot correction was widespread before the Ponseti technique became widespread. Surgical procedures are effective in correcting foot deformities, but the operated foot may develop osteoarthritis and stiffness later in life. Additional surgery is often required to relieve the pain caused by osteoarthritis.
clinical picture
In approximately 50 % of cases, the localized injury is preceded by severe posterior foot inversion.
Women over the age of 40 and younger athletes are most commonly affected.
- In the early stages (stage 1 or acute phase), patients often do not seek treatment because symptoms are mild.
- Patients typically present in stage 2 or the subacute phase, with diffuse swelling and fever in the medial aspect of the ankle and along the tendon path. Patients have difficulty or a feeling of instability when lifting the heel on the affected side, the heel does not supinate when lifted off the surface.
- In stage 3 or the chronic phase, patients notice a gradual decrease in the height of the longitudinal arch, the development of flat feet on one side, and fatigue of the lower limbs when walking. Viewed from behind, excessive abduction of the forefoot (symptom of too many toes) is noted. In severe cases: loss of the longitudinal arch, eversion of the heel bone. Excessive abduction of the medial part of the heel in footwear.
Diagnosis and differential diagnosis
The integrity of the posterior biceps tendon is assessed by palpation as the patient actively performs plantar flexion and adduction of the foot while the clinician applies a retraction force to the forefoot. It is important to accurately identify the area of damage within the tendon and compare it to the healthy foot. Direct pressure along the tendon path may reveal pain, active inversion of the foot against resistance may reveal reduced strength of the posterior biceps muscle. If the tendon is partially damaged, this can be determined by palpation.
If the tendon is completely damaged, it cannot be felt along its normal bearing and the patient cannot turn the foot against resistance.
Partial or complete damage caused by trauma is accompanied by various pains in the navicular tuberosity area. In strain injuries and tendon degeneration, pain occurs distal to the medial malleolus.
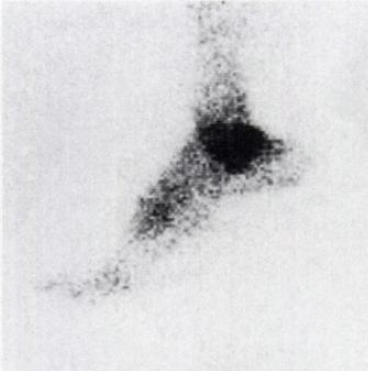
MRI is the most useful method for examining the tendons around the ankle and detecting tendon damage. Other diagnostic tests include bone scans and injection of a contrast dye into the tendon sheath.
Early diagnosis is not improved by a direct radiograph, but examination of the foot will reveal the extent of structural changes in stage 3. A standard anteroposterior radiograph shows an increase in the angle between the long axis of the talus and the long axis of the calcaneus, the anterior aspect of the foot and a displacement of the second metatarsal. The long axis of the forefoot no longer divides the angle of the rear foot in half. Under normal conditions, the linear relationship between ramus, navicular bone, medial sphenoid, and first metatarsal is lost on the lateral radiograph. As the situation progresses, osteoarthritis of the first metatarsophalangeal joint manifests itself as a result of the hallux limitus.
- Skeletal abnormalities:
- Scaphoid syndrome (Os tibiale externum), triangular bone syndrome, scaphoid tear, stress fracture of the scaphoid;
- osteochondritis or avascular necrosis of the ramus head or scaphoid;
- fracture of the medial malleolus;
- subacromial tarsal coalition;
- medial tarsal sinusitis;
Surgical treatment of hammertoe deformity
The surgical treatment of hammertoe deformity and the pain syndrome, the so-called metatarsalgia, pursues two important goals:
- Shortening osteotomies in the area of the heads of the metatarsal bones - the 'Weil' osteotomy.
- The 'harmonization of the foot', defined by careful preoperative planning and accurate measurement of the ball height during surgery to achieve the desired metatarsal length.
This operation is sometimes accompanied by the correction of a deformity of the first toe.


The extent of the surgical procedure depends of course on many other factors and characteristics of the respective patient.
postoperative period
During the postoperative period no plaster is applied No plaster immobilization is used.
After 1 to 2 days in an elevated position, the patient begins to walk with Baruca shoes - specially made orthopedic shoes with forefoot relief - with weight placed on the leg.


The duration of use of the special shoes depends on the individual, usually 4-6 weeks.
Particularly important are constant self-training (or with the help of relatives) in physiotherapy and constant passive movements of the operated toes in order to prevent possible stiffening.
According to medical statistics, 80-85% of patients who underwent surgery using the described method are satisfied with the result.
Two weeks after surgery
You will be examined by a doctor and a bandage will be applied. Once the wounds have completely healed, you will be explained how to massage the tissue in the area of the procedure. Measures to reduce the sensitivity of the scar begin only after the wound has completely healed. For this purpose, you can use a massage cream (e.g. E45) rubbed into and around the scar area. Only when the wounds have completely healed can you expose the surgical area to moisture and shower.
Once the swelling has largely subsided after the operation, you can stand your foot up more often, but you should keep it horizontal for as long as possible.
However, driving is only possible for a short time if you have had surgery on your left foot and your car has an automatic transmission. If you have had surgery on your right foot, you will not be able to drive until 6 to 8 weeks after the procedure.
At this stage, you may be referred to the physiotherapy department for early rehabilitation and exercises to strengthen the tibialis posterior muscle.
Six weeks after surgery
If the healing process goes well, the swelling and bleeding will now be virtually gone, but some swelling may remain for up to 3-4 months after surgery.
You can wear normal footwear during this time (swelling permitting), but we recommend that you wear stiff-soled shoes for the time being. You will need to undergo physical therapy over the next 3 to 6 months to achieve the best possible outcome from the surgery.
causes

There is a long list of factors that can cause Taylor deformity. This includes:
- Congenital foot characteristics or an inherited tendency to develop certain orthopedic disorders such as flat feet, abnormal adduction and extensor muscle fixation, hollow feet, etc.
- Fifth toe abnormalities, including dumbbells, hammertoes, extra bones, abnormal curvature, etc.
- Habit of sitting in a crossed position for long periods of time.
- Prolonged wearing of uncomfortable, tight, small shoes or shoes with heels or platforms that are too high.
- Flat feet, especially those that remain undetected for a long time and are therefore not corrected.
- New growths on the foot near the 5th metatarsal.
- Neurological diseases, especially cerebral palsy, meningitis, lederhosen contracture, etc.
- Fractures of the 5th metatarsal that have not healed properly, injuries that have led to weakening of the musculoskeletal system, tendon overloads and other abnormalities that affect the anatomy of the foot.
Symptoms of fifth toe deformity

Tailor's foot can cause significant discomfort and difficulty both at work and at home. It is characterized by:
- an annoying, often throbbing pain that occurs and increases when walking and exercising (it can become bothersome and cause limitation in physical activity);
- annoying pain of mild to moderate intensity, even at rest and at night while sleeping;
- discomfort in the foot due to widening of the transverse arch;
- Difficulties in choosing footwear, since in the later stages the formation of callus, especially in combination with the presence of a similar but reflective callus on the big toe, makes wearing normal footwear impossible;
- Pain, swelling and redness of the soft tissues in the projection of the inflamed ankle joints;
- Ulcers and fluid accumulation in the area of the protruding bone on the lateral surface of the foot caused by the bone rubbing against footwear;
- The formation of calluses and corns on the sole of the foot caused by the lateral spread of the foot.
What is Keller disease type 2 or Freiberg disease?

Keller disease type 2 or Freiberg disease is a relatively rare, non-infectious disease and belongs to the group of osteochondropathies. The head of the metatarsal bone begins to break down and die as a result of circulatory problems for one reason or another. In 95 % cases, the heads of 2 or 3 metatarsals are affected, although aseptic necrosis cannot be ruled out in the others.
Although the disease was recognized and described more than 100 years ago, little is known about it to this day.

The tarsal bones are a group of 5 long bones located in the metatarsal. They connect the phalanges of the toes to the back of the foot. The heads of the metatarsal bones form the metatarsophalangeal joints with the distal phalanges of the toes, which enable the movement of the toes and the maintenance of normal support function. Aseptic necrosis of the head of the second metatarsal bone occurs most commonly in adolescent girls between the ages of 10 and 15 years. This is the age at which it is most often discovered. However, Keller disease type 2 does not appear for the first time in adults, although it is often diagnosed in cases where appropriate treatment was not given in youth. However, there are case reports of the disease occurring in 20 to 25 year olds, but these require further investigation.
The course of type 2 Keller disease can be divided into four stages:
- Aseptic necrosis. This stage is characterized by the destruction of the bony ridges in the bone that provide strength, ie the development of local osteoporosis. As a result, the affected metatarsal head loses its density and is no longer able to withstand the loads placed on it.
- Compression fracture – results from the destruction of part of the remaining bone beams within the head or newly formed bone beams. This causes them to break off, wedge into each other and drastically reduce the height of the bone.
- Fragmentation or resorption. Changes in the metatarsal bone lead to the formation of osteoclasts (special cells that resorb damaged bone bodies). This leads to a reduction in the size of the head and even its almost complete resorption.
- Recovery and consolidation. The body attempts to repair the damage by attempting to rebuild the lost bone. As a result, the metatarsal head gradually rebuilds itself, but this is often difficult because it is severely deformed by the resulting pathological fractures and defragmentation, and the repair process itself requires a good blood supply, which is not present if Keller's disease is not treated .
Treatment
The prognosis of Keller disease is very favorable, especially if it is diagnosed and treated early. If this is the case, patients have every chance of getting rid of the excruciating pain in the foot and the need to limit physical activities.
The type of treatment largely depends on the stage of the disease, the presence of complications and the patient's age. While conservative treatment is sufficient in the early stages, surgical intervention may be necessary in advanced cases.
Conservative treatment:
- Immobilization of the foot with a plaster cast in the shape of a boot for a period of 4-6 weeks. In particularly difficult cases, immobilization can be extended to 12 weeks. During this time, mobility is ensured with the help of crutches.
- Wearing orthoses. They help to correctly distribute the load on the foot and eliminate movement abnormalities. They eliminate the symptoms of the disease and dramatically reduce the risk of complications. However, to be effective, they must be made individually for each patient.
- Pharmacological treatment aimed primarily at eliminating the symptoms of the disease, especially pain, by taking NSAIDs and improving metabolic processes in the foot. Therefore, additional preparations are prescribed that activate calcium metabolism and improve peripheral blood circulation. In this way, an attempt is made to influence the causes of the disease.
- Physiotherapy, which includes massage, magnetic therapy, electrophoresis, iontophoresis, laser, shock wave therapy, foot baths, etc., is also used. The aim of these treatments is to improve blood circulation in the feet, eliminate inflammation and reduce pain. Physiotherapy is very effective against Keller's disease.
- Physical therapy – exercises individually tailored to the patient that improve local blood circulation, increase the amplitude of movement of the big toe joint, strengthen the foot muscles and prevent the development of flat feet.
Clinically Relevant Anatomy
During human embryonic development, the shaft and posterior processes of the talus form separate ossification centers. Between the ages of 7 and 13, the posterior process of the talus forms a separate bone (triangular bone). However, within a year of its appearance, it reunites with the talus (this does not happen in 7 % of affected individuals). It can occur on one or both sides. It has smooth or jagged edges. The size is less than 1cm but may vary.
Georgy Temichev's seminar 'Diagnosis and treatment of problems of the lower limbs. Gait and running analysis'. Learn more…
This bone usually has three horns, anterior, inferior and posterior surfaces. The anterior surface is connected to the lateral cusp via a cartilaginous synchondrosis. The lower surface can be articulated with the heel bone. The posterior surface has no articulation, but serves as an attachment point for the ligamentous structures of the capsule. The triangular leg can also have a round or oval shape.
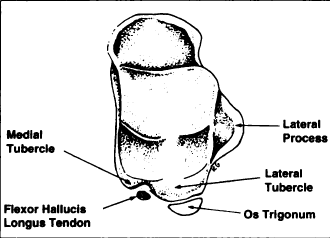
The flexor tendon of the thumb is located medial to the triangular bone in the groove between the medial and lateral cusps.
Epidemiology/Etiology
There are 3 mechanisms of triangular bone formation:
The presence of SCC can be caused by overuse or trauma (e.g. in ballet dancers or track and field athletes). The strong flexion of the plantar muscle, which occurs when standing on tiptoe or half-toe and when running downhill (track and field athletes), puts pressure on the back of the ankle joint. The triangular bone can shift as a result of forced flexion of the sole of the foot caused by trauma.
The soft tissue structures, including the ankle joint capsule and surrounding ligaments, may be stressed by such movement/stress and painfully increase in size (hypertrophy).
nail leg
The navicular bone is a small bone in the feet of most mammals.
In humans, the navicular bone is one of the tarsal bones of the foot. Its name derives from the resemblance of this human bone to a small boat, caused by the highly concave proximal articular surface. The term navicular bone or carpal bone was previously used for the navicular bone, one of the bones of the wrist.
In humans, the navicular bone is located on the medial side of the foot and connects proximally to the talus bone, distally to the three sphenoid bones and laterally to the elbow bone.
It is the last of the foot bones that begins to ossify, usually at the end of the third year of life for girls and at the beginning of the fourth year of life for boys, although a wide range of variations has been found.
Calcaneus. View from above.
The pastern bone. View from below.
 Fracture of the heel bone
Fracture of the heel boneThe tibialis posterior muscle is the only muscle that attaches to the heel bone. The main part of the muscle enters the tuberosity of the scaphoid. An extra ankle joint can occur in 2-14 % of the general population.
Clinical Significance
The human navicular bone is not usually a broken bone, but it does occasionally break for two reasons. The first mechanism is a stress fracture, which typically occurs in athletes, and the second mechanism is high-energy trauma. The scaphoid is the cornerstone of the foot: it is part of the foot pelvis and is connected to the talus, the first, second and third sphenoids, the ankle and the heel bones. It plays an important role in the biomechanics of the foot by supporting inversion, eversion and movement; it is the structural link between the midfoot and forefoot and part of the longitudinal and transverse arch of the foot.
Horse anatomy
The horse has a sesamoid bone, the so-called navicular bone, which is located inside the hoof and lies on the inside of the coffin joint between the second and third phalanges (coffin bone). The horse's navicular bone is supported by the distal metacarpal ligament and two lateral metacarpal ligaments. The pocket of the tarsal joint is located between the flexor side of the articular bone and the deep flexor tendon of the fingers, which passes between the pocket and the distal phalanx. The middle tarsal bone in the horse's hip joint is homologous and similar to the navicular bone of the human foot, so the horse's navicular bone has a different structure than the human toe labial bone.
The navicular area is an important structure in relation to lameness, particularly in the forefoot, and is involved in a significant pain process called navicular disease or navicular syndrome. Much of the original literature on scaphoid disease has recently been questioned, particularly the importance of radiographic changes as the sole diagnostic criterion. Scaphoid syndrome may account for up to a third of all cases of lameness in horses, but radiographic changes in the scaphoid do not always allow a definitive diagnosis. New imaging techniques have shown that soft tissue damage in this area can be a significant contributing factor to lameness and that multiple causes can lead to visible lameness.
- Pain in the heel bone of the foot.
- scaphoid in the foot.
- metatarsal bones.
- heel bone injury.
- Fracture of the calcaneus of the foot.
- The tarsal of the foot.
- Anatomy of the heel bone x-ray.
- Fracture of the heel bone.
