The Ponseti method was proposed by the orthopedic surgeon Ignacio Ponseti in the USA in the 1940s. In Russia it was used only 18 years ago. Before that, other techniques of home treatment according to VJ Vilensky, TS Zatsepin and others were used. This included long casts of 6 to 12 months, extensive surgery, casts again, and heavy shoes at the end. After all these procedures, the child was classified as disabled. The feet were more or less straightened, but mobility was limited and the patient usually had painful walking and running difficulties and difficulty finding the right footwear.

- clubfoot
- Possible causes
- Purpose of clubfoot training
- Principles of exercise therapy
- Treatment of congenital clubfoot in newborns
- Support for the 'Towards Life' project.
- Our patients
- Anastasia
- Miroslav
- Alexander
- Maria
- Filipp
- What does the Ponseti plaster treatment involve?
- 1. Plasters
- 2) Achillotomy
- 3. Stiffening
- Clubfoot at the age of 1 year
- Treatment of clubfoot in children in the first year of life
- Metatarsus adductus and Metatarsus adductovarus
- Internal rotation of the lower limbs
- Where can I buy orthodontic braces? Are they made in Russia?
- Do I need to see a doctor after my Ponseti treatment?
- What is the disease?
- Causes of Clubfoot
- Congenital (clubfoot in newborns)
- Acquired clubfoot
- Pediatric massage at home for clubfoot: features
- Also read:
clubfoot
Clubfoot in children is a common musculoskeletal abnormality. It manifests itself in a deformity of the foot, an abnormal physiological alignment of the heel bones and limited mobility of the ankle joint. Externally, the defect looks like a curvature in which the outside of the foot, the sole part upwards, and the toes bend inward. The disorder occurs in one foot or can be bilateral. It is caused by abnormalities in soft tissue and bone development resulting from a variety of causes.
Treatment for clubfoot in a child depends on the type and severity of the condition. The abnormality is:
- Congenital, recognizable already in the womb.
- Acquired by trauma or disease, the course of which affects the treatment of clubfoot in children with this condition.
- Typical, usually not extending beyond the limits of the foot, caused only by the development of the muscles.
- Atypical, caused by diseases of the central nervous system and severe diseases of the musculoskeletal system.
There are three levels of difficulty when deciding how to correct a child's clubfoot. The first is varus contracture, which is painless and can be corrected manually. The second stage is the soft-tissue mold, when the child does not fully plant the leg on the floor, and the tissues resist manual correction. The third stage is a musculoskeletal form with permanent changes and a limitation of joint mobility, when treatment of clubfoot in children with conservative methods is impossible. In very difficult cases, especially those over 2.5 years of age, clubfoot requires tendon grafting.
Possible causes
In newborns, the condition is often due to mechanical causes, such as B. Lack of water or misalignment of the fetus during the mother's pregnancy. The increased pressure causes the walls of the uterus to press the legs more tightly against the fetus. Not infrequently, clubfoot is caused by neuromuscular abnormalities in fetal development:
- abnormalities caused by avitaminosis;
- lack of nerve fibers;
- abnormalities in the formation of muscles and ligaments in the first few weeks of fetal life;
- Toxicosis caused by the use of drugs by the mother during pregnancy.
If a parent had clubfoot as a child, the child's developmental abnormality is due to a hereditary factor. The question of how to correct clubfoot has a genetic basis - a tripling of a pair of chromosomes (Edwards syndrome) leading to clubfoot. If the question of how to correct a clubfoot is not considered, musculoskeletal problems can arise later: through incorrect foot support, increased strain, weight gain, wearing unsuitable shoes, after injuries, leg diseases. In the treatment of clubfoot in children, the cause of its formation has little influence, the main thing is to eliminate the pathology in time.
Purpose of clubfoot training
Clubfoot of varying degrees is diagnosed in nearly 12 % of the infants. It has been proven that congenital clubfoot can result from a genetic predisposition or from excessive mechanical stress on the lower limbs of the fetus during intrauterine development associated with malnutrition or malposition. Clubfoot acquired at a young age occurs in about 3-5 % cases and usually develops after trauma or certain infectious and inflammatory diseases. The anatomical anomaly leads to a permanent foot deformity: the soles of the feet turn inward, a thickening occurs in the middle of the foot, and the volume of the lower limbs is significantly reduced.

This is not painful for the child, but is associated with restricted mobility of the ankle and a change in the gait pattern. In severe cases, clubfoot can lead to disability if left untreated. The main treatment method is exercise therapy, the main goals of which are.
- Restoring mobility and the physiological structure of the foot;
- normalization of muscle tone in the lower limbs;
- prevention of muscle wasting in the lower limbs and thighs;
- Activation of local blood flow and tissue nutrition.
Warning.
If congenital clubfoot is diagnosed, therapy must begin in the first few days of life. As the child gets older, their musculoskeletal system becomes less flexible and supple, and it takes much longer to recover the natural foot position.
Principles of exercise therapy
The following rules should be observed when performing clubfoot exercises in children of all ages:
- The exercises are required at least 5-6 times a week. The duration of work with each foot is 5-7 minutes for newborns, at least 15-20 minutes for school-age children;
- All movements should be smooth and painless. In case of discomfort or fatigue, a break should be taken;
- Classes for children of all ages are conducted barefoot. Thin socks can be worn;
- Clubfoot exercises should be performed after heat treatment (bath or shower, warming compress). It is advisable to end each session with an intensive foot massage using oil or a special cream. After exercise, hypothermia should be avoided and feet should be warmed with woolen socks or tights;
- To increase the effectiveness of treatment, training should be combined with physical therapy, swimming, sports and wearing orthopedic shoes as recommended by a doctor.
Treatment of congenital clubfoot in newborns
Traditionally, a combination of conservative and surgical procedures is used to correct clubfoot. Both therapies require a lot of physiotherapy, physical therapy, and massage and can last into adolescence, but do not guarantee complete correction of the condition. A child with restricted mobility will develop an irregular gait in adulthood. If the problem of effective treatment of the right and left clubfoot is not addressed in time, the limb will shorten.
The Ponseti method is becoming increasingly popular and results in a complete cure in 80-90 % of cases. It is used to start correcting foot deformities in children as early as the first few months after birth. The Ponseti method divides all phases of the treatment of congenital clubfoot into three stages:
- Correction with plaster casts (4-8 bandages depending on the complexity of the deformity).
- Minimal traumatic passage of the Achilles tendon to lengthen it.
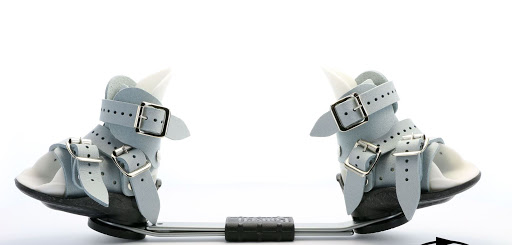
- Maintaining the correction/treatment by wearing orthopedic shoes (braces).
Support for the 'Towards Life' project.
If you have an ultrasound, knowing in advance that your child will need treatment for congenital clubfoot, you will have a good time leading up to your child's birth. Even before the birth of your child, you can decide on a pediatric orthopedist who treats congenital clubfoot using the Ponseti method, who has experience in dealing with similar problems, and on the medical facility where the doctor will carry out the treatment. Talk to parents of clubfoot sufferers on forums. If you are convinced that it is possible to get rid of clubfoot without consequences, come to our clinic. We help your child gently and effectively to get well and to overcome one or two-sided clubfoot.
As part of the 'Towards Life' project, you will receive help from highly qualified doctors. They have mastered the advanced Ponseti technique, which almost completely rules out relapses. Many children around the world and in Russia have already been cured with this method. The treatment is free! For an appointment and if you have any questions, we look forward to your call 8 (800) 555-84-21 Weekdays from 9 a.m. to 7 p.m. (Moscow time).
Our patients
Anastasia



Diagnosis: Congenital bilateral severe atypical clubfoot
Treating doctor: Maxim Vavilov
Miroslav



Diagnosis: Congenital bilateral severe clubfoot
Treating doctor: Maxim Vavilov
Alexander



Diagnosis: Congenital right-sided severe clubfoot
Treating doctor: Maxim Vavilov
Maria



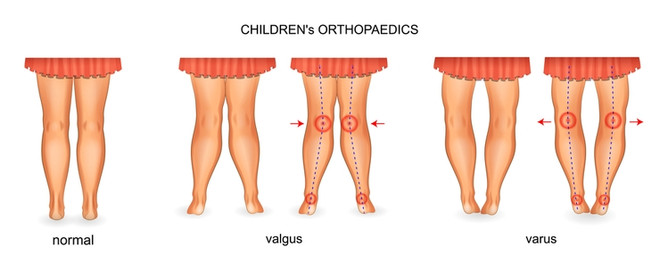
Diagnosis: Congenital bilateral valgus
Treating doctor: Maxim Vavilov
Filipp



Diagnosis: Congenital bilateral valgus foot
What does the Ponseti plaster treatment involve?
The currently most important and internationally recognized method for the treatment of congenital clubfoot is the Ponseti plaster method.
This method was developed in the 1940s by Ignacio Ponseti, an American orthopedist (University of Iowa, USA).
This method is even suitable for late treatment in early childhood. Surgical correction is required in most cases, but is less extensive than would be the case without the Ponseti cast.
Clubfoot treatment with the Ponseti method is a simple and straightforward method, but it requires a clear sequence of corrections and steps.
1. Plasters
It all starts with a plaster cast. Taking into account the correction of the deformity, a plaster of paris is glued to the child's leg. The cast is changed once a week. During this time, the tendons, muscles, ligaments, and joint capsule are stretched. With each additional plaster cast, the misalignment is corrected even more. On average, five plaster casts are required. By this time, forefoot adduction, supination, and heel bone alignment are usually corrected.
2) Achillotomy
Once the bandages are in place, dorsiflexion remains an issue. In 75 % children, the equinus remains or the foot is only extended to a dorsiflexion of 90° (extensio). In such cases, an achillotomy is recommended. This is a mini-surgical procedure in which the Achilles tendon is severed subcutaneously. The aim is to lengthen the Achilles tendon and thus reduce its pathological effect on the heel bone.
After the achillotomy, the heel eventually returns to its normal position, the calcaneus tuberosity is lowered (it can now be felt) and dorsiflexion of the foot is possible. Another plaster cast is applied, this time for three weeks. After this time, the next stage can be started.
3. Stiffening
Clubfoot at the age of 1 year
Both congenital and acquired forms can be diagnosed from 0 to 12 months of age. The former are often detected during fetal development, and treatment is initiated after birth on the doctor's recommendation.
Acquired defects are diagnosed after 4 months of life (before that, the inward and upward arches of the foot may be normal). The diagnosis is often made just before the child begins to walk independently. It is better if the foot is able to walk again before taking the first steps.

Treatment of clubfoot in children in the first year of life
Depending on the severity of the disease, treatment can be conservative or surgical, with the latter being a combination of both methods. In mild to moderate cases, the mobility of the ankle is not or only slightly restricted. Restoration of foot function and shape can be improved with comprehensive treatment.
- Massage.
- Corrective exercises for 5-7 minutes.
- Manual therapy.
- Gentle bandaging according to the Fink-Ettingen method consolidates the results achieved with passive exercises and manual therapy.
- In the case of a moderately severe lesion, the treatment is carried out according to Ponseti. A plaster cast is placed on the leg at intervals of 5-7 days. Each stage causes a small change, fixing the leg in a new position until the anatomical norm is reached.
- Wearing orthotics - devices in the form of shoes that affect the position of the sole - is effective. For example, an orthosis is a pair of shoes with a metal plate in between. It fixes the physiologically correct position of muscles, joints and ligaments and does not allow the child to voluntarily change them.
Metatarsus adductus and Metatarsus adductovarus
These are two very similar conditions where the forefoot points inward with a tight heel. The first condition is believed to be caused by increased activity of the dorsal flexor muscle of the thumb and most commonly occurs between the ages of 0-18 months. The second form (where the plantar surface of the forefoot also points slightly inward) is thought to be caused by the pressure of the uterine wall on the foot in the fetal position. They usually correct themselves spontaneously before the age of 3-4 months.
What these disorders also have in common is that they do not require any special treatment and usually end in self-righting of the foot. They are easily distinguished from the conditions associated with congenital bone and muscle abnormalities because they are easily erected with gentle pressure with one hand and then brought into what is known as hypercorrection.
Internal rotation of the lower limbs
In internal rotation of the tibia, the tibia (which has a supporting function) is rotated slightly inward about its axis. When the child is seated on the edge of a chair and allowed to hang down, the ankles are turned in together with the feet and the knees are 'straight'.
In the history of orthopedics, treatment ranged from systematic changes in foot position during sleep to orthopedic shoes and surgical interventions (derotational osteotomies). However, it has been shown that internal rotation occurs in most healthy children during the first year of life and spontaneously corrects as the child grows.
Where can I buy orthodontic braces? Are they made in Russia?
When the Ponseti method was introduced in Russia, at first you could only buy braces made abroad. However, it did not take long for Russian orthodontic companies to launch analogue products. To date, Medvezhonok is the leading manufacturer of high-quality orthodontic braces in Russia. But in general, I can highlight several models on the market: Mitchell (UK), Alfa-flex (Germany), Kinetic Pro (Russia). Braces for every taste and budget, so to speak. It should be noted that more and more patients are choosing the native Bear braces, especially the latest Kinetic Pro model. Good quality, affordable price - all arguments speak for it!
Do I need to see a doctor after my Ponseti treatment?
A responsible and important period begins immediately after the plaster cast. Parents must follow the prescribed track system to prevent relapses and come for check-ups every 2-3 months at first and then twice a year. These visits are like a feast for the parents as we assess the treatment and shorten the time the brace is worn, giving the child more freedom.
After treatment, the child should wear the orthosis and come for regular follow-up visits until the age of 4-5 years.
What is the disease?
A foot deformity can be congenital or acquired. The former occurs during fetal development. Possible causes are:
- Bad habits of mother - alcohol, smoking, drugs;
- work in a harmful occupation;
- malnutrition, vitamin deficiency;
- Incorrect positioning of the fetus;
- low water content;
- abnormal bone development;
- spinal nerve abnormalities;
- toxoplasmosis;
- hip dysplasia;
- Genetic Disorders.
Congenital clubfoot has mild, moderate, and severe symptoms. The first two are often not recognized during the infant's initial examination, while the second form, characterized by twisting of the tibia, is immediately apparent. Parents should pay attention to the foot is too short, there is a transverse groove in the sole, the toes are turned inward, and the tissue is swollen.

Causes of Clubfoot
Acquired clubfoot develops during the growth of the child under the influence of various factors:
- Trauma, burns, tumors of the bones, muscles and ligaments;
- complications after infectious diseases;
- paralysis due to neurological problems;
- Bone growth disorders of the lower limbs and foot;
- Injuries, diseases of the spine;
- Rickets;
- Poliomyelitis;
- uncomfortable shoes;
- overweight.
Clubfeet acquired in children are much less common and easier to correct. If a child has a shaky foot, hobbles, gait, and knees turning inward, parents shouldn't put off going to the podiatrist.
Early detection of a congenital foot defect is crucial to correct it. When a child starts to walk, the bones are soft and flexible and can be easily corrected. As the child gets older, there are profound changes in the foot that are very difficult or impossible to correct.
Clubfoot can be detected in babies in the womb with an ultrasound scan of the fetus. If the neonatologist suspects clubfoot during the initial evaluation of the newborn, they will refer the child to an orthopedist. He will assess the mobility and position of the joints and recommend a comprehensive examination. The clubfoot should be corrected under his guidance and supervision.
Acquired clubfoot develops in children between the ages of 3 and 14 and is almost asymptomatic in the early stages. At the first worrisome symptoms, a comprehensive examination is urgently needed, including:
- X-rays of the ankle and foot to determine the degree of deformation of the bones and joints;
- General blood and urine tests – important for assessing the child's condition.
Congenital (clubfoot in newborns)
The dysplasia is already visible in the sixteenth week of fetal development by means of an ultrasound scan. The neonatologist can also identify signs of dysplasia after the baby is born. The main signs include:
- Equinus, in which the outside edge of the foot is lowered and the inside is raised. The back faces the other foot.
- Varus deformity of the foot. The child leans on the outer edge of the foot.
- Torsion - the bones of the lower limbs are twisted outwards.
- The most severe case is adduction, where the foot is completely inverted and sole-pointing up.
Acquired clubfoot
Clubfoot can develop in a child if the abnormality is ignored:
- The skin of the buttocks and feet of the child is unevenly and symmetrically corrugated.
- The position of the upper limbs when walking - the arms are raised.
- The child cannot sit up or rise from a crouch without using their arms to support themselves.
These symptoms indicate the presence of swelling in muscle tissue. The swelling of the proteins prevents the muscles from contracting normally.
Symptoms of clubfoot in a healthy child may appear in the second or third year of life. They usually look like this:
- Irregular gait (bear gait) – when walking, the child 'waddles' with one leg.
- When the child walks, they do not put their feet down properly. This can be seen from the footprints left by the child. The footprint of one foot is always turned to the other.
- The knees point inwards – towards each other.
- Limited mobility of the ankle.
- Abnormalities may be visible when the child is asleep.
- The big toe points inward: a valgus curve where a specific thickening occurs on the inside of the foot.
The progression of the disease is due to increasing swelling caused by stress on the muscle groups of the lower back, buttocks and lower limbs. In children, the skeleton grows rapidly, but since the muscle tissue cannot function normally, the Muscles begin to pull on the bones.. Because of this, the joints cannot be fully flexed and extended.
Because of this, some muscle groups are severely swollen (hypertonic) while others are completely relaxed. All of these factors manifest themselves in the form of a flat foot.
Pediatric massage at home for clubfoot: features
Stroking, rubbing, stretching with vibration, slow kneading are used to relax the internal and posterior muscle groups of the lower leg, where there is increased muscle tension.
The following techniques can be used to strengthen the stretched and weakened muscles of the front and outer muscle groups of the lower leg: vigorous rubbing and kneading, possibly light tapping with the fingers.
It is advisable to do special exercises after heat treatment.
- The child is lying on his stomach. Bend the child's leg at the knee joint; hold the lower leg with one hand, and with the palm of the other hand, slightly press the child's foot, bending it backwards (to stretch the Achilles tendon and eliminate the flexion of the sole of the foot);
- Try doing the same. The child is lying on its back. One hand presses the child's shins against the table surface, pinning them at the ankles. The palm of the other hand rests on the sole of the foot and gently bends the foot backwards while pressing on the outer edge of the foot. Combine this with a massage of the pressure points at the transition between the dorsal and shin bones.
- To eliminate forefoot adduction: One hand holds the child's foot by the ankle and the other hand makes gentle stretching movements, gradually pulling the forefoot outward.
- Turning the foot outward (very gently along the longitudinal axis, gradually lowering the inner edge of the foot and raising the outer edge).
With mild clubfoot, fixation with bandages is carried out after Massage and exercises for clubfoot (The bandages should be changed 3-4 times a day, and passive corrective exercise and a 5-minute light massage should be done each time). The mother puts on the bandages and the masseur massages and checks the condition once a day. It is good to do this immediately after sleep or heat treatment (bath at 37-38 degrees). (Banding with doctor's approval).

Also read:
If you found this article interesting, please share it on social media, maybe someone else will find it useful. Moms always have a lot of questions, let us help them find the answers!
Natalia G. Rostov-on-Don
Alexey Matrosov
Hello, if the bony form of clubfoot, then no. If the child simply rolls the toe inward when walking, then at the age of 7 one can still try to correct it. The child is already a big boy and if he had a congenital clubfoot, the body has already adapted to the problem. It is useful to massage the foot and lower leg muscles to keep them functional. With a clubfoot, the leg muscles work with different loads.
Another
Hello, our child was born with bilateral clubfoot. It was successfully fixed with the help of a cast. However, one leg does not want to come off completely. The child tiptoes. Is it possible to massage them independently? The child is afraid of people in white coats. Thank you
Masseur Alexey Matrosov
Hello, without practice you will not be able to massage yourself. You need to try a massage from a professional and if that doesn't work you might need to redo the cast, that helps a lot, the most important thing is to keep the leg in the right position. The masseur does not have to wear a white apron, there are now colorful uniforms for paediatricians, or he does not wear medical clothing.
Read more:- The Ponseti method.
- Congenital clubfoot.
- What is clubfoot?.
- Why does a child develop clubfoot?.
- Ponseti breeches.
- Clubfoot in 7-year-old children.
- clubfoot.
- Clubfoot Treatment.
